-
摘要: 急性局灶性细菌性肾炎(acute focal bacterial nephritis,AFBN)是一种细菌感染引起的肾实质局灶性非液化坏死性炎症,特征是影像学表现为肾脏占位性损害,极易被误诊为肾肿瘤。本文报道淄博市中心医院近年收治的1例AFBN患者被误诊为左肾肿瘤合并泌尿道感染,后经抗感染治疗痊愈。
-
关键词:
- 急性局灶性细菌性肾炎 /
- 泌尿系感染 /
- 肾肿瘤
Abstract: Acute focal bacterial nephritis (AFBN) is a bacterial infection that causes focal non-liquefied necrotizing inflammation of the renal parenchyma. It is characterized by space-occupying lesion of the kidney, so is easily misdiagnosed as renal tumor. This paper reports a case of AFBN patient admitted to Zibo Central Hospital in recent years who was misdiagnosed as left kidney tumor complicated with urinary tract infection and recovered after anti-infection therapy.-
Key words:
- acute focal bacterial nephritis /
- urinary tract infection /
- renal tumor
-

-
[1] Mizutani M, Hasegawa S, Matsushige T, et al. Distinctive inflammatory profile between acute focal bacterial nephritis and acute pyelonephritis in children[J]. Cytokine, 2017, 99: 24-29. doi: 10.1016/j.cyto.2017.06.012
[2] Campos-Franco J, Macia C, Huelga E, et al. Acute focal bacterial nephritis in a cohort of hospitalized adult patients with acute pyelonephritis. Assessment of risk factors and a predictive model[J]. Eur J Intern Med, 2017, 39: 69-74. doi: 10.1016/j.ejim.2016.12.002
[3] García JL, Benavent MO, Monleón SF, et al. Predictive markers of acute focal bacterial nephritis. A multicentre case-control study[J]. An Pediatr(Engl Ed), 2020, 93(2): 77-83.
[4] Janett S, Milani GP, Faré PB, et al. Pyuria and microbiology in acute bacterial focal nephritis: a systematic review[J]. Minerva Med, 2019, 110(3): 232-237.
[5] Sieger N, Kyriazis I, Schaudinn A, et al. Acute focal bacterial nephritis is associated with invasive diagnostic procedures-a cohort of 138 cases extracted through a systematic review[J]. BMC Infect Dis, 2017, 17(1): 240. doi: 10.1186/s12879-017-2336-6
[6] Bitsori M, Raissaki M, Maraki S, et al. Acute focal bacterial nephritis, pyonephrosis and renal abscess in children[J]. Pediatr Nephrol, 2015, 30(11): 1987-1993. doi: 10.1007/s00467-015-3141-3
[7] Bibalo C, Apicella A, Guastalla V, et al. Acute lobar nephritis in children: Not so easy to recognize and manage[J]. World J Clin Pediatr, 2016, 5(1): 136-142. doi: 10.5409/wjcp.v5.i1.136
[8] Kline MW, Kaplan SL, Baker CJ. Acute focal bacterial nephritis: diverse clinical presentations in pediatric patients[J]. Pediatr Infect Dis J, 1988, 7(5): 346-349. doi: 10.1097/00006454-198805000-00012
[9] Hosokawa T, Tanami Y, Sato Y, et al. Comparison of imaging findings between acute focal bacterial nephritis(acute lobar nephronia)and acute pyelonephritis: a preliminary evaluation of the sufficiency of ultrasound for the diagnosis of acute focal bacterial nephritis[J]. Emerg Radiol, 2020, 27(4): 405-412. doi: 10.1007/s10140-020-01771-8
[10] Shimizu M, Katayama K, Kato E, et al. Evolution of acute focal bacterial nephritis into a renal abscess[J]. Pediatr Nephrol, 2005, 20(1): 93-95. doi: 10.1007/s00467-004-1646-2
[11] Sekine H, Kawasaki Y, Ohara S, et al. Focal bacterial nephritis without pyuria in a boy presenting with high urinary β2-MG and NAG levels[J]. Fukushima J Med Sci, 2014, 60(1): 91-94. doi: 10.5387/fms.2014-3
[12] Hosokawa T, Tanami Y, Sato Y, et al. Comparison of imaging findings between acute focal bacterial nephritis(acute lobar nephronia)and acute pyelonephritis: a preliminary evaluation of the sufficiency of ultrasound for the diagnosis of acute focal bacterial nephritis[J]. Emerg Radiol, 2020, 27(4): 405-412. doi: 10.1007/s10140-020-01771-8
[13] Esteban JM, Gomes E, Santamaría JF, et al. Hyperechoic focal bacterial nephritis: findings on contrast-enhanced Colour Doppler ultrasound[J]. Eur J Ultrasound, 2001, 13(3): 201-204. doi: 10.1016/S0929-8266(01)00136-7
[14] Yang CC, Shao PL, Lu CY, et al. Comparison of acute lobar nephronia and uncomplicated urinary tract infection in children[J]. J Microbiol Immunol Infect, 2010, 43(3): 207-214. doi: 10.1016/S1684-1182(10)60033-3
[15] Zulfiqar M, Ubilla CV, Nicola R, et al. Imaging of Renal Infections and Inflammatory Disease[J]. Radiol Clin North Am, 2020, 58(5): 909-923. doi: 10.1016/j.rcl.2020.05.004
[16] 章学泉, 夏凡. 急性局灶性细菌性肾炎的诊断及治疗(附12例报告)[J]. 中国中西医结合肾病杂志, 2004, 5(7): 420-421. doi: 10.3969/j.issn.1009-587X.2004.07.024
[17] Guella A, Khan A, Jarrah D. Acute Focal Bacterial Nephritis: Two Cases and Review of the Literature[J]. Can J Kidney Health Dis, 2019, 6: 2054358119884310.
[18] 傅淑霞, 邢玲玲, 段建召, 等. 急性局灶性细菌性肾炎55例临床分析[J]. 中华临床感染病杂志, 2015, 8(4): 340-343. doi: 10.3760/cma.j.issn.1674-2397.2015.04.012
[19] Yamaguchi H, Nagase H, Ito Y, et al. Acute focal bacterial nephritis characterized by acute encephalopathy with biphasic seizures and late reduced diffusion[J]. J Infect Chemother, 2018, 24(11): 932-935. doi: 10.1016/j.jiac.2018.04.007
[20] Udare A, Abreu-Gomez J, Krishna S, et al. Imaging Manifestations of Acute and Chronic Renal Infection That Mimics Malignancy: How to Make the Diagnosis Using Computed Tomography and Magnetic Resonance Imaging[J]. Can Assoc Radiol J, 2019, 70(4): 424-433. doi: 10.1016/j.carj.2019.07.002
[21] Demertzis J, Menias CO. State of the art: imaging of renal infections[J]. Emerg Radiol, 2007, 14(1): 13-22. doi: 10.1007/s10140-007-0591-3
[22] Craig WD, Wagner BJ, Travis MD. Pyelonephritis: radiologic-pathologic review[J]. Radiographics, 2008, 28(1): 255-277;quiz 327-328. doi: 10.1148/rg.281075171
[23] 陈植, 刘小荣, 孟群, 等. 儿童急性局灶性细菌性肾炎的临床特点[J]. 中华实用儿科临床杂志, 2017, 32(17): 1343-1345. doi: 10.3760/cma.j.issn.2095-428X.2017.17.016
[24] Sieger N, Kyriazis I, Schaudinn A, et al. Acute Focal Bacterial Nephritis Can Lead to Unnecessary Invasive Procedures: A Report of Three Cases[J]. Urol Int, 2017, 99(2): 245-248. doi: 10.1159/000441955
[25] 闫喆, 王春祥, 赵滨, 等. 儿童急性局灶性细菌性肾炎的DWI诊断价值[J]. 国际放射医学核医学杂志, 2018, 42(4): 332-336. doi: 10.3760/cma.j.issn.1673-4114.2018.04.008
-

| 引用本文: | 苏文桂, 杨猛, 徐磊, 等. 成人急性局灶性细菌性肾炎1例[J]. 临床泌尿外科杂志, 2022, 37(6): 483-485. doi: 10.13201/j.issn.1001-1420.2022.06.017 |
| Citation: | SU Wengui, YANG Meng, XU Lei, et al. One case report of adult acute focal bacterial nephritis[J]. J Clin Urol, 2022, 37(6): 483-485. doi: 10.13201/j.issn.1001-1420.2022.06.017 |
- Figure 1.
- Figure 2.
- Figure 3.
- Figure 4.
- Figure 5.
- Figure 6.
- Figure 7.
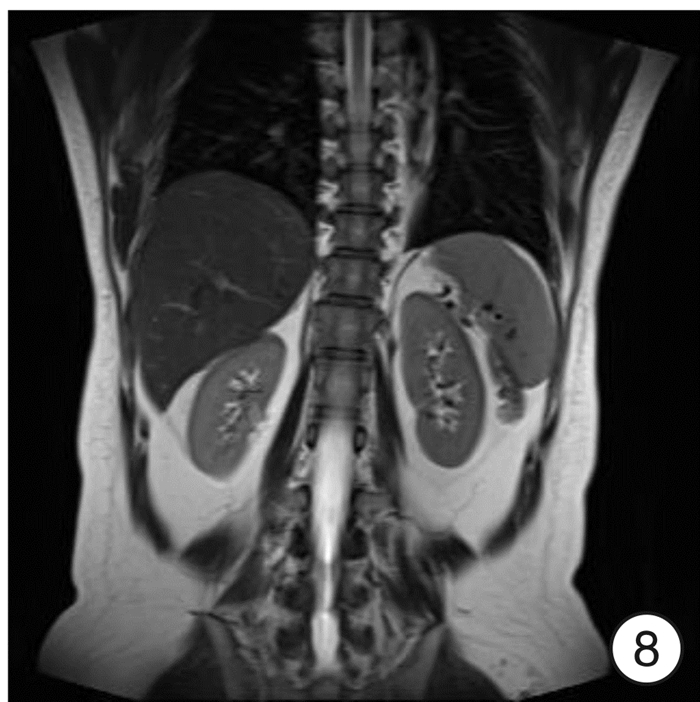
- Figure 8.




 下载:
下载: