Single-center large-sample clinical study on transurethral holmium laser enucleation of the prostate with en-bloc technique
-
摘要: 目的 分析保留膀胱颈的整叶法经尿道前列腺钬激光剜除术(holmium laser enucleation of the prostate,HoLEP)治疗良性前列腺增生(benign prostatic hyperplasia,BPH)的有效性和安全性,探讨其在尿控及性功能保护方面的意义。方法 回顾性分析2012年6月—2022年6月在南京医科大学第一附属医院接受保留膀胱颈的整叶法HoLEP治疗,并有完整信息的3 116例BPH患者的临床资料,记录患者基线资料、围手术期数据,随访时间12个月。排尿功能采用国际前列腺症状评分(international prostate symptom score,IPSS)、最大尿流率(Qmax)、残余尿(post-void residual urine,PVR)和生活质量(quality of life,QoL)评分进行评估。对于术前有性活动并有正常顺行射精的213例患者,进一步评估勃起功能及射精功能。结果 平均手术时间为(68.3±15.4) min,切除腺体重量为(55.3±16.7)g,估计失血量为(61.2±22.6) mL;平均住院时间和术后留置导尿管时间分别为(5.1±3.3) d和(2.0±1.4) d。术后第2天进行拔管,首次拔管失败率为4.5%(141/3 116)。与术前比较,术后3、6、12个月IPSS、Qmax、PVR及QoL等指标均有显著改善(P < 0.05),且在随访过程中持续稳定。术后3个月尿失禁发生率为11.1%(346/3 116),多数患者在术后1年内恢复,长期尿失禁23例(0.7%)。对于性功能评估亚组的213例患者,术后国际勃起功能指数(IIEF-5)评分及勃起硬度分级量表(EHGS)均无显著变化(P>0.05);术后逆行射精患者共61例(28.6%)。所有患者术后均无射精痛。结论 整叶法HoLEP治疗BPH是安全有效的,术中采用保留膀胱颈的技术可以有效改善尿控功能,保护性功能,尤其是减少逆行射精的发生。
-
关键词:
- 良性前列腺增生 /
- 经尿道前列腺钬激光剜除 /
- 性功能 /
- 大样本
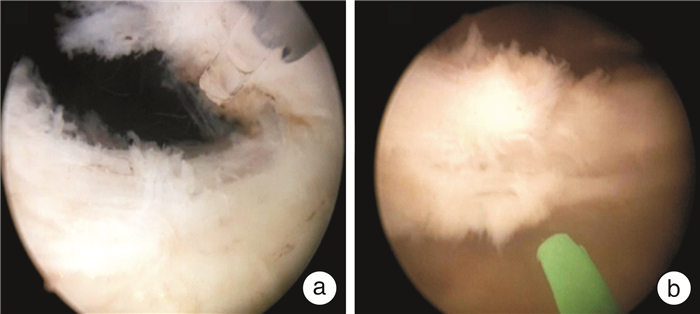
Abstract: Objective To study the efficacy and safety of holmium laser enucleation of the prostate(HoLEP) with en-bloc and bladder neck preservation technique for the treatment of benign prostatic hyperplasia(BPH), and to explore its significance in urinary control and sexual function protection.Methods We retrospectively analyzed the clinical data of 3 116 patients who were treated with HoLEP with en-bloc and bladder neck preservation technique at the First Affiliated Hospital of Nanjing Medical University from June 2012 to June 2022. The follow-up period was 12 months, and the baseline characteristics, perioperative and outcome data were recorded. The voiding function was assessed by the International Prostate Symptom Score(IPSS), maximum urinary flow rate(Qmax), post-void residual urine(PVR), and quality of life(QoL) score. Erectile and ejaculatory function were further assessed in 213 patients who were sexually active preoperatively and had normal antegrade ejaculation.Results The mean operative time was (68.3±15.4)min, and the mean weight of resected gland was (55.3±16.7)g, the estimated blood loss was (61.2±22.6)mL, the mean length of hospitalization and postoperative catheterization were (5.1±3.3) and (2.0±1.4) days, respectively. The catheter was removed at second postoperative day, and the failure rate of the first removal was 4.5%(141/3 116). Compared with the preoperative level, IPSS, Qmax, PVR, and QoL were significantly improved at 3, 6, and 12 months postoperatively(P < 0.05) and continued to stabilize during the follow-up. The incidence of urinary incontinence at 3 months was 11.1%(346/3 116). Most patients recovered within one year postoperatively, but there were 23 cases of persistent urinary incontinence(0.7%). For the 213 patients in the sexual function assessment subgroup, there was no significant change in the International Index of Erectile Function(IIEF-5) score or the Erectile Hardness Grading Scale(EHGS) after operation(P>0.05); a total of 61 patients(28.6%) suffered from retrograde ejaculation after the operation. No patients had ejaculatory pain after surgery.Conclusion HoLEP with en-bloc and bladder neck preservation technique is safe and effective, for it can effectively improve urinary control function, protect sexual function, and significantly reduce the incidence of retrograde ejaculation. -

-
表 1 术前及术后排尿功能和尿失禁情况
X±S 项目 术前 术后3个月 术后6个月 术后12个月 IPSS/分 22.3±3.5 6.7±1.81) 5.9±1.11) 5.3±2.01) PVR/mL 97.3±82.4 21.5±15.81) 22.7±14.71) 21.4±12.31) Qmax/(mL/s) 5.6±2.3 19.5±3.41) 20.2±2.11) 20.5±3.71) QoL/分 5.1±1.0 2.6±0.81) 2.2±0.61) 2.1±0.71) 压力性尿失禁/例(%) 轻度 266(8.5) 97(3.1) 14(0.5) 中度 73(2.3) 14(0.4) 6(0.06) 重度 7(0.2) 4(0.1) 3(0.09) 与术前比较,1)P < 0.05。 表 2 手术前后患者性功能的比较
例(%),X±S 项目 术前 术后6个月 术后12个月 P1 P2 IIEF-5/分 17.02±3.75 17.33±2.04 17.34±3.39 0.67 0.75 EHGS/分 3.03±0.62 3.06±0.52 3.02±0.44 0.74 0.86 射精疼痛 0(0) 0(0) 0(0) 逆行射精 0(0) 25(11.7) 25(11.7) 精液量 增加 0(0) 0(0) 减少 82(43.6) 82(43.6) 不变 106(56.4) 106(56.4) 注:P1,术后6个月vs术前;P2,术后12个月vs术前。 -
[1] Hashim H, Abrams P. Transurethral resection of the prostate for benign prostatic obstruction: will it remain the gold standard?[J]. Eur Urol, 2015, 67(6): 1097-1098.
[2] Pyrgidis N, Mykoniatis I, Lusuardi L, et al. Enucleation of the prostate as retreatment for recurrent or residual benign prostatic obstruction: a systematic review and a meta-analysis[J]. Prostate Cancer Prostatic Dis, 2023.
[3] Lin YH, Chang SY, Tsao SH, et al. Anterior fibromuscular stroma-preserved endoscopic enucleation of the prostate: a precision anatomical approach[J]. World J Urol, 2023, 41(8): 2127-2132.
[4] Das AK, Han TM, Hardacker TJ. Holmium laser enucleation of the prostate(HoLEP): size-independent gold standard for surgical management of benign prostatic hyperplasia[J]. Can J Urol, 2020, 27(S3): 44-50.
[5] Sun FZ, Yao HB, Bao XJ, et al. The efficacy and safety of HoLEP for benign prostatic hyperplasia with large volume: a systematic review and meta-analysis[J]. Am J Mens Health, 2022, 16(4): 15579883221113203.
[6] Shvero A, Calio B, Humphreys MR, et al. HoLEP: the new gold standard for surgical treatment of benign prostatic hyperplasia[J]. Can J Urol, 2021, 28(S2): 6-10.
[7] Das AK, Teplitsky S, Humphreys MR. Holmium laser enucleation of the prostate(HoLEP): a review and update[J]. Can J Urol, 2019, 26(4 Suppl 1): 13-19.
[8] Couteau N, Duquesne I, Frédéric P, et al. Ejaculations and benign prostatic hyperplasia: an impossible compromise?A comprehensive review[J]. J Clin Med, 2021, 10(24): 5788.
[9] Li P, Wang CM, Tang M, et al. Holmium laser enucleation of prostate by using en-bloc and bladder neck preservation technique: technical consideration and influence on functional outcomes[J]. Transl Androl Urol, 2021, 10(1): 134-142.
[10] Altinbas NK, Hamidi N. Penile Doppler ultrasonography and elastography evaluation in patients with erectile dysfunction[J]. Pol J Radiol, 2018, 83: e491-e499.
[11] Teo JS, Lee YM, Ho HSS. An update on transurethral surgery for benign prostatic obstruction[J]. Asian J Urol, 2017, 4(3): 195-198.
[12] Bearelly P, Avellino GJ. The role of benign prostatic hyperplasia treatments in ejaculatory dysfunction[J]. Fertil Steril, 2021, 116(3): 611-617.
[13] Manfredi C, García-Gómez B, Arcaniolo D, et al. Impact of surgery for benign prostatic hyperplasia on sexual function: a systematic review and meta-analysis of erectile function and ejaculatory function[J]. Eur Urol Focus, 2022, 8(6): 1711-1732.
[14] Brunocilla E, Schiavina R, Borghesi M, et al. Preservation of the internal vesical sphincter and proximal urethra during retropubic radical prostatectomy may improve earlier recovery of continence in selected patients[J]. Actas Urol Esp, 2014, 38(7): 421-428.
[15] Aho T, Armitage J, Kastner C. Anatomical endoscopic enucleation of the prostate: the next gold standard?Yes![J]. Andrologia, 2020, 52(8): e13643.
[16] Oh SJ, Shitara T. Enucleation of the prostate: an anatomical perspective[J]. Andrologia, 2020, 52(8): e13744.
[17] Boxall NE, Georgiades F, Miah S, et al. A call for HoLEP: AEEP for mega-prostates(≥ 200 cc)[J]. World J Urol, 2021, 39(7): 2347-2353.
[18] Zell MA, Abdul-Muhsin H, Navaratnam A, et al. Holmium laser enucleation of the prostate for very large benign prostatic hyperplasia(≥ 200 cc)[J]. World J Urol, 2021, 39(1): 129-134.
[19] Zhang JJ, Ou ZY, Zhang XB, et al. Holmium laser enucleation of the prostate versus thulium laser enucleation of the prostate for the treatment of large-volume prostates>80 ml: 18-month follow-up results[J]. World J Urol, 2020, 38(6): 1555-1562.
[20] Yilmaz M, Esser J, Suarez-Ibarrola R, et al. Safety and efficacy of laser enucleation of the prostate in elderly patients-A narrative review[J]. Clin Interv Aging, 2022, 17: 15-33.
[21] Boeri L, Capogrosso P, Ventimiglia E, et al. Clinical comparison of holmium laser enucleation of the prostate and bipolar transurethral enucleation of the prostate in patients under either anticoagulation or antiplatelet therapy[J]. Eur Urol Focus, 2020, 6(4): 720-728.
[22] Abedi A, Razzaghi MR, Rahavian A, et al. Is holmium laser enucleation of the prostate a good surgical alternative in benign prostatic hyperplasia management?A review article[J]. J Lasers Med Sci, 2020, 11(2): 197-203.
[23] Houssin V, Olivier J, Brenier M, et al. Predictive factors of urinary incontinence after holmium laser enucleation of the prostate: a multicentric evaluation[J]. World J Urol, 2021, 39(1): 143-148.
[24] Kim A, Hak AJ, Choi WS, et al. Comparison of long-term effect and complications between holmium laser enucleation and transurethral resection of prostate: nations-wide health insurance study[J]. Urology, 2021, 154: 300-307.
[25] Droghetti M, Porreca A, Bianchi L, et al. Long-term outcomes of Holmium laser enucleation of prostate and predictive model for symptom recurrence[J]. Prostate, 2022, 82(2): 203-209.
[26] Stolzenburg JU, Rabenalt R, Do M, et al. Intrafascial nerve-sparing endoscopic extraperitoneal radical prostatectomy[J]. Eur Urol, 2008, 53(5): 931-940.
[27] Sato R, Sano A, Watanabe K, et al. Effects of changes in erectile function after holmium laser enucleation of the prostate on postoperative outcomes in patients with benign prostatic hyperplasia[J]. In Vivo, 2022, 36(6): 2960-2964.
[28] Kim JK, Cho MC, Son H, et al. Patient perception of ejaculatory volume reduction after holmium laser enucleation of the prostate(HoLEP)[J]. Urology, 2017, 99: 142-147.
[29] Gild P, Dahlem R, Pompe RS, et al. Retrograde ejaculation after holmium laser enucleation of the prostate(HoLEP)-Impact on sexual function and evaluation of patient bother using validated questionnaires[J]. Andrology, 2020, 8(6): 1779-1786.
-




 下载:
下载: