Study on sleep structure and respiratory characteristics of children with nocturnal enuresis through overnight polysomnography
-
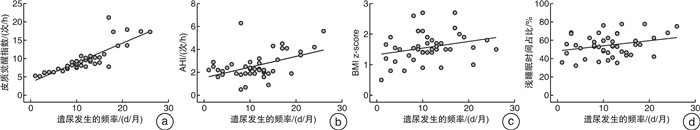
摘要: 目的 探究夜间遗尿症(nocturnal enuresis,NE)患儿的睡眠呼吸特征和相关影响因素。方法 选取2021年6月—2023年3月于郑州大学第一附属医院确诊为NE的患儿45例,按照是否存在日间下尿路症状,分为单症状性夜间遗尿(monosymptomatic nocturnal enuresis,MNE)组与非单症状性夜间遗尿(non-monosymptomatic nocturnal enuresis,NMNE)组,对所有患儿进行整夜多导睡眠监测(polysomnography,PSG)并记录7天排尿日记。同期选取在我院因上尿路疾病就诊而无下尿路功能障碍的儿童25例为对照组,行PSG检查。结果 与对照组相比,NE患儿的睡眠呼吸暂停低通气指数(apnea hypopnea index,AHI)、体重指数标准分数(BMI z-score)及皮质觉醒指数升高(均P < 0.05),3组在血氧饱和度及平均血压之间均差异无统计学意义(均P>0.05)。相对于MNE组,NMNE组在非快速眼动睡眠中浅睡眠时相的所占睡眠时间百分及皮质觉醒指数显著增高[(61.1±9.5)% vs(48.0±10.6)%,(10.5±4.2)次/h vs (8.6±2.8)次/h,P < 0.001],而平均心率显著降低[(69.5±5.7)次/min vs (82.7±4.3)次/min,P < 0.001];并且NMNE组的BMI z-score高于MNE组[(1.7±0.5) vs (1.4±0.4),P < 0.001]。皮质觉醒指数及AHI分别与每月遗尿夜晚数呈正相关(r=0.848,P < 0.001;r=0.466,P=0.001)。结论 NE患儿睡眠呼吸障碍多见,发生率与日间下尿路症状、遗尿严重程度和肥胖呈正相关。Abstract: Objective To investigate the sleep and respiratory characteristics and its related factors in children with nocturnal enuresis(NE).Methods A total of 45 children with NE from June 2021 to March 2023 were collected. They were categorized into monosymptomatic nocturnal enuresis(MNE) and non-monosymptomatic nocturnal enuresis(NMNE) groups. A control group contains 25 children without lower urinary tract dysfunction. All-night polysomnography(PSG) monitoring and a 7-day urination diary were carried out in all children.Results Compared with the control group, NE group showed an increase in sleep apnea hypopnea index(AHI), body mass index standard score(BMI z-score), and cortical arousal index(CAI) (P < 0.05). There were no significant differences in blood oxygen saturation or mean blood pressure among the three groups(P>0.05). The NMNE group showed a significant increase in sleep time and CAI during the light sleep phase in non-rapid eye movement sleep([61.1±9.5]% vs [48.0±10.6]%, [10.5±4.2] times/h vs [8.6±2.8] times/h, P < 0.001). Additionally, the average heart rate significantly decreased([69.5±5.7] times/min vs [82.7±4.3] times/min, P < 0.001). The BMI z-score of the NMNE group was higher than that of the MNE group([1.7±0.5] vs [1.4±0.4], P < 0.001). Both CAI and AHI were positively correlated with the days of enuresis per month(r=0.848, P < 0.001; r=0.466, P=0.001).Conclusion Sleep breathing disorder in children with NE is common, and the incidence is associated with daytime lower urinary tract symptoms, severity level of NE and obesity in children with NE.
-

-
表 1 NE组与对照组患儿的一般情况比较
例(%),X±S 项目 NMNE组(23例) MNE组(22例) 对照组(25例) χ2/F P值 年龄/岁 12.2±2.7 12.0±3.3 11.7±2.1 0.209 0.812 男性 12(52.2) 9(40.9) 12(48.0) 0.584 0.747 BMI z-score 1.7±0.51)2) 1.4±0.41) 1.1±0.3 15.218 < 0.001 1)与对照组相较,P < 0.05;2)与MNE组相较,P < 0.05。 表 2 NE组与对照组患儿的PSG参数比较
X±S 参数 NMNE组(22例) MNE组(23例) 对照组(25例) χ2/F P值 睡眠时间占比/% N1 11.4±2.21)2) 6.3±3.0 4.9±1.7 50.642 < 0.001 N2 49.7±9.6 41.7±8.9 41.7±7.7 6.528 0.003 浅睡眠(N1+N2) 61.1±9.51)2) 48.0±10.6 46.6±7.3 17.815 < 0.001 N3 20.3±9.21)2) 31.8±10.4 32.7±7.4 13.359 < 0.001 REM 18.6±6.0 20.2±3.9 21.0±3.5 1.619 0.206 AHI/(次/h) 2.6±1.01) 2.5±0.71) 0.6±0.2 62.976 < 0.001 平均心率/(次/min) 69.5±5.71)2) 82.7±4.3 82.5±4.4 56.248 < 0.001 平均SpO2/% 95.4±1.9 95.1±2.2 96.3±1.9 2.351 0.103 最低SpO2/% 86.3±2.1 87.6±2.4 87.4±2.8 1.734 0.179 最高SpO2/% 97.0±1.6 96.6±1.5 97.6±1.7 2.276 0.110 平均血压/mmHg 90.8±5.9 91.7±4.0 92.6±3.5 0.895 0.414 皮质觉醒指数/(次/h) 10.5±4.21)2) 8.6±2.81) 3.7±1.6 32.512 < 0.001 1)与对照组相较,P < 0.05;2)与MNE组相较,P < 0.05。 -
[1] Austin PF, Bauer SB, Bower W, et al. The standardization of terminology of lower urinary tract function in children and adolescents: Update report from the standardization committee of the International Children's Continence Society[J]. Neurourol Urodyn, 2016, 35(4): 471-481. doi: 10.1002/nau.22751
[2] 中华医学会小儿外科学分会小儿尿动力和盆底学组和泌尿外科学组. 儿童遗尿症诊断和治疗中国专家共识[J]. 中华医学杂志, 2019, 99(21): 1615-1620. doi: 10.3760/cma.j.issn.0376-2491.2019.21.005
[3] Wang QW, Wen JG, Zhu QH, et al. The effect of familial aggregation on the children with primary nocturnal enuresis[J]. Neurourol Urodyn, 2009, 28(5): 423-426. doi: 10.1002/nau.20666
[4] Cohen-Zrubavel V, Kushnir B, Kushnir J, et al. Sleep and sleepiness in children with nocturnal enuresis[J]. Sleep, 2011, 34(2): 191-194. doi: 10.1093/sleep/34.2.191
[5] Nevéus T, Leissner L, Rudblad S, et al. Respiration during sleep in children with therapy-resistant enuresis[J]. Acta Paediatr, 2014, 103(3): 300-304. doi: 10.1111/apa.12515
[6] Soster LA, Alves RC, Fagundes SN, et al. Non-REM sleep instability in children with primary monosymptomatic sleep enuresis[J]. J Clin Sleep Med, 2017, 13(10): 1163-1170. doi: 10.5664/jcsm.6762
[7] Yeung CK, Diao M, Sreedhar B. Cortical arousal in children with severe enuresis[J]. N Engl J Med, 2008, 358(22): 2414-2415. doi: 10.1056/NEJMc0706528
[8] Zhang QY, Zhu W, Wang CY, et al. Nocturnal bladder function and sleep in the children with refractory nocturnal enuresis: a prospective study[J]. Urology, 2023, 182: 218-224. doi: 10.1016/j.urology.2023.08.032
[9] Dhondt K, van Herzeele C, Roels SP, et al. Sleep fragmentation and periodic limb movements in children with monosymptomatic nocturnal enuresis and polyuria[J]. Pediatr Nephrol, 2015, 30(7): 1157-1162. doi: 10.1007/s00467-015-3044-3
[10] Haid B, Tekgül S. Primary and secondary enuresis: pathophysiology, diagnosis, and treatment[J]. Eur Urol Focus, 2017, 3(2-3): 198-206. doi: 10.1016/j.euf.2017.08.010
[11] Kitta T, Mitsui T, Kanno Y, et al. Brain-bladder control network: the unsolved 21st century urological mystery[J]. Int J Urol, 2015, 22(4): 342-348. doi: 10.1111/iju.12721
[12] 王庆伟, 张钦涌, 朱文, 等. 多导睡眠监测联合动态尿动力评估原发单症状性夜间遗尿症患儿的膀胱功能及睡眠特征[J]. 中华医学杂志, 2022, 102(38): 2994-3000. doi: 10.3760/cma.j.cn112137-20220122-00169
[13] Shafiek H, Evangelisti M, Hassan N, et al. The association between obstructive sleep apnea and nocturnal enuresis in children[C]//7.1 Paediatric Respiratory Physiology and Sleep. European Respiratory Society, 2016, 48(suppl 60): PA4358.
[14] Gross JB, Bachenberg KL, Benumof JL, et al. Practice guidelines for the perioperative management of patients with obstructive sleep apnea: a report by the American Society of Anesthesiologists Task Force on Perioperative Management of patients with obstructive sleep apnea[J]. Anesthesiology, 2006, 104(5): 1081-1093;quiz 1117-1118. doi: 10.1097/00000542-200605000-00026
[15] Tsai JD, Chen HJ, Ku MS, et al. Association between allergic disease, sleep-disordered breathing, and childhood nocturnal enuresis: a population-based case-control study[J]. Pediatr Nephrol, 2017, 32(12): 2293-2301. doi: 10.1007/s00467-017-3750-0
[16] Kovacevic L, Wolfe-Christensen C, Lu H, et al. Adenotonsillectomy improves quality of life in children with sleep-disordered breathing regardless of nocturnal enuresis outcome[J]. J Pediatr Urol, 2015, 11(5): 269. e1-269. e5. doi: 10.1016/j.jpurol.2015.03.021
[17] Davaro F, Kaba A, Osei H, et al. Treatment of obstructive sleep apnea does not treat primary nocturnal enuresis[J]. J Pediatr Urol, 2021, 17(2): 182. e1-182182. e6. doi: 10.1016/j.jpurol.2020.12.022
[18] Marin-Oto M, Vicente EE, Marin JM. Long term management of obstructive sleep apnea and its comorbidities[J]. Multidiscip Respir Med, 2019, 14: 21. doi: 10.1186/s40248-019-0186-3
[19] Cummings JM, Rodning CB. Urinary stress incontinence among obese women: review of pathophysiology therapy[J]. Int Urogynecol J Pelvic Floor Dysfunct, 2000, 11(1): 41-44. doi: 10.1007/s001920050008
[20] Ma YL, Shen Y, Liu XM. Association between enuresis and obesity in children with primary monosymptomatic nocturnal enuresis[J]. Int Braz J Urol, 2019, 45(4): 790-797. doi: 10.1590/s1677-5538.ibju.2018.0603
[21] Mellin AE, Neumark-Sztainer D, Story M, et al. Unhealthy behaviors and psychosocial difficulties among overweight adolescents: the potential impact of familial factors[J]. J Adolesc Health, 2002, 31(2): 145-153. doi: 10.1016/S1054-139X(01)00396-2
[22] Kovacevic L, Jurewicz M, Dabaja A, et al. Enuretic children with obstructive sleep apnea syndrome: should they see otolaryngology first?[J]. J Pediatr Urol, 2013, 9(2): 145-150. doi: 10.1016/j.jpurol.2011.12.013
[23] Fujiwara J, Kimura S, Tsukayama H, et al. Evaluation of the autonomic nervous system function in children with primary monosymptomatic nocturnal enuresis: power spectrum analysis of heart rate variability using 24-hour Holter electrocardiograms[J]. Scand J Urol Nephrol, 2001, 35(5): 350-356. doi: 10.1080/003655901753224396
[24] Bascom A, McMaster MA, Alexander RT, et al. Nocturnal enuresis in children is associated with differences in autonomic control[J]. Sleep, 2019, 42(3): zsy239.
-

计量
- 文章访问数: 213
- 施引文献: 0



 下载:
下载: