Analysis of risk factors and construction of risk prediction model for biochemical recurrence after radical prostatectomy
-
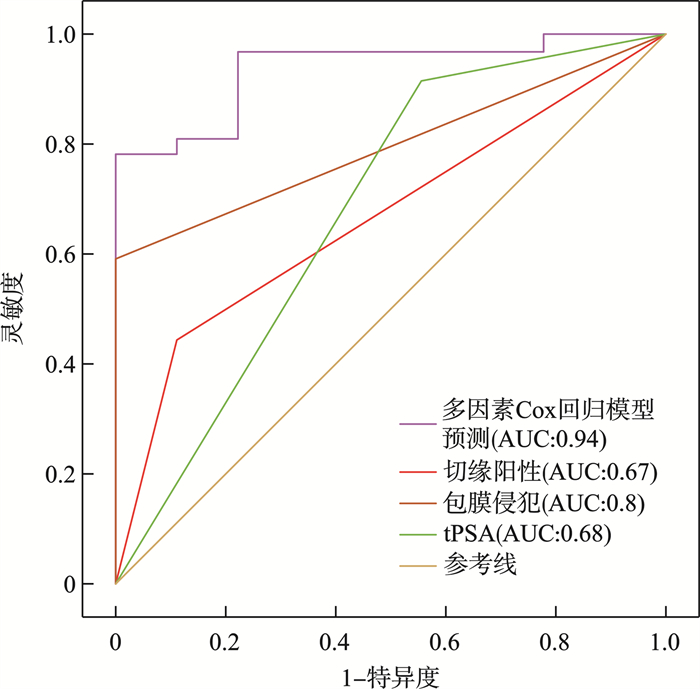
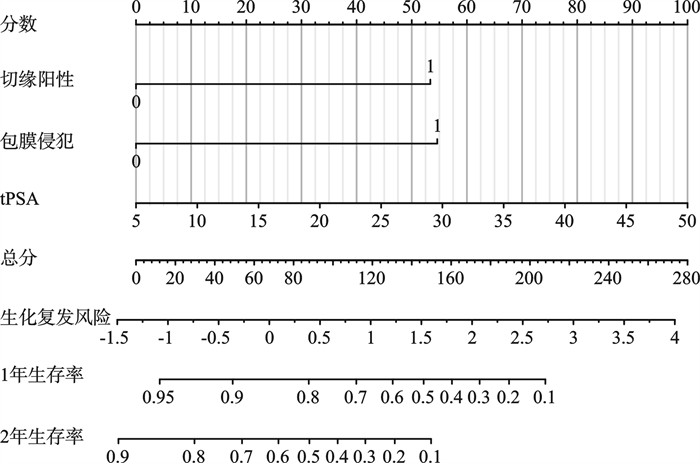
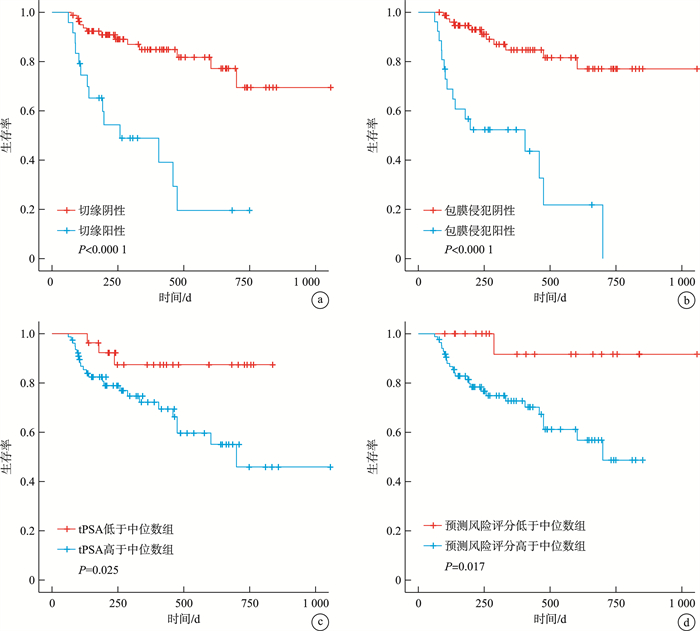
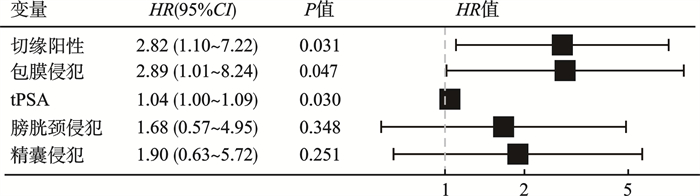
摘要: 目的 分析前列腺癌根治术后生化复发的危险因素并构建风险预测模型。方法 回顾性分析2020年6月—2023年6月在我院治疗的105例前列腺癌患者的临床资料,使用单因素和多因素Cox回归模型分析生化复发事件的影响因素并进行模型评价,构建风险预测方程和列线图预测生化复发的风险,最后对单个独立危险因素和多因素风险预测模型进行生存分析。结果 共纳入患者105例,其中生化复发27例(25.7%),中位生化复发时间140(100,310) d。单因素Cox回归模型发现7个指标均是生化复发的危险因素,通过逐步回归建立多因素Cox回归模型,结果显示切缘阳性(HR=2.82,95%CI:1.10~7.22,P=0.031)、包膜侵犯(HR=2.89,95%CI:1.01~8.24,P=0.047)、术前总前列腺特异性抗原(total prostate specific antigen,tPSA)(HR=1.04,95%CI:1.00~1.09,P=0.030)均为前列腺癌根治术后生化复发的独立危险因素。受试者工作特征(receiver operating characteristic,ROC)曲线表明风险预测模型的预测效果显著优于单个独立危险因素。生存分析的Kaplan-Meier曲线图表明单个独立危险因素及风险预测模型不同分组的生存率均有显著差异。结论 切缘阳性、包膜侵犯、术前tPSA是前列腺癌根治术后生化复发的独立危险因素和独立预后因子,构建的风险预测方程和列线图能有效预测生化复发的风险,对前列腺癌根治术后患者预测生化复发及个体化诊疗具有重要意义。Abstract: Objective To analyze the risk factors in biochemical recurrence after radical prostatectomy and to construct a risk prediction model.Methods The clinical data of 105 patients with prostate cancer treated in ours hospital from June 2020 to June 2023 were retrospectively analyzed. Univariate and multivariate Cox regression models were used to analyze the influencing factors in biochemical recurrence events and model evaluation was performed. The risk prediction equation and nomogram were constructed to predict the risk of biochemical recurrence. Finally, the survival analysis of single independent risk factor and multi-factor risk prediction model was carried out.Results A total of 105 patients were included, of which 27(25.7%) had biochemical recurrence, with a median biochemical recurrence time of 140(100, 310) days. Univariate Cox regression model found that 7 indicators were risk factors in biochemical recurrence. Multivariate Cox regression model was established by stepwise regression. The results showed that positive resection margin(HR=2.82, 95%CI: 1.10-7.22, P=0.031), capsular invasion(HR=2.89, 95%CI: 1.01-8.24, P=0.047), preoperative total prostate specific antigen(tPSA)(HR=1.04, 95%CI: 1.00-1.09, P=0.030) were independent risk factors in biochemical recurrence after radical prostatectomy. The ROC curve showed that the prediction effect of the risk prediction model was significantly better than that of a single independent risk factor. The Kaplan-Meier curve of survival analysis showed that survival rates in the different groups of three independent risk factors and risk prediction models were significantly different.Conclusion Positive resection margin, capsular invasion and preoperative tPSA are independent risk factors and independent prognostic factors in biochemical recurrence after radical prostatectomy. The constructed risk prediction equation and nomogram can effectively predict the risk of biochemical recurrence, which is of great significance for predicting biochemical recurrence and individualized diagnosis and treatment of patients after radical prostatectomy.
-
Key words:
- prostate cancer /
- radical prostatectomy /
- biochemical recurrence /
- Cox regression /
- survival analysis /
- nomogram
-

-
表 1 患者临床基线资料
例(%),X±S,M(Q1,Q3) 变量 总例数(105例) 未生化复发组(78例) 生化复发组(27例) 年龄/岁 69.7±6.0 69.7±6.3 69.7±5.3 前列腺体积/mL 43.8(31.3,62.4) 41.7(29.5,58.8) 47.9(40.9,74.7) tPSA/(ng/mL) 15.2(10.0,25.7) 12.7(8.7,20.9) 24.8(17.8,32.4) BMI/(kg/m2) 24.1±2.4 24.3±2.4 23.3±2.2 淋巴结侵犯 阴性 89(84.8) 73(93.6) 16(59.3) 阳性 16(15.2) 5(6.4) 11(40.7) 精囊侵犯 阴性 75(71.4) 66(84.6) 9(33.3) 阳性 30(28.6) 12(15.4) 18(66.7) 切缘 阴性 81(77.1) 68(87.2) 13(48.1) 阳性 24(22.9) 10(12.8) 14(51.9) 膀胱颈侵犯 阴性 95(90.5) 76(97.4) 19(70.4) 阳性 10(9.5) 2(2.6) 8(29.6) 包膜侵犯 阴性 79(75.2) 68(87.2) 11(40.7) 阳性 26(24.8) 10(12.8) 16(59.3) 脉管侵犯 阴性 70(66.7) 59(75.6) 11(40.7) 阳性 35(33.3) 19(24.4) 16(59.3) 神经侵犯 阴性 23(21.9) 21(26.9) 2(7.4) 阳性 82(78.1) 57(73.1) 25(92.6) 术后Gleason评分 ≤7 60(57.1) 54(69.2) 6(22.2) ≥8 45(42.9) 24(30.8) 21(77.8) 表 2 单因素Cox回归模型
变量 HR(95%CI) Cox回归P值 PH检验P值 年龄 1.003(0.942~1.067) 0.931 0.693 前列腺体积 1.011(0.997~1.025) 0.128 0.207 tPSA 1.056(1.027~1.087) < 0.001 0.453 BMI 0.855(0.714~1.024) 0.088 0.220 淋巴结侵犯 4.442(2.058~9.587) < 0.001 0.992 精囊侵犯 6.556(2.932~14.662) < 0.001 0.688 切缘阳性 5.459(2.539~11.740) < 0.001 0.903 膀胱颈侵犯 9.602(4.010~22.992) < 0.001 0.630 包膜侵犯 6.860(3.147~14.953) < 0.001 0.683 脉管侵犯 2.654(1.229~5.730) 0.013 0.597 神经侵犯 3.820(0.904~16.130) 0.068 0.083 术后Gleason评分 5.515(2.224~13.677) < 0.001 0.038 表 3 既往报道生化复发的独立危险因素
作者 时间 独立危险因素 刘建华等[8] 2020年 术前PSA水平高、病理分期高、手术切缘阳性、包膜侵犯阳性、淋巴结转移、精囊侵犯阳性、术前Gleason评分 范宇等[ 6 ]2021年 临床治愈、术后病理分期 马帅军等[7] 2022年 年龄≥70岁、初始PSA>20 ng/mL、≥pT3期、穿刺Gleason评分≥7分 严于昊等[ 9 ]2022年 PSA≥23.25 ng/mL、穿刺Gleason评分≥4+3分、术后Gleason评分升级、病理淋巴结阳性、精囊侵犯 田超等[12] 2022年 术前Gleason评分、术后Gleason评分、精囊侵犯、淋巴结侵犯、切缘阳性、术前PSA水平 陈剑等[ 5 ]2023年 病理高分期(≥pT3期)、切缘阳性、淋巴结侵犯、营养风险指数≤106.9 李林[10] 2023年 穿刺Gleason评分、切缘阳性、精囊侵犯 史鉴修[ 11 ]2023年 术前PSA>20 ng/mL、Gleason评分≥8分 -
[1] Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries[J]. CA Cancer J Clin, 2021, 71(3): 209-249. doi: 10.3322/caac.21660
[2] Van den Broeck T, van den Bergh RCN, Arfi N, et al. Prognostic value of biochemical recurrence following treatment with curative intent for prostate cancer: a systematic review[J]. Eur Urol, 2019, 75(6): 967-987. doi: 10.1016/j.eururo.2018.10.011
[3] 黄健, 张旭. 中国泌尿外科和男科疾病诊断治疗指南: 2022版[M]. 北京: 科学出版社, 2022.
[4] van den Broeck T, van den Bergh RCN, Briers E, et al. Biochemical recurrence in prostate cancer: the European association of urology prostate cancer guidelines panel recommendations[J]. Eur Urol Focus, 2020, 6(2): 231-234. doi: 10.1016/j.euf.2019.06.004
[5] 陈剑, 陈启铭, 汪泽, 等. 前列腺癌根治术后生化复发的危险因素分析[J]. 陆军军医大学学报, 2023, 45(18): 1955-1964.
[6] 范宇, 叶林·木拉提, 梁磊, 等. 根治性前列腺切除术后影响患者临床治愈和生化复发的危险因素分析[J]. 中华泌尿外科杂志, 2021, 42(9): 644-649. doi: 10.3760/cma.j.cn112330-20210720-00379
[7] 马帅军, 张景良, 苏醒, 等. 根治性前列腺切除术后生化复发的危险因素分析[J]. 中华泌尿外科杂志, 2022, 43(1): 35-39. doi: 10.3760/cma.j.cn112330-20210722-00388
[8] 刘建华, 张会朋, 黄随富, 等. 腹腔镜前列腺癌根治术患者1年内生化复发的影响因素分析[J]. 中国实用医刊, 2020, 47(6): 38-40. doi: 10.3760/cma.j.cn115689-20191108-08020
[9] 严于昊, 胡广漠, 谢超, 等. 前列腺癌生化复发危险因素报告: 单中心11年回顾分析[J]. 现代泌尿生殖肿瘤杂志, 2022, 14(3): 150-155. doi: 10.3870/j.issn.1674-4624.2022.03.005
[10] 李林. 高危前列腺癌术后生化复发高危因素研究及预后模型的建立[D]. 昆明: 昆明医科大学, 2023.
[11] 史鉴修. 机器人辅助腹腔镜根治性前列腺切除术后生化复发的危险因素及新辅助内分泌治疗对生化复发影响的研究[D]. 沈阳: 中国医科大学, 2023.
[12] 田超, 曹正国, 韩庆杰, 等. 基于潜在类别分析的不同PSA水平前列腺癌患者术后生化复发影响因素分布[J]. 临床泌尿外科杂志, 2022, 37(7): 537-542. https://lcmw.whuhzzs.com/article/doi/10.13201/j.issn.1001-1420.2022.07.010
[13] Yang CW, Wang HH, Hassouna MF, et al. Prediction of a positive surgical margin and biochemical recurrence after robot-assisted radical prostatectomy[J]. Sci Rep, 2021, 11(1): 14329. doi: 10.1038/s41598-021-93860-y
[14] 陶军跃, 梁朝朝, 周骏. 前列腺癌根治术后切缘阳性的诊疗进展[J]. 临床泌尿外科杂志, 2023, 38(3): 232-237. https://lcmw.whuhzzs.com/article/doi/10.13201/j.issn.1001-1420.2023.03.017
[15] Zhang B, Zhou J, Wu S, et al. The impact of surgical margin status on prostate cancer-specific mortality after radical prostatectomy: a systematic review and meta-analysis[J]. Clin Transl Oncol, 2020, 22(11): 2087-2096. doi: 10.1007/s12094-020-02358-y
[16] Shore ND, Moul JW, Pienta KJ, et al. Biochemical recurrence in patients with prostate cancer after primary definitive therapy: treatment based on risk stratification[J]. Prostate Cancer Prostatic Dis, 2024, 27(2): 192-201. doi: 10.1038/s41391-023-00712-z
-

计量
- 文章访问数: 74
- 施引文献: 0



 下载:
下载: