-
摘要: 目的 探讨儿童睾丸损伤的分析与体会。方法 收集2015年1月—2020年12月河北省儿童医院收治的15例睾丸损伤患儿的临床资料,年龄3~14岁,中位年龄7岁;其中闭合性损伤12例,开放性损伤3例。左侧6例,右侧9例。对术前及术后1、3、6、12个月复查患侧睾丸体积、患侧/健侧睾丸体积比情况进行对比分析。结果 13例患儿行手术治疗,2例患儿保守治疗。术后随访12个月,有2例患儿患侧睾丸出现萎缩,其中1例为保守患儿,1例为睾丸破裂修补术后脓肿再次手术清创患儿;其余患儿睾丸均正常生长发育。所有患儿健侧睾丸随访期内均正常生长发育。术后第12个月复查患侧睾丸体积,与术前比较差异有统计学意义[(0.47±0.09) mL vs.(0.32±0.05) mL,P < 0.05];患侧/健侧睾丸体积比与术前比较差异无统计学意义[(0.93±0.06) vs.(1.05±0.03),P>0.05]。结论 对于阴囊损伤患儿应警惕有无合并睾丸损伤,准确的诊断和及时的手术探查可以最大限度地保留睾丸功能,减少睾丸萎缩概率等并发症出现。Abstract: Objective To explore the analysis and experience of testicular injury in children.Methods From January 2015 to December 2020, 15 children with testicular injury treated in Hebei Children's Hospital were selected. The relevant clinical data were collected. Their age ranged from 3 to 14 years, with a median age of 7 years, including 12 cases of closed injury and 3 cases of open injury. There were 6 cases on the left and 9 cases on the right. The volume of testis on the affected side and the volume ratio of testis on the affected side/healthy side were compared and analyzed before operation and 1, 3, 6 and 12 months after operation.Results Thirteen cases were treated with surgery and 2 cases were treated conservatively. After follow-up for 12 months, 2 cases were found testicular atrophy on the affected side. One case received conservative treatment, and the other case was reoperated because of abscess after testicular rupture repair. The testicles of other children grew and developed normally. The healthy-side testis of all children grew and developed normally during the follow-up period. The volume of testis on the affected side was (0.47±0.09) mL at the 12th month after operation, which was statistically significant compared with (0.32±0.05) mL before operation (P < 0.05). The volume ratio of testis on the affected side/healthy side was (0.93±0.06), which was not statistically significant compared with (1.05±0.03) before operation (P > 0.05).Conclusion Children with scrotal injury should be alert to the presence of combined testicular injury. Accurate diagnosis and timely surgical exploration can preserve testicular function to the greatest extent and reduce the probability of testicular atrophy and other complications.
-
Key words:
- children /
- testicular injury /
- testicular atrophy /
- treatment
-

-
表 1 手术前后不同时间点患侧与健侧睾丸发育情况比较
X±S 时间 患侧睾丸体积/mL 患侧/健侧睾丸体积比 术前 0.32±0.05 1.05±0.03 术后1个月 0.34±0.06 0.96±0.01 术后3个月 0.37±0.05 0.93±0.03 术后6个月 0.41±0.03 0.94±0.04 术后12个月 0.47±0.09 0.93±0.06 -
[1] Pogorelić Z, Jurić I, Biočić M, et al. Management of testicular rupture after blunt trauma in children[J]. Pediatr Surg Int, 2011, 27(8): 885-889. doi: 10.1007/s00383-011-2873-9
[2] Muttarak M, Thinyu S, Lojanapiwat B. Clinics in diagnostic imaging(114). Rupture of the right testis[J]. Singapore Med J, 2007, 48(3): 264-268;quiz 269.
[3] 薛恩生, 林礼务, 叶真, 等. 睾丸损伤的超声分型及临床应用评价[J]. 中华超声影像学杂志, 2000, 9(12): 736-738. doi: 10.3760/j.issn:1004-4477.2000.12.010
[4] Isikbay M, Sugi MD, Bowman MS. Traumatic testicular rupture: Multimodality imaging with intraoperative correlate[J]. Clin Imaging, 2021, 71: 13-16. doi: 10.1016/j.clinimag.2020.10.042
[5] Buckley JC, McAninch JW. Use of ultrasonography for the diagnosis of testicular injuries in blunt scrotal trauma[J]. J Urol, 2006, 175(1): 175-178. doi: 10.1016/S0022-5347(05)00048-0
[6] Powers R, Hurley S, Park E, et al. Usefulness of Preoperative Ultrasound for the Evaluation of Testicular Rupturein the Setting of Scrotal Gunshot Wounds[J]. J Urol, 2018, 199(6): 1546-1551. doi: 10.1016/j.juro.2018.01.076
[7] Rofe CJ, Abbas A, Bryant T. Traumatic testicular injury: a fracture not to miss[J]. Emerg Med, 2011, 28(9): 820.
[8] Buckley JC, McAninch JW. Diagnosis and management of testicular ruptures[J]. Urol Clin North Am, 2006, 33(1): 111-116, vii. doi: 10.1016/j.ucl.2005.11.002
[9] 王世先, 郭昭建, 张遵俊, 等. 外伤性睾丸破裂16例诊治体会[J]. 中国男科学杂志, 2010, 24(3): 55-57. doi: 10.3969/j.issn.1008-0848.2010.03.015
[10] Cass AS, Luxenberg M. Value of early operation in blunt testicular contusion with hematocele[J]. J Urol, 1988, 139(4): 746-747. doi: 10.1016/S0022-5347(17)42620-6
[11] 吴雄飞, 金锡御, 熊恩庆, 等. 睾丸损伤29例报告[J]. 中华创伤杂志, 1993, 9(1): 41-42. https://www.cnki.com.cn/Article/CJFDTOTAL-ZHCS199301022.htm
[12] Wang Z, Yang JR, Huang YM, et al. Diagnosis and management of testicular rupture after blunt scrotal trauma: a literature review[J]. Int Urol Nephrol, 2016, 48(12): 1967-1976. doi: 10.1007/s11255-016-1402-0
[13] Slavis SA, Scholz JN, Hewitt CW, et al. The effects of testicular trauma on fertility in the Lewis rat and comparisons to isoimmunized recipients of syngeneic sperm[J]. J Urol, 1990, 143(3): 638-641.
-

| 引用本文: | 许鹏, 周云, 齐灿, 等. 儿童睾丸损伤的诊治分析与体会[J]. 临床泌尿外科杂志, 2022, 37(8): 631-634. doi: 10.13201/j.issn.1001-1420.2022.08.012 |
| Citation: | XU Peng, ZHOU Yun, QI Can, et al. Diagnosis and treatment of testicular injury in children[J]. J Clin Urol, 2022, 37(8): 631-634. doi: 10.13201/j.issn.1001-1420.2022.08.012 |
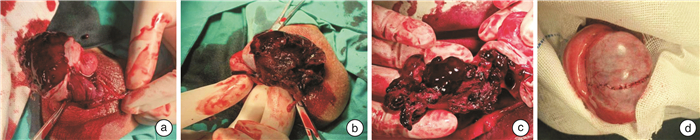
- Figure 1.
- Figure 2.




 下载:
下载: