Predictive value of neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio in the prognosis of patients with muscular-invasive bladder cancer undergoing laparoscopic radical cystectomy
-
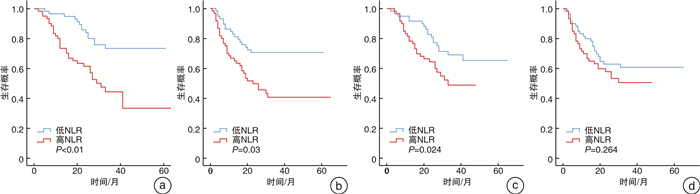
摘要: 目的 探讨术前中性粒细胞与淋巴细胞比值(NLR)、血小板与淋巴细胞比值(PLR)对行腹腔镜下膀胱癌根治术(LRC)的肌层浸润性膀胱癌(MIBC)患者预后的预测价值。方法 分析2016—2019年在我院行LRC的118例MIBC患者的临床资料,根据术前外周血NLR、PLR分为高NLR组(NLR≥2.33,58例)与低NLR组(NLR<2.33,60例)、高PLR组(PLR≥115.00,59例)与低PLR组(PLR<115.00,59例)。采用Kaplan-Meier、log-rank法单因素分析各临床病理特点对患者的生存预后的影响,并比较各组生存曲线差异,Cox多因素回归分析影响MIBC患者预后的危险因素。结果 高NLR、PLR与T分期及淋巴结转移相关,高PLR还与肿瘤体积相关,差异有统计学意义(P<0.05)。高NLR、PLR均能影响患者的OS,高NLR还与患者RFS相关,差异有统计学意义(P<0.05)。此外,多因素回归分析显示只有高NLR和T分期是影响患者OS和RFS的独立危险因素。结论 术前高NLR、PLR与行LRC的MIBC患者的不良预后相关,可作为MIBC患者预后的预测指标。Abstract: Objective To investigate the predictive value of preoperative neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR) in the prognosis of muscle-invasive bladder cancer (MIBC) following laparoscopic radical cystectomy (LRC).Methods We retrospectively analyzed 118 MIBC patients who underwent LRC in the Affiliated Provincial Hospital of Anhui Medical University from 2016 to 2019. The patients were divided into four groups, i. e. high NLR (NLR≥2.33, 58 cases) and low NLR (NLR < 2.33, 60 cases), high PLR (PLR≥115.00, 59 cases) and low PLR (PLR < 115.00, 59 cases). Kaplan-Meier and log-rank methods were used to analyze the impact of each clinicopathological feature on the survival and prognosis of patients. Differences in survival curves of each group were also compared. Cox multivariate regression analysis was used to analyze the risk factors that affect the prognosis of MIBC patients.Results High NLR and high PLR were significantly associated with pT stage and lymph node metastasis of bladder cancer (P< 0.05), and high PLR was also significantly associated with tumor volume (P< 0.05). Both high NLR and PLR showed significant impact on the patients' OS (P< 0.05), and high NLR was also significantly associated with the patients' RFS (P< 0.05). In addition, multivariate regression analysis revealed that high NLR and pT stage were independent risk factors for patients' OS and RFS.Conclusion Preoperative high NLR and high PLR are related to the poor prognosis of MIBC patients undergoing LRC, so they can be used as prognostic predictors in MIBC patients treated with LRC.
-

-
表 1 NLR、PLR与膀胱肿瘤患者的临床病例资料
例(%),X±S 危险因素 例数 NLR PLR NLR<2.33 (n=58) NLR≥2.33 (n=60) P值 PLR<115.00 (n=59) PLR≥115.00 (n=59) P值 年龄/岁 66.2±11.6 67.7±10.4 0.481 66.2±11.4 67.7±10.5 0.462 BMI 23.1±3.8 22.3±3.4 0.234 22.9±3.0 22.5±4.1 0.491 性别 男 104 50(86.2) 54(90.0) 0.524 53(89.9) 51(86.4) 0.569 女 14 8(13.8) 6(10.0) 6(10.1) 8(13.6) 吸烟 是 75 36(62.1) 39(65.0) 0.741 40(67.8) 35(59.3) 0.339 否 43 22(37.9) 21(35.0) 19(32.2) 24(40.7) 肿瘤单、多发 单发 89 40(69.0) 49(81.7) 0.109 42(71.1) 47(79.7) 0.285 多发 29 18(31.0) 11(18.3) 17(28.9) 12(20.3) 肿瘤大小 <3 cm 48 25(43.1) 23(38.3) 0.598 30(50.8) 18(30.5) 0.025 ≥3 cm 70 33(56.9) 37(61.7) 29(49.2) 41(69.5) 病理T分期 T2 89 49(84.5) 40(66.7) 0.025 50(84.7) 39(66.1) 0.019 T3~T4 29 9(15.5) 20(33.3) 9(15.3) 20(33.9) 淋巴结 阳性 21 5(8.6) 16(26.7) 0.010 6(10.2) 15(25.4) 0.030 阴性 97 53(91.4) 44(73.3) 53(89.8) 44(74.6) 表 2 Cox多因素分析
变量 OS RFS 95%可信区间 风险比 P值 95%可信区间 风险比 P值 吸烟 0.312~1.078 0.580 0.086 0.332~1.043 0.589 0.069 病理T分期 1.585~6.046 3.096 0.001 1.363~4.815 2.562 0.003 淋巴结转移 0.828~3.576 1.721 0.146 0.957~3.830 1.915 0.066 NLR 1.079~4.811 2.278 0.031 1.079~4.138 2.113 0.029 PLR 0.534~2.173 1.077 0.836 0.412~1.447 0.772 0.419 -
[1] Lenis AT, Lec PM, Chamie K, et al. Bladder Cancer: A Review[J]. JAMA, 2020, 324(19): 1980-1991. doi: 10.1001/jama.2020.17598
[2] Knowles MA, Hurst CD. Molecular biology of bladder cancer: new insights into pathogenesis and clinical diversity[J]. Nat Rev Cancer, 2015, 15(1): 25-41. doi: 10.1038/nrc3817
[3] 姜帅, 许培榕, 项卓仪, 等. 机器人辅助腹腔镜、传统腹腔镜和开放手术3种膀胱癌根治性全膀胱切除加回肠膀胱术的围手术期疗效比较[J]. 复旦学报(医学版), 2020, 47(1): 1-6. https://www.cnki.com.cn/Article/CJFDTOTAL-SHYK202001002.htm
[4] Zhang W, Wang R, Ma W, et al. Systemic immune-inflammation index predicts prognosis of bladder cancer patients after radical cystectomy[J]. Ann Transl Med, 2019, 7(18): 431. doi: 10.21037/atm.2019.09.02
[5] 李想. 腹腔镜与开放手术行膀胱癌根治性切除术的Meta分析[D]. 广西: 广西医科大学, 2015.
[6] Castelao JE, Yuan JM, Gago-Dominguez M, et al. Non-steroidal anti-inflammatory drugs and bladder cancer prevention[J]. Br J Cancer, 2000, 82(7): 1364-1369. doi: 10.1054/bjoc.1999.1106
[7] Ma X, Aoki T, Tsuruyama T, et al. Definition of Prostaglandin E2-EP2 Signals in the Colon Tumor Microenvironment That Amplify Inflammation and Tumor Growth[J]. Cancer Res, 2015, 75(14): 2822-2832. doi: 10.1158/0008-5472.CAN-15-0125
[8] Clatot F, Gouérant S, Mareschal S, et al. The gene expression profile of inflammatory, hypoxic and metabolic genes predicts the metastatic spread of human head and neck squamous cell carcinoma[J]. Oral Oncol, 2014, 50(3): 200-207. doi: 10.1016/j.oraloncology.2013.12.009
[9] Zheng J, Cai J, Li H, et al. Neutrophil to Lymphocyte Ratio and Platelet to Lymphocyte Ratio as Prognostic Predictors for Hepatocellular Carcinoma Patients with Various Treatments: a Meta-Analysis and Systematic Review[J]. Cell Physiol Biochem, 2017, 44(3): 967-981. doi: 10.1159/000485396
[10] 赵雅文, 董頔, 薛茜文, 等. 术前外周血中NLR、PLR、LMR与早期宫颈癌患者预后的相关性研究[J]. 新疆医科大学学报, 2020, 43(8): 997-1003. https://www.cnki.com.cn/Article/CJFDTOTAL-XJYY202008004.htm
[11] Song S, Chen H, Dou X, et al. The prognostic value of before treatment neutrophil-to-lymphocyte ratio in nasopharyngeal carcinoma[J]. Eur Arch Otorhinolaryngol, 2021.
[12] Tang X, Cao Y, Liu J, et al. Diagnostic and Predictive Values of Inflammatory Factors in Pathology and Survival of Patients Undergoing Total Cystectomy[J]. Mediators Inflamm, 2020, 2020: 9234067.
[13] Paijens ST, Vledder A, de Bruyn M, et al. Tumor-infiltrating lymphocytes in the immunotherapy era[J]. Cell Mol Immunol, 2021, 18(4): 842-859. doi: 10.1038/s41423-020-00565-9
[14] 毕海, 覃子健, 刘承, 等. 淋巴细胞/单核细胞比值对根治性膀胱全切患者生存预后的预测价值[J]. 临床泌尿外科杂志, 2021, 36(5): 342-347. http://lcmw.cbpt.cnki.net/WKC/WebPublication/paperDigest.aspx?paperID=5e4915c0-4d79-4c9a-ba20-bc37e3be0298
[15] Zhao Y, Shao Q, Peng G. Exhaustion and senescence: two crucial dysfunctional states of T cells in the tumor microenvironment[J]. Cell Mol Immunol, 2020, 17(1): 27-35. doi: 10.1038/s41423-019-0344-8
[16] Schlesinger M. Role of platelets and platelet receptors in cancer metastasis[J]. J Hematol Oncol, 2018, 11(1): 125. doi: 10.1186/s13045-018-0669-2
[17] Celik O, Akand M, Keskin MZ, et al. Preoperative neutrophil-to-lymphocyte ratio(NLR)may be predictive of pathologic stage in patients with bladder cancer larger than 3 cm[J]. Eur Rev Med Pharmacol Sci, 2016, 20(4): 652-656.
[18] Wang R, Yan Y, Liu S, et al. Comparison of Preoperative Neutrophil-Lymphocyte and Platelet-Lymphocyte Ratios in Bladder Cancer Patients Undergoing Radical Cystectomy[J]. Biomed Res Int, 2019, 2019: 3628384.
[19] Zhang J, Zhou X, Ding H, et al. The prognostic value of routine preoperative blood parameters in muscle-invasive bladder cancer[J]. BMC Urol, 2020, 20(1): 31. doi: 10.1186/s12894-020-00602-9
[20] 高峰, 宋东奎, 杨小明, 等. 中性粒细胞淋巴细胞比值与血小板淋巴细胞比值对肌层浸润性膀胱癌根治术后的预后价值[J]. 中华实验外科杂志, 2019, 36(7): 1185-1188. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGYK201907014.htm
[21] Kim M, Moon KC, Choi WS, et al. Prognostic value of systemic inflammatory responses in patients with upper urinary tract urothelial carcinoma[J]. World J Urol, 2015, 33(10): 1439-1457. doi: 10.1007/s00345-015-1484-9
-




 下载:
下载: