Prognostic impact of cytoreductive nephrectomy on patients with bone metastases from renal cancer: an analysis based on the SEER database
-
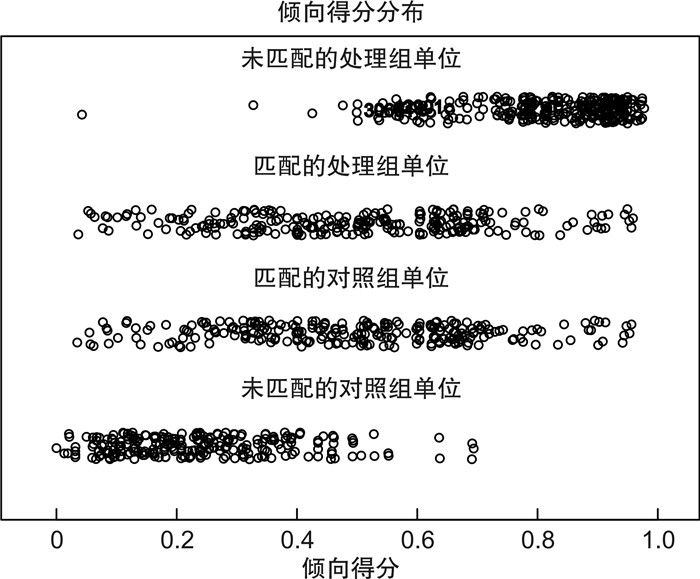
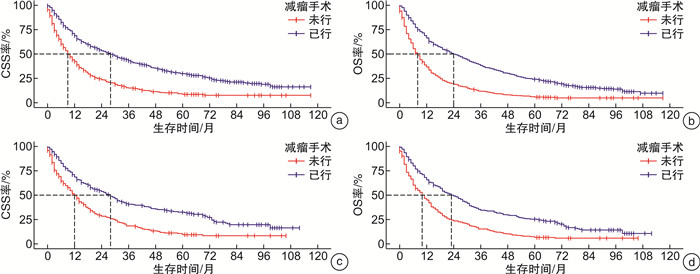
摘要: 目的 探究减瘤手术对肾癌骨转移患者生存预后的影响,为临床决策提供参考。方法 本研究基于监测、流行病学和最终结果(surveillance,epidemiology,and end results,SEER)数据库分析,从数据库中收集大量多中心的肾癌患者的临床数据,分别通过logistic法分析了肾癌患者的骨转移的危险因素、Kaplan-Meier法绘制骨转移与非骨转移患者的生存曲线,Cox分析骨转移患者的预后影响因素,并使用倾向性评分匹配法去除混杂因素后分析了减瘤手术对肾癌骨转移患者的预后影响。结果 本研究共纳入41 221例肾癌患者,其中1 038例发生了骨转移,通过对比,骨转移患者呈现以下临床特征:男性、年龄偏高、T分期较晚、多数合并淋巴结及其他器官转移。logistic分析结果显示肾癌骨转移的独立风险因素有:T分期高、合并淋巴结及其他远处器官转移。生存分析显示骨转移患者生存期远低于未转移患者。Cox回归分析显示高龄、T4、N1、远处转移是影响生存的独立危险因素,减瘤手术为独立保护因素。倾向性评分匹配后减瘤手术仍然是影响肾癌骨转移患者预后的独立保护因素。结论 肾癌患者发生骨转移的风险因素包括T4肿瘤分期和肺转移。T4肿瘤分期和淋巴结转移通常预示预后不良。减瘤手术对患者生存预后的影响稳定,肾癌骨转移的患者可以通过减瘤手术获得生存获益。Abstract: Objective To investigate the effect of cytoreductive nephrectomy on the survival prognosis of patients with bone metastases from renal cancer, and to provide reference for clinical decision-making.Methods In this study, a large number of clinical data of renal cancer patients from multiple centers were collected based on the SEER database. The risk factors in bone metastases for patients with RCC were analyzed by the logistic method, and the survival curves of patients with bone metastases versus those with non-bone metastases were plotted by the Kaplan-Meier method. Prognostic influences on patients with bone metastases were analyzed by the Cox. The prognostic impact of cytoreductive nephrectomy on RCC-BM patients was analyzed after removing confounding factors.Results A total of 41 221 renal cancer patients were included in this study, of which 1 038 had bone metastases. By comparison, patients with bone metastases presented the following clinical characteristics: male, old age, late T stage, and most of them combined with lymph node and other organ metastases. Logistic analysis showed that the independent risk factors in bone metastases of renal cancer were: high T stage, combined with lymph node and other distant organ metastases. Survival analysis showed that the survival of bone metastases was much lower than that of patients without metastases. Cox regression analysis showed that advanced age, T4, N1, and distant metastases were independent risk factors affecting survival, and cytoreductive nephrectomy was an independent protective factor. Cytoreductive nephrectomy remained an independent protective factor affecting the prognosis of patients with RCC-BM after PSM.Conclusion Risk factors in bone metastases for patients with kidney cancer include T4 tumor stage and lung metastases. T4 tumor stage and lymph node metastases usually portend a poor prognosis. Tumor reduction surgery has a stable impact on survival prognosis, and patients with bone metastases from renal cancer can receive a survival benefit from cytoreductive nephrectomy.
-

-
表 1 入组患者统计基线表
例(%) 变量 有BM (1 038例) 无BM (40 183例) P值 变量 有BM (1 038例) 无BM (40 183例) P值 性别 < 0.001 T分期 < 0.001 女 304(29.3) 14 417(35.9) T1 300(28.9) 28 419(70.7) 男 734(70.7) 25 766(64.1) T2 226(21.8) 4 078(10.1) 年龄/岁 0.003 T3 411(39.6) 7 217(18.0) ≤58 352(33.9) 15 551(38.7) T4 101(9.7) 469(1.2) 59~76 553(53.3) 20 340(50.6) N分期 < 0.001 ≥77 133(12.8) 4 292(10.7) N0 738(71.1) 39 103(97.3) 人种 0.041 N1 300(28.9) 1 080(2.7) 美洲人 9(0.9) 396(1.0) 手术信息 < 0.001 亚洲人 54(5.2) 2 339(5.8) 未行手术 484(46.6) 1 767(4.4) 黑种人 85(8.2) 4 301(10.7) 其他 3(0.3) 23(0.1) 白种人 890(85.7) 33 147(82.5) 肿瘤切除 544(52.4) 37 134(92.4) 婚姻状态 0.850 微创手术 7(0.7) 1 259(3.1) 离婚 106(10.2) 3 837(9.5) 化疗信息 < 0.001 已婚 674(64.9) 25 985(64.7) 无 379(36.5) 38 528(95.9) 分居 9(0.9) 476(1.2) 有 659(63.5) 1 655(4.1) 未婚 164(15.8) 6 590(16.4) 肝转移 < 0.001 同居 2(0.2) 149(0.4) 无 913(88.0) 39 895(99.3) 丧偶 83(8.0) 3 146(7.8) 有 125(12.0) 288(0.7) 肿瘤位置 0.012 脑转移 < 0.001 双侧 1(0.1) 24(0.1) 无 932(89.8) 39 970(99.5) 左侧 554(53.4) 19 694(49.0) 有 106(10.2) 213(0.5) 右侧 483(46.5) 20 465(50.9) 肺转移 < 0.001 肿瘤大小/mm < 0.001 无 572(55.1) 38 847(96.7) ≤40 423(40.8) 24 078(59.9) 有 466(44.9) 1 336(3.3) 41~80 445(42.9) 13 666(34.0) ≥81 170(16.4) 2 439(6.1) 表 2 BM患者logistic回归分析
变量 单因素 多因素 OR(95%CI) P值 OR(95%CI) P值 年龄/岁 ≤58 参考 参考 59~76 1.20(1.05~1.38) < 0.05 1.12(0.97~1.30) 0.12 ≥77 1.37(1.12~1.68) < 0.05 1.35(1.08~1.68) < 0.01 性别 女 参考 参考 男 1.35(1.18~1.55) < 0.001 1.19(1.02~1.37) < 0.05 肿瘤大小/ mm ≤40 参考 参考 41~80 1.85(1.62~2.12) < 0.001 2.03(1.75~2.36) < 0.001 ≥81 3.97(3.30~4.76) < 0.001 1.50(1.21~1.86) < 0.001 T分期 T1 参考 T2 5.25(4.40~6.26) < 0.001 2.50(2.04~3.06) < 0.001 T3 5.39(4.64~6.27) < 0.001 2.15(1.81~2.56) < 0.001 T4 20.40(16.00~26.02) < 0.001 2.91(2.15~3.94) < 0.001 N分期 N0 参考 参考 N1 14.72(12.70~17.05) < 0.001 3.40(2.83~4.08) < 0.001 肝转移 无 参考 参考 有 18.97(15.22~23.63) < 0.001 2.26(1.73~2.95) < 0.001 脑转移 无 参考 参考 有 21.34(16.76~27.18) < 0.001 3.14(2.36~4.19) < 0.001 肺转移 无 参考 参考 有 23.69(20.72~27.08) < 0.001 8.10(6.83~9.61) < 0.001 表 3 影响RCC-BM肿瘤特异性生存预后相关因素的Cox回归分析
风险因素 单因素 多因素 HR 95%CI P值 HR 95%CI P值 肿瘤位置 双侧 参考 参考 左侧(原发) 0.08 0.01~0.63 < 0.05 0.17 0.02~1.29 0.08 右侧(原发) 0.09 0.01~0.68 < 0.05 0.19 0.02~1.42 0.10 手术信息 未行手术 参考 参考 其他 0.61 0.15~2.45 0.49 0.75 0.18~3.07 0.69 CN 0.46 0.40~0.54 < 0.001 0.53 0.45~0.62 < 0.001 消融 0.62 0.25~1.49 0.28 0.94 0.38~2.29 0.89 T分期 T1 参考 参考 T2 1.10 0.90~1.34 0.34 0.95 0.77~1.18 0.70 T3 1.08 0.91~1.29 0.35 1.08 0.90~1.31 0.37 T4 1.82 1.41~2.34 < 0.001 1.33 1.03~1.73 < 0.05 N分期 N0 参考 参考 N1 1.75 1.50~2.04 < 0.001 1.36 1.16~1.60 < 0.001 肝转移 无 参考 参考 有 1.82 1.48~2.24 < 0.001 1.23 0.99~1.53 0.06 脑转移 无 参考 参考 有 1.74 1.39~2.17 < 0.05 1.35 1.07~1.71 < 0.05 肺转移 无 参考 参考 有 1.92 1.67~2.22 < 0.001 1.56 1.33~1.82 < 0.001 表 4 影响RCC-BM总生存预后相关因素的Cox回归分析
变量 单因素 多因素 HR 95%CI P值 HR 95%CI P值 肿瘤位置 双侧 参考 参考 左侧(原发) 0.09 0.01~0.63 < 0.05 0.17 0.02~1.29 0.087 右侧(原发) 0.09 0.01~0.68 < 0.05 0.19 0.02~1.42 0.107 手术信息 未行手术 参考 参考 其他 0.61 0.15~2.45 0.49 0.75 0.18~3.07 0.696 CN 0.46 0.40~0.54 < 0.001 0.53 0.45~0.62 < 0.001 消融 0.62 0.25~1.49 0.289 0.94 0.38~2.29 0.892 T分期 T1 参考 参考 T2 1.10 0.90~1.34 0.345 0.95 0.77~1.18 0.701 T3 1.08 0.91~1.30 0.351 1.08 0.90~1.31 0.375 T4 1.82 1.42~2.35 < 0.001 1.33 1.03~1.73 < 0.05 N分期 N0 参考 参考 N1 1.75 1.51~2.05 < 0.001 1.36 1.16~1.60 < 0.001 肝转移 无 参考 参考 有 1.83 1.48~2.25 < 0.001 1.23 0.99~1.53 0.061 脑转移 无 参考 参考 有 1.74 1.39~2.17 < 0.05 1.35 1.07~1.71 < 0.05 肺转移 无 参考 参考 有 1.93 1.67~2.22 < 0.001 1.56 1.33~1.82 < 0.001 -
[1] Bukavina L, Bensalah K, Bray F, et al. Epidemiology of Renal Cell Carcinoma: 2022 Update[J]. Eur Urol, 2022, 82(5): 529-542. doi: 10.1016/j.eururo.2022.08.019
[2] Gupta K, Miller JD, Li JZ, et al. Epidemiologic and socioeconomic burden of metastatic renal cell carcinoma(mRCC): a literature review[J]. Cancer Treat Rev, 2008, 34(3): 193-205. doi: 10.1016/j.ctrv.2007.12.001
[3] Capitanio U, Bensalah K, Bex A, et al. Epidemiology of Renal Cell Carcinoma[J]. Eur Urol, 2019, 75(1): 74-84. doi: 10.1016/j.eururo.2018.08.036
[4] 王军, 侯亚信, 梁华庚, 等. 肾透明细胞癌合并单一肩胛骨转移1例[J]. 临床泌尿外科杂志, 2022, 37(8): 646-648. https://lcmw.whuhzzs.com/article/doi/10.13201/j.issn.1001-1420.2022.08.016
[5] Umer M, Mohib Y, Atif M, et al. Skeletal metastasis in renal cell carcinoma: a review[J]. Ann Med Surg(Lond), 2018, 27: 9-16. doi: 10.1016/j.amsu.2018.01.002
[6] Brozovich A, Garmezy B, Pan TH, et al. All bone metastases are not created equal: Revisiting treatment resistance in renal cell carcinoma[J]. J Bone Oncol, 2021, 31: 100399. doi: 10.1016/j.jbo.2021.100399
[7] Bex A, Ljungberg B, van Poppel H, et al. The Role of Cytoreductive Nephrectomy: European Association of Urology Recommendations in 2016[J]. Eur Urol, 2016, 70(6): 901-905. doi: 10.1016/j.eururo.2016.07.005
[8] Méjean A, Ravaud A, Thezenas S, et al. Sunitinib Alone or after Nephrectomy in Metastatic Renal-Cell Carcinoma[J]. N Engl J Med, 2018, 379(5): 417-427. doi: 10.1056/NEJMoa1803675
[9] Hankey BF, Ries LA, Edwards BK. The surveillance, epidemiology, and end results program: a national resource[J]. Cancer Epidemiol Biomarkers Prev, 1999, 8(12): 1117-1121.
[10] 何先东. 基于SEER数据库研究初诊肾癌发生肺转移的危险因素及预后因素[D]. 重庆: 中国人民解放军陆军军医大学, 2020.
[11] Pierorazio PM, McKiernan JM, McCann TR, et al. Outcome after cytoreductive nephrectomy for metastatic renal cell carcinoma is predicted by fractional percentage of tumour volume removed[J]. BJU Int, 2007, 100(4): 755-759. doi: 10.1111/j.1464-410X.2007.07108.x
[12] Moch H, Amin MB, Berney DM, et al. The 2022 World Health Organization classification of tumours of the urinary system and male genital organs: Part A: renal, penile, and testicular tumours[J]. Eur Urol, 2022, 82(5): 458-468. doi: 10.1016/j.eururo.2022.06.016
[13] Fan ZY, Huang ZH, Huang XH. Bone metastasis in renal cell carcinoma patients: risk and prognostic factors and nomograms[J]. J Oncol, 2021, 2021: 5575295.
[14] Vieweg J, Su Z, Dahm P, et al. Reversal of tumor-mediated immunosuppression[J]. Clin Cancer Res, 2007, 13(2 pt 2): 727s-732s.
[15] Wood SL, Brown JE. Skeletal metastasis in renal cell carcinoma: current and future management options[J]. Cancer Treat Rev, 2012, 38(4): 284-291. doi: 10.1016/j.ctrv.2011.06.011
[16] Ljungberg B, Albiges L, Abu-Ghanem Y, et al. European Association of Urology Guidelines on Renal Cell Carcinoma: The 2022 Update[J]. Eur Urol, 2022, 82(4): 399-410. doi: 10.1016/j.eururo.2022.03.006
[17] 肾癌骨转移专家共识编写组. 肾癌骨转移专家共识(2020版)[J]. 中华肿瘤杂志, 2020, 42(7): 537-542. doi: 10.3760/cma.j.cn112152-20200401-00292
[18] 吴珺, 陆爱东, 张乐萍, 等. 儿童核心结合因子相关性急性髓系白血病疗效及预后因素分析[J]. 中华血液学杂志, 2019, 40(1): 52-57. https://www.cnki.com.cn/Article/CJFDTOTAL-SYAZ202111043.htm
[19] Bassil B, Dosoretz DE, Prout GR Jr. Validation of the tumor, nodes and metastasis classification of renal cell carcinoma[J]. J Urol, 1985, 134(3): 450-454. doi: 10.1016/S0022-5347(17)47235-1
[20] Brouwer OR, Noe A, Olmos RA, et al. Lymphatic drainage from renal cell carcinoma along the thoracic duct visualized with SPECT/CT[J]. Lymphat Res Biol, 2013, 11(4): 233-238. doi: 10.1089/lrb.2013.0017
[21] Capitanio U, Leibovich BC. The rationale and the role of lymph node dissection in renal cell carcinoma[J]. World J Urol, 2017, 35(4): 497-506. doi: 10.1007/s00345-016-1886-3
[22] Ljungberg B, Albiges L, Abu-Ghanem Y, et al. European Association of Urology Guidelines on Renal Cell Carcinoma: The 2019 Update[J]. Eur Urol, 2019, 75(5): 799-810.
[23] Massari F, Di Nunno V, Gatto L, et al. Should CARMENA really change our attitude towards cytoreductive nephrectomy in metastatic renal cell carcinoma?A systematic review and meta-analysis evaluating cytoreductive nephrectomy in the era of targeted therapy[J]. Target Oncol, 2018, 13(6): 705-714.
[24] 郭博达. 减瘤性肾切除术对肾癌肝转移患者预后的影响研究[D]. 北京: 北京协和医学院, 2022.
[25] 韩超, 王立东, 张璐琛, 等. 探究原发灶减瘤术对肾细胞癌合并骨转移患者的生存获益[J]. 中日友好医院学报, 2023, 37(5): 267-271, 276, 321. https://www.cnki.com.cn/Article/CJFDTOTAL-ZRYH202305003.htm
[26] Ahern E, Smyth MJ, Dougall WC, et al. Roles of the RANKL-RANK axis in antitumour immunity-implications for therapy[J]. Nat Rev Clin Oncol, 2018, 15(11): 676-693.
[27] McIntosh AG, Umbreit EC, Holland LC, et al. Optimizing patient selection for cytoreductive nephrectomy based on outcomes in the contemporary era of systemic therapy[J]. Cancer, 2020, 126(17): 3950-3960.
[28] Abel EJ, Master VA, Spiess PE, et al. The selection for cytoreductive nephrectomy(SCREEN)score: improving surgical risk stratification by integrating common radiographic features[J]. Eur Urol Oncol, 2024, 7(2): 266-274.
[29] Marchioni M, Kriegmair M, Heck M, et al. Development of a Novel Risk Score to Select the Optimal Candidate for Cytoreductive Nephrectomy Among Patients with Metastatic Renal Cell Carcinoma. Results from a Multi-institutional Registry(REMARCC)[J]. Eur Urol Oncol, 2021, 4(2): 256-263.
-





 下载:
下载: