Effect of urinary stone composition on acute kidney injury after percutaneous nephrolithotomy
-
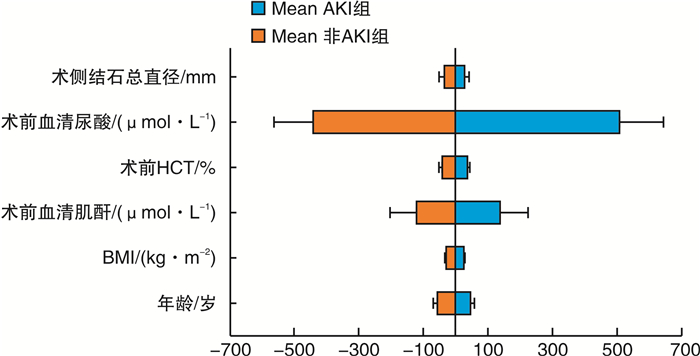
摘要: 目的 评估经皮肾镜取石术(PCNL)后更容易发生急性肾损伤(AKI)的病例的临床特征,并探究各结石成分是否影响PCNL术后AKI的发生。方法 收集2016年3月—2022年1月北京清华长庚医院收治的483例PCNL治疗的尿路结石患者的临床资料,包括人口学相关参数、检验参数、结石特征参数、手术相关资料共4方面的数据,将所有患者根据是否发生术后AKI分成2组,计算整体AKI的发生率,并比较组间各临床因素的差异,并对组间差异有统计学意义的尿酸结石患者进行进一步各临床参数的亚组分析。结果 483例患者PCNL术后AKI的发生率为6.00%,与非AKI组患者比较,既往有结石病史、术前血清肌酐升高、术前血清尿酸增高、血清钙离子降低及结石成分为尿酸结石的患者PCNL术后发生AKI的可能性增高(P < 0.05)。72例尿酸结石患者PCNL术后AKI的发生率为12.50%,术后发生AKI与未发生AKI的尿酸结石患者比较,各临床参数差异均无统计学意义(P>0.05),但发生AKI的尿酸结石患者术前血清肌酐及尿酸水平略高,合并糖尿病及术前尿培养阳性的患者比例亦有增高。结论 本中心患者PCNL术后AKI的发生率为6.00%,尿酸结石患者术后AKI发生率可能增高,PCNL术后AKI还多见于既往有结石病史、术前血清肌酐、尿酸增高及钙离子降低的患者。Abstract: Objective To evaluate the clinical characteristics of patients who are more likely to develop acute kidney injury (AKI) after percutaneous nephrolithotomy(PCNL), and to explore whether each stone composition affects the occurrence of AKI after PCNL.Methods The clinical data of 483 patients with urinary calculi treated by PCNL in Beijing Tsinghua Changgung Hospital from March 2016 to January 2022 were collected, including demographic-related parameters, test parameters, stone characteristic parameters, and operation-related data. All the patients were divided into two groups according to whether they had postoperative AKI. The overall incidence of AKI was calculated, and the differences in clinical factors between the two groups were compared.Results The incidence of AKI after PCNL was 6.00% in 483 patients. Compared with the non-AKI group, patients with a history of stones, an increase in preoperative serum creatinine, an increase in preoperative serum uric acid, a decrease in serum calcium, and uric acid stones were more likely to have AKI after PCNL (P < 0.05). The incidence of AKI after PCNL in 72 patients with uric acid stones was 12.50%. There was no significant difference in clinical parameters between patients with AKI and those without AKI (P > 0.05). Nonetheless, the preoperative serum creatinine and uric acid levels of patients with AKI were slightly higher. The proportion of patients with diabetes mellitus and positive urine culture before operation also increased.Conclusion The incidence of AKI after standard PCNL in our center is 6.00%. The incidence of AKI may increase in patients with uric acid stones after PCNL. The incidence of AKI after PCNL is also common in patients with a history of stones, an increase in preoperative serum creatinine and uric acid and a decrease in serum calcium.
-
Key words:
- acute kidney injury /
- percutaneous nephrolithotomy /
- urolithiasis /
- stone composition /
- uric acid stone
-

-
表 1 AKI组和非AKI组人口学相关各参数的比较
例(%),M(P25,P75) 参数 总体(483例) 非AKI组(454例) AKI组(29例) P值 统计值 年龄/岁 53.00(42.00,60.00) 53.00(42.00,60.00) 54.00(42.00,64.00) 0.411 0.676 性别 0.043 4.098 男 316(65.42) 292(64.32) 24(82.76) 女 167(34.58) 162(35.68) 5(17.24) BMI/(kg·m-2) 25.04(22.88,27.74) 25.03(22.91,27.68) 25.16(21.72,28.73) 0.958 0.003 结石病史 0.028 4.839 无 136(28.16) 133(29.3) 3(10.34) 有 347(71.84) 321(70.7) 26(89.66) 合并髓质海绵肾 0.585 - 无 469(97.10) 441(97.14) 28(96.55) 有 14(2.90) 13(2.86) 1(3.45) 合并马蹄肾 1.000 - 无 464(96.07) 436(96.04) 28(96.55) 有 19(3.93) 18(3.96) 1(3.45) 合并脊柱畸形 0.430 - 无 474(98.14) 446(98.24) 28(96.55) 有 9(1.86) 8(1.76) 1(3.45) 糖尿病 1.000 - 无 403(83.44) 379(83.48) 24(82.76) 有 80(16.56) 75(16.52) 5(17.24) 高血压 0.641 0.218 无 319(66.05) 301(66.3) 18(62.07) 有 164(33.95) 153(33.7) 11(37.93) CKD 0.220 - 无 479(99.17) 451(99.34) 28(96.55) 有 4(0.83) 3(0.66) 1(3.45) 痛风 0.267 - 无 478(98.96) 450(99.12) 28(96.55) - - 有 5(1.04) 4(0.88) 1(3.45) - - 表 2 AKI组和非AKI组检验资料各参数的比较
例(%),M(P25,P75) 参数 总体(483例) 非AKI组(454例) AKI组(29例) P值 统计值 术前尿培养 0.263 1.255 阴性 313(64.80) 297(65.42) 16(55.17) 阳性 170(35.20) 157(34.58) 13(44.83) 术前血清肌酐/
(μmol·L-1)72.80(61.85,89.85) 72.25(61.23,87.30) 97.60(74.80,153.20) < 0.001 17.928 术后24 h内血清肌酐/
(μmol·L-1)78.60(64.20,96.95) 77.00(63.85,93.62) 131.40(114.60,189.40) < 0.001 54.436 术前HCT/% 40.70(37.10,44.60) 40.70(37.10,44.60) 40.80(36.10,44.10) 0.933 0.007 术前血清尿酸/
(μmol·L-1)357.00(300.00,438.50) 355.00(297.00,435.50) 398.00(343.00,481.00) 0.004 8.297 术前血清钙离子/
(mmol·L-1)2.24(2.18,2.31) 2.25(2.18,2.32) 2.20(2.13,2.25) 0.003 8.529 表 3 AKI组和非AKI组结石特征及手术相关资料各参数的比较
例(%),M(P25,P75) 参数 总体(483例) 非AKI组(454例) AKI组(29例) P值 统计值 术侧结石总直径/mm 28.00(20.00,40.00) 28.00(20.00,40.00) 33.00(20.00,40.00) 0.515 0.424 术侧积水程度 0.440 - 无 168(34.78) 155(34.14) 13(44.83) 轻度 242(50.10) 230(50.66) 12(41.38) 中度 64(13.25) 61(13.44) 3(10.34) 重度 9(1.86) 8(1.76) 1(3.45) 草酸钙结石 0.040 4.231 否 165(34.16) 150(33.04) 15(51.72) 是 318(65.84) 304(66.96) 14(48.28) 鸟粪石 0.840 0.041 否 390(80.75) 367(80.84) 23(79.31) 是 93(19.25) 87(19.16) 6(20.69) 尿酸石 0.026 - 否 411(85.09) 391(86.12) 20(68.97) 是 72(14.91) 63(13.88) 9(31.03) 术前留置支架管/造瘘管 0.593 - 无 413(85.51) 389(85.68) 24(82.76) 有 70(14.49) 65(14.32) 5(17.24) 手术时长/min 94.00(73.00,120.50) 94.00(72.00,120.00) 105.00(83.00,144.00) 0.062 3.478 表 4 AKI组和非AKI组各参数的单因素分析
参数 OR(95%CI) P值 性别 0.376(0.141~1.003) 0.051 结石病史 3.591(1.069~12.067) 0.039 术前血清肌酐/
(μmol·L-1)1.004(1.001~1.007) 0.009 术前血清尿酸/
(μmol·L-1)1.005(1.002~1.008) 0.001 术前血清钙离子/
(mmol·L-1)0.003(0~0.158) 0.004 草酸钙结石 0.461(0.217~0.979) 0.044 尿酸石 2.793(1.217~6.408) 0.015 表 5 尿酸结石中AKI组和非AKI组各参数的比较
例(%),M(P25,P75) 参数 尿酸结石非AKI组(63例) 尿酸结石AKI组(9例) P值 统计值 年龄/岁 55.00(49.00,62.50) 47.00(44.00,56.00) 0.173 1.858 性别 0.679 - 男 50(79.37) 8(88.89) 女 13(20.63) 1(11.11) BMI/(kg·m-2) 26.04(23.82,29.36) 28.72(27.55,29.17) 0.072 3.227 结石病史 1 - 无 19(30.16) 2(22.22) 有 44(69.84) 7(77.78) 糖尿病 0.441 - 无 45(71.43) 5(55.56) 有 18(28.57) 4(44.44) 高血压 0.494 - 无 30(47.62) 3(33.33) 有 33(52.38) 6(66.67) 痛风 0.421 - 无 60(95.24) 8(88.89) 有 3(4.76) 1(11.11) 术前尿培养 0.14 - 阴性 41(65.08) 3(33.33) 阳性 22(34.92) 6(66.67) 术侧积水程度 0.082 - 无 23(36.51) 5(55.56) 轻度 34(53.97) 3(33.33) 中度 6(9.52) 0(0) 重度 0(0) 1(11.11) 术前有无支架管 0.363 - 无 52(82.54) 6(66.67) 有 11(17.46) 3(33.33) 手术侧结石总量/mm 30.00(22.50,41.50) 35.00(28.00,40.00) 0.805 0.061 术前血清肌酐/(μmol·L-1) 83.30(72.50,125.80) 107.70(85.80,146.50) 0.090 2.870 术后24 h内血清肌酐/(μmol·L-1) 93.10(81.65,123.70) 170.30(121.20,180.80) 0.002 9.762 术前HCT/% 41.10(37.05,45.50) 43.40(40.70,44.10) 0.871 0.026 术前血清尿酸/(μmol·L-1) 440.00(352.50,499.50) 481.00(473.00,582.00) 0.084 2.987 术前血清钙离子/(mmol·L-1) 2.25(2.18,2.33) 2.18(2.15,2.25) 0.093 2.819 手术时长/min 100.00(76.00,121.00) 112.00(105.00,150.00) 0.113 2.509 -
[1] Verma S, Kellum JA. Defining Acute Kidney Injury[J]. Crit Care Clin, 2021, 37(2): 251-266. doi: 10.1016/j.ccc.2020.11.001
[2] Liangos O, Wald R, O'Bell JW, et al. Epidemiology and outcomes of acute renal failure in hospitalized patients: a national survey[J]. Clin J Am Soc Nephrol, 2006, 1(1): 43-51. doi: 10.2215/CJN.00220605
[3] Ostermann M, Zarbock A, Goldstein S, et al. Recommendations on Acute Kidney Injury Biomarkers From the Acute Disease Quality Initiative Consensus Conference: A Consensus Statement[J]. JAMA Netw Open, 2020, 3(10): e2019209. doi: 10.1001/jamanetworkopen.2020.19209
[4] 李建兴, 肖博. 经皮肾镜取石术在肾结石治疗中的地位[J]. 临床外科杂志, 2017, 25(2): 89-90. https://www.cnki.com.cn/Article/CJFDTOTAL-LCWK201702003.htm
[5] Fulla J, Prasanchaimontri P, Wright HC, et al. Acute kidney injury and percutaneous nephrolithotomy: incidence and predictive factors[J]. World J Urol, 2022, 40(2): 563-567. doi: 10.1007/s00345-021-03874-4
[6] Shi X, Peng Y, Li L, et al. Renal function changes after percutaneous nephrolithotomy in patients with renal calculi with a solitary kidney compared to bilateral kidneys[J]. BJU Int, 2018, 122(4): 633-638. doi: 10.1111/bju.14413
[7] Yu J, Park HK, Kwon HJ, et al. Risk factors for acute kidney injury after percutaneous nephrolithotomy: Implications of intraoperative hypotension[J]. Medicine(Baltimore), 2018, 97(30): e11580.
[8] Corrales M, Doizi S, Barghouthy Y, et al. Classification of Stones According to Michel Daudon: A Narrative Review[J]. Eur Urol Focus, 2021, 7(1): 13-21. doi: 10.1016/j.euf.2020.11.004
[9] Patel PM, Kandabarow AM, Druck A, et al. Association of Impaired Renal Function With Changes in Urinary Mineral Excretion and Stone Composition[J]. Urology, 2020, 141: 45-49. doi: 10.1016/j.urology.2020.03.023
[10] Li X, Wang LP, Ou LL, et al. Revolution spectral CT for urinary stone with a single/mixed composition in vivo: a large sample analysis[J]. World J Urol, 2021, 39(9): 3631-3642. doi: 10.1007/s00345-021-03597-6
[11] Larcher L, Lefevre G, Bailleul S, et al. Importance of pre-analytical for urinalysis with urinary crystals. Dosages biochimiquesurinaires dans les urines présentant des cristaux: importance de la phase préanalytique[J]. Ann Biol Clin(Paris), 2017, 75(5): 525-530.
[12] Mehta RL, Kellum JA, Shah SV, et al. Acute Kidney Injury Network: report of an initiative to improve outcomes in acute kidney injury[J]. Crit Care, 2007, 11(2): R31. doi: 10.1186/cc5713
[13] Keller EX, De Coninck V, Audouin M, et al. Stone composition independently predicts stone size in 18, 029 spontaneously passed stones[J]. World J Urol, 2019, 37(11): 2493-2499. doi: 10.1007/s00345-018-02627-0
[14] Tabibzadeh N, Zalc M, Michel T, et al. Prevalence and identification of crystalluria in critically ill patients: association between uric acid crystals and sepsis[J]. Clin Kidney J, 2020, 14(4): 1291-1293.
[15] Caddeo G, Williams ST, McIntyre CW, et al. Acute kidney injury in urology patients: incidence, causes and outcomes[J]. Nephrourol Mon, 2013, 5(5): 955-961. doi: 10.5812/numonthly.12721
[16] Hobson C, Ozrazgat-Baslanti T, Kuxhausen A, et al. Cost and Mortality Associated With Postoperative Acute Kidney Injury[J]. Ann Surg, 2015, 261(6): 1207-1214. doi: 10.1097/SLA.0000000000000732
[17] Reeves T, Pietropaolo A, Gadzhiev N, et al. Role of Endourological Procedures(PCNL and URS)on Renal Function: a Systematic Review[J]. Curr Urol Rep, 2020, 21(5): 21. doi: 10.1007/s11934-020-00973-4
[18] Hsu CY, Iribarren C, McCulloch CE, et al. Risk factors for end-stage renal disease: 25-year follow-up[J]. Arch Intern Med, 2009, 169(4): 342-350. doi: 10.1001/archinternmed.2008.605
[19] Zhou F, Yu G, Wang G, et al. Association of serum uric acid levels with the incident of kidney disease and rapid eGFR decline in Chinese individuals with eGFR>60 mL/min/1.73 m2and negative proteinuria[J]. Clin Exp Nephrol, 2019, 23(7): 871-879. doi: 10.1007/s10157-019-01705-w
[20] Su HY, Yang C, Liang D, et al. Research Advances in the Mechanisms of Hyperuricemia-Induced Renal Injury[J]. Biomed Res Int, 2020, 2020: 5817348.
[21] 张勇, 陈站, 陈建刚, 等. 尿酸结石致病相关基因的研究进展[J]. 临床泌尿外科杂志, 2021, 36(2): 148-151. https://www.cnki.com.cn/Article/CJFDTOTAL-LCMW202102016.htm
[22] Spatola L, Angelini C, Badalamenti S, et al. Kidney stones diseases and glycaemic statuses: focus on the latest clinical evidences[J]. Urolithiasis, 2017, 45(5): 457-460. doi: 10.1007/s00240-016-0956-8
[23] Singh NP, Panwar V, Aggarwal NP, et al. Regulation of Calcium Homeostasis in Acute Kidney Injury: A Prospective Observational Study[J]. Indian J Crit Care Med, 2022, 26(3): 302-306. doi: 10.5005/jp-journals-10071-24124
[24] Cheikh Hassan HI, Murali K, Lambert K, et al. Acute kidney injury increases risk of kidney stones-a retrospective propensity score matched cohort study[J]. Nephrol Dial Transplant, 2022.
-




 下载:
下载: