Clinical efficacy of robot-assisted laparoscopic transvesical radical prostatectomy in the treatment of locally advanced prostate cancer
-
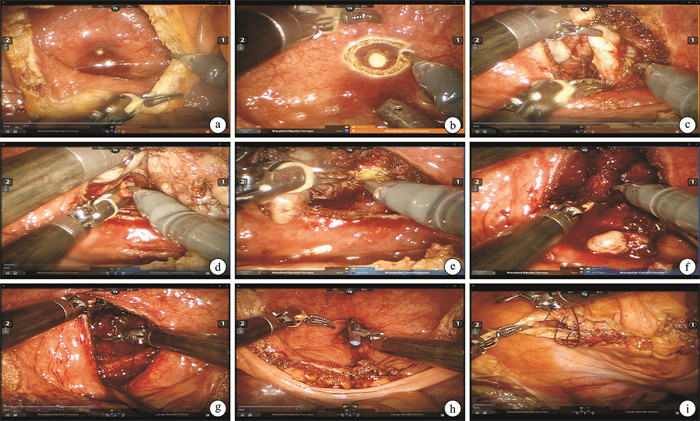
摘要: 目的 探讨局部晚期前列腺癌在新辅助内分泌治疗后行经膀胱入路机器人辅助腹腔镜根治性前列腺切除术(robotic assisted radical prostatectomy,RARP)的可行性和短期临床疗效。方法 回顾性分析2021年1月—2023年8月南昌大学第一附属医院收治的75例局部晚期前列腺癌行经膀胱入路RARP的患者资料。患者初诊前列腺特异性抗原(prostate-specific antigen,PSA)14.1~182.8 ng/mL,平均(52.5±23.9) ng/mL,术前均接受3~6个月新辅助内分泌治疗后,PSA水平降低至0.01~4.20 ng/mL,平均(0.6±0.2) ng/mL,再行经膀胱入路RARP和扩大盆腔淋巴结清扫术。记录患者围术期情况并随访患者术后PSA及尿控情况。结果 75例患者经膀胱入路RARP和扩大盆腔淋巴结清扫术均顺利完成,无中转开放手术。手术时间为90~150 min,中位手术时间120 min;术中出血量为50~300 mL,中位出血量150 mL;术后住院时间为3~7 d,平均(4.7±0.8) d;术后引流管留置时间为3~6 d,平均(3.5±0.3) d,导尿管留置时间为10~14 d。无直肠损伤和神经损伤等术中并发症。术后病理提示14例患者切缘阳性,阳性率为18.7%;盆腔淋巴结清扫数目12~25枚,中位数16枚;25例患者有阳性淋巴结。随访时间12~32个月,术后1~3个月复查PSA为0.001~0.050 ng/mL。术后即刻、3个月、6个月和12个月尿控率分别为62.7%、85.3%、92.0%和97.3%。4例患者出现生化复发,其余患者未出现局部复发和远处转移。结论 局部晚期前列腺癌行术前新辅助内分泌治疗有助于缩瘤降期,降低手术难度,经膀胱入路RARP治疗局部晚期前列腺癌是安全可行的,有较满意的肿瘤控制和早期尿控恢复效果,未来仍需多中心、大样本研究进一步验证。Abstract: Objective To explore the feasibility and short-term clinical efficacy of robot-assisted laparoscopic radical prostatectomy(RARP) via transvesical approach for locally advanced prostate cancer after neoadjuvant hormone therapy.Methods The data of 75 patients with locally advanced prostate cancer who underwent transvesical approach RARP in the First Affiliated Hospital of Nanchang University from January 2021 to August 2023 were retrospectively analyzed. The prostate-specific antigen(PSA) of the patients at initial diagnosis was 14.1-182.8 ng/mL, with an average of (52.5±23.9) ng/mL. After 3-6 months of neoadjuvant hormone therapy before surgery, the PSA decreased to 0.01-4.20 ng/mL, with an average of (0.6±0.2) ng/mL, and then transvesical approach RARP and extended pelvic lymph node dissection were performed. The perioperative data of the patients were recorded, and the postoperative PSA and urinary control of the patients were followed up.Results Transvesical approach RARP and extended pelvic lymph node dissection were successfully completed in 75 patients, without conversion to open surgery. The operation time was 90-150 minutes, with a median operation time of 120 minutes; the intraoperative blood loss was 50-300 mL, with a median blood loss of 150 mL; the postoperative hospital stay was 3-7 days, with an average of (4.7±0.8) days; the postoperative drainage tube retention time was 3-6 days, with an average of (3.5±0.3) days, and the catheter retention time was 10-14 days. There were no intraoperative complications such as rectal injury or nerve injury. Postoperative pathology showed that 14 patients had positive resection margins, with a positive rate of 18.7%. The number of pelvic lymph nodes dissected was 12-25, with a median of 16, and positive lymph nodes were found in 25 patients. The follow-up time was 12-32 months, and PSA was rechecked 1-3 months after surgery, with a PSA of 0.001-0.050 ng/mL. The urinary control rates were 62.7%, 85.3%, 92.0% and 97.3% immediately after surgery, 3 months, 6 months and 12 months, respectively. Biochemical recurrence occurred in 4 cases, and no local recurrence or distant metastasis was observed in the other patients.Conclusion Preoperative neoadjuvant hormone therapy for locally advanced prostate cancer can help reduce tumor size and stage, and reduce the difficulty of surgery. Transvesical RARP for locally advanced prostate cancer is safe and feasible, with satisfactory tumor control and early urinary control recovery effects. Multicenter, large-sample studies are still needed to further verify this in the future.
-
Key words:
- prostate cancer /
- robotic surgery /
- local advanced /
- transvesical /
- neoadjuvant hormone therapy
-

-
[1] 李星, 曾晓勇. 中国前列腺癌流行病学研究进展[J]. 肿瘤防治研究, 2021, 48(1): 98-102.
[2] Liu J, Dong L, Zhu Y, et al. Prostate cancer treatment-China's perspective[J]. Cancer Lett, 2022, 550: 215927. doi: 10.1016/j.canlet.2022.215927
[3] Chen R, Ren S, Chinese Prostate Cancer Consortium, et al. Prostate cancer in Asia: A collaborative report[J]. Asian J Urol, 2014, 1(1): 15-29. doi: 10.1016/j.ajur.2014.08.007
[4] 袁令兴, 娄庆艳, 徐英民, 等. 新辅助内分泌治疗联合腹腔镜前列腺癌根治术治疗高危及局部晚期前列腺癌的临床研究[J]. 临床泌尿外科杂志, 2019, 34(10): 801-803, 808. https://lcmw.whuhzzs.com/article/doi/10.13201/j.issn.1001-1420.2019.10.010
[5] 汪雄, 周佳维, 刘志, 等. 新辅助内分泌治疗联合腹腔镜前列腺癌根治术治疗局部进展期前列腺癌的优势[J]. 国际泌尿系统杂志, 2023, 43(5): 795-798. doi: 10.3760/cma.j.cn431460-20210908-00204
[6] Qian H, Chi C, Tricard T, et al. A Prospective Randomized Trial of Neoadjuvant Chemohormonal Therapy vs Hormonal Therapy in Locally Advanced Prostate Cancer Treated by Radical Prostatectomy[J]. J Urol, 2024, 211(5): 648-655. doi: 10.1097/JU.0000000000003876
[7] 周晓晨, 傅斌, 张成, 等. 经膀胱入路机器人辅助根治性前列腺切除术的短期疗效分析[J]. 中华泌尿外科杂志, 2019, 40(2): 127-131.
[8] Zhou X, Fu B, Zhang C, et al. Transvesical robot-assisted radical prostatectomy: initial experience and surgical outcomes[J]. BJU Int, 2020, 126(2): 300-308. doi: 10.1111/bju.15111
[9] 周晓晨, 胡兵, 傅斌, 等. 3种机器人辅助腹腔镜根治性前列腺切除术手术入路对比研究: 前入路、后入路及经膀胱入路[J]. 临床泌尿外科杂志, 2019, 34(7): 501-506. https://lcmw.whuhzzs.com/article/doi/10.13201/j.issn.1001-1420.2019.07.001
[10] 周晓晨, 张成, 傅斌, 等. 单孔经膀胱机器人根治性前列腺切除术: 一种保护术后尿控的新术式[J]. 机器人外科学杂志, 2020, 35(1): 11-17.
[11] 程晓锋, 许嵩, 周晓晨, 等. 寡转移性PCa新辅助内分泌治疗后RARP与仅行RARP的短期临床疗效对比[J]. 临床泌尿外科杂志, 2021, 36(8): 627-632. https://lcmw.whuhzzs.com/article/doi/10.13201/j.issn.1001-1420.2021.08.008
[12] Saika T, Miura N, Fukumoto T, et al. Role of robot-assisted radical prostatectomy in locally advanced prostate cancer[J]. Int J Urol, 2018, 25(1): 30-35. doi: 10.1111/iju.13441
[13] Gandaglia G, De Lorenzis E, Novara G, et al. Robot-assisted Radical Prostatectomy and Extended Pelvic Lymph Node Dissection in Patients with Locally-advanced Prostate Cancer[J]. Eur Urol, 2017, 71(2): 249-256. doi: 10.1016/j.eururo.2016.05.008
[14] 赵浩辰, 鲍一歌, 杨璐, 等. 机器人辅助根治性前列腺切除术中相关解剖结构的保留方法及策略进展[J]. 临床泌尿外科杂志, 2024, 39(8): 692-695. https://lcmw.whuhzzs.com/article/doi/10.13201/j.issn.1001-1420.2024.08.008
[15] 中国经膀胱入路机器人辅助根治性前列腺切除术专家协作组. 经膀胱入路机器人辅助根治性前列腺切除术中国专家共识(2021版)[J]. 机器人外科学杂志(中英文), 2022, 3(2): 149-160.
[16] Chen WH, Lee YK, Kuo HC, et al. Oncological and functional outcomes of high-risk and very high-risk prostate cancer patients after robot-assisted radical prostatectomy[J]. PLoS One, 2023, 18(3): e0282494.
[17] Qiu X, Li Y, Chen M, et al. Retzius-sparing robot-assisted radical prostatectomy improves early recovery of urinary continence: a randomized, controlled, single-blind trial with a 1-year follow-up[J]. BJU Int, 2020, 126(5): 633-640.
[18] Pu XY, Wang XH, Wu YL, et al. Comparative study of the impact of 3-versus 8-month neoadjuvant hormonal therapy on outcome of laparoscopic radical prostatectomy[J]. J Cancer Res Clin Oncol, 2007, 133(8): 555-562.
[19] Abdollah F, Gandaglia G, Suardi N, et al. More extensive pelvic lymph node dissection improves survival in patients with node-positive prostate cancer[J]. Eur Urol, 2015, 67(2): 212-219. http://www.onacademic.com/detail/journal_1000036311913710_c1cc.html
[20] Moschini M, Fossati N, Abdollah F, et al. Determinants of long-term survival of patients with locally advanced prostate cancer: the role of extensive pelvic lymph node dissection[J]. Prostate Cancer Prostatic Dis, 2016, 19(1): 63-67.
-




 下载:
下载: