Diagnosis and treatment of metastatic renal tumor originating from lung cancer: analysis of 21 cases in a single center and review of the literature
-
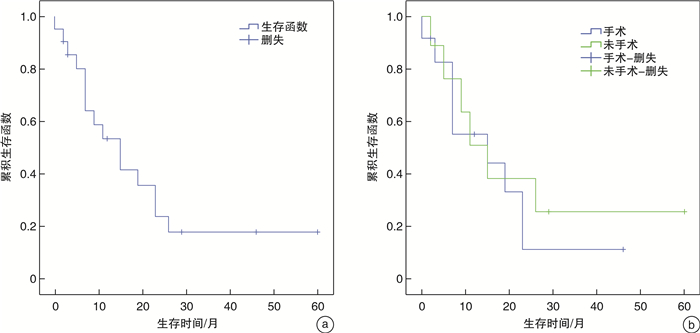
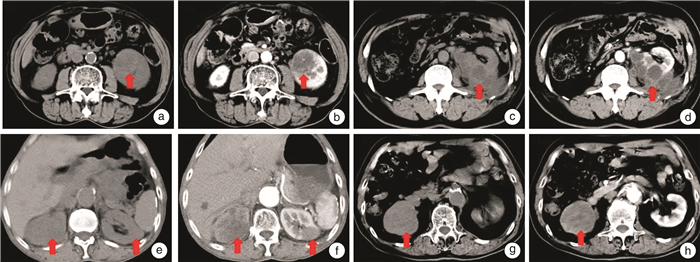
摘要: 目的 探讨肺癌肾脏转移的临床表现、诊断、治疗及预后特点。方法 回顾性收集2005年1月—2019年12月病理确诊为肺癌肾脏转移的病例21例。分析病例的临床特征、穿刺病理、治疗方式以及并发症情况等。对纳入的病例进行电话随访,记录患者的生存情况。计算患者总生存时间(OS),分析是否接受肾脏手术的2组患者OS的差异并分析其影响因素。结果 患者平均年龄为64.3岁,男性患者占81.0%。肺鳞癌10例,腺癌9例,腺鳞癌1例,小细胞肺癌1例。42.9%的患者有腰痛、血尿等临床表现,47.6%伴有其他部位的转移。从诊断肺癌到发现肾脏转移的平均时间间隔为21.9个月。增强CT诊断准确性为47.6%。76.2%的病灶为单侧,平均肿瘤大小为4.3 cm。11例患者行肾穿刺活检,其中有10例病理确诊肺癌。12例患者接受手术治疗。接受手术患者倾向于无其他部位转移的患者(P=0.019)。20例患者获得随访,平均随访时间34.2个月,共有6例患者存活,14例患者死亡。中位OS为15.0个月,其中行肾脏手术患者中位存活时间(15.0±8.1)个月,未行肾脏手术患者平均存活时间(15.0±4.1)个月,差异无统计学意义。结论 肺癌肾脏转移较为罕见,诊断、治疗相对困难,肾脏转移灶的手术治疗可能并不改善患者的预后。Abstract: Objective To investigate the clinical manifestation, diagnosis, treatment and prognosis of metastatic renal tumor originating from lung cancer.Methods Twenty-one cases of lung cancer with renal metastasis diagnosed by pathology from January 2005 to December 2019 were collected retrospectively. The demographic information, the occurrence time of renal metastasis, symptoms, CT imaging features, other site metastases, puncture pathology, operation and complications conditions were analyzed. The included cases were followed up by telephone and the survival conditions of the patients were recorded. The total survival time of the patients was calculated, and the difference of OS between the two groups of patients who underwent renal surgery or not was analyzed.Results The average age of the patients was 64.3 years old, and the male patients accounted for 81.0%. There were 10 cases of squamous cell carcinoma, 9 cases of adenocarcinoma, 1 case of adenosquamous carcinoma and 1 case of small cell lung cancer. Low back pain and hematuria were found in 42.9% of the patients. Other metastatic tumor was found in 47.6% of the patients. The interval between the diagnosis of lung cancer and the discovery of renal metastasis was 21.9 months. The accuracy of enhanced CT diagnosis was 47.6%. Unilateral lesion accounted for 76.2%, and the average tumor size was 4.3 cm. Renal biopsy was performed in 11 patients, of which 10 cases showed lung cancer pathologically. Twelve patients received surgical treatment. Patients who underwent surgery were more likely to have no other metastases than those without other metastases (P=0.019). Twenty patients were followed up with an average follow-up time of 34.2 months. Six patients survived and 14 patients died. The median OS was 15.0 months. The median survival time of patients undergoing renal surgery was (15.0±8.1) months, and the average survival time of patients without renal surgery was (15.0±4.1) months. There was no significant difference between two groups.Conclusion The metastatic renal tumor originating from lung cancer is rare, so its diagnosis and treatment is relatively difficult. Surgical treatment of metastatic renal tumor does not improve the prognosis of patients.
-
Key words:
- lung cancer /
- metastatic renal tumor /
- diagnosis /
- treatment
-

-
表 1 肺癌肾脏转移患者临床特征
例(%) 临床特征 总体(n=21) 接受肾脏手术患者(n=12) 未接受肾脏手术患者(n=9) P值 平均年龄/岁 64.3(45~80) 65.3(52~78) 63(45~80) 0.608 性别 0.422 男 17 (81.0) 9(75.0) 8(88.9) 女 4 (19.0) 3(25.0) 1(11.1) 肺癌治疗方式 0.319 手术 15(71.4) 10(83.3) 5(55.6) 放化疗 4(19.0) 1 (8.3) 3(33.3) 其他 2(9.5) 1(8.3) 1(11.1) 肺癌分期 0.899 Ⅰ/Ⅱ 12(57.1) 7(58.3) 5(55.6) Ⅲ/Ⅳ 9(42.9) 5(41.7) 4(44.4) 症状 0.899 有 9 (42.9) 5(41.7) 4(44.4) 无 12(57.1) 7(58.3) 5(55.6) 肾外其他部位转移 0.017 有 10 (47.6) 3(25.0) 7(77.8) 无 11 (52.4) 9(75.0) 2(22.2) 单双侧 0.003 单侧 16(76.2) 12(100) 4(44.4) 双侧 5(23.8) 0 5(55.6) 肾脏转移平均时间/月 21.9(0~123) 29.9(0~123) 11.1(0~35) 0.184 肾脏转移瘤平均直径/cm 4.5(1~8.4) 4.5(2.6~6.1) 4.6(1~8.4) 0.913 肾穿刺活检 0.001 有 11(52.4) 3(25.0) 9(100) 无 10(47.6) 9(75.0) 0 肾手术方式 肾全切 10(47.6) 10(83.3) 肾部分切除 2(9.5) 2(16.7) 表 2 肾脏转移瘤的CT特点
例(%) CT特点 数值 CT特点 数值 肿瘤部位 肿瘤平均直径/cm 4.3(1~8.4) 单侧 16(76.2) 肿瘤边界 双侧 5(23.8) 不清 21(100) 肿瘤数量 清晰 0 单发 16(76.2) 肿瘤外生程度 多发 5(23.8) 内生 17(81.0) 肿瘤侧别 外生 4(19.0) 左侧 6(37.5) 平均CT平扫密度/HU 31.0 右侧 10(62.5) 肾脏转移瘤CT增强-平扫/HU 10.9 肿瘤位置 肺原发灶CT增强-平扫/HU 13.4 上极 7(33.3) 其他部位转移 中极 4(19.0) 有 10(47.6) 下极 10(47.6) 无 11(52.4) 表 3 肺癌肾脏转移总生存时间的单因素与多因素分析
总生存 单因素分析 多因素分析 HR 95%CI P值 HR 95%CI P值 年龄 1.05 0.98~1.12 0.18 1.08 0.99~1.18 0.073 性别 男(参照) 女 0.48 0.11~2.14 0.33 0.27 0.032~2.22 0.22 肺癌分期 Ⅰ/Ⅱ(参照) Ⅲ/Ⅵ 1.78 0.61~5.24 0.29 1.97 0.62~6.31 0.25 肾外其他部位转移 无(参照) 有 0.73 0.25~2.11 0.56 1.12 0.23~5.42 0.89 症状 无(参照) 有 1.01 0.34~3.03 0.98 0.97 0.23~4.02 0.96 肾脏转移时间 ≤12个月(参照) >12个月 0.92 0.32~2.63 0.87 1.86 0.46~7.50 0.38 肾脏手术 有(参照) 无 0.80 0.28~2.35 0.69 1.31 0.24~7.05 0.75 -
[1] Matsumoto C, Imai K, Nakao Y, et al. Renal metastasis from intrahepatic cholangiocarcinoma[J]. Int Cancer Conf J, 2020, 9(2): 66-71. doi: 10.1007/s13691-019-00398-y
[2] Bracken RB, Chica G, Johnson DE, et al. Secondary renal neoplasms: an autopsy study[J]. South Med J, 1979, 72(7): 806-807. doi: 10.1097/00007611-197907000-00013
[3] Zhou C, Urbauer DL, Fellman BM, et al. Metastases to the kidney: a comprehensive analysis of 151 patients from a tertiary referral centre[J]. BJU Int, 2016, 117(5): 775-782. doi: 10.1111/bju.13194
[4] Ettinger DS, Wood DE, Aggarwal C, et al. NCCN Guidelines Insights: Non-Small Cell Lung Cancer, Version 1.2020[J]. J Natl Compr Canc Netw, 2019, 17(12): 1464-1472. doi: 10.6004/jnccn.2019.0059
[5] Khan F, Mahmalji W, Sriprasad S, et al. Prostate cancer with metastases to the kidney: a rare manifestation of a common disease[J]. BMJ Case Rep, 2013, 2013: bcr2012008388.
[6] 肖英明, 陈东, 周芳坚, 等. 肾继发性肿瘤的临床诊治及预后分析[J]. 中华泌尿外科杂志, 2016, 37(5): 331-334. doi: 10.3760/cma.j.issn.1000-6702.2016.05.004
[7] Chen J, Qi N, Zhu S. Metastases to the Kidney: An Analysis of 35 Cases and a Review of Literature[J]. Front Oncol, 2020, 10: 632221.
[8] Anani W, Amin M, Pantanowitz L, et al. A series of collision tumors in the genitourinary tract with a review of the literature[J]. Pathol Res Pract, 2014, 210(4): 217-223. doi: 10.1016/j.prp.2013.12.005
[9] Khurana KK, Powers CN. Basaloid squamous carcinoma metastatic to renal-cell carcinoma: fine-needle aspiration cytology of tumor-to-tumor metastasis[J]. Diagn Cytopathol, 1997, 17(5): 379-382. doi: 10.1002/(SICI)1097-0339(199711)17:5<379::AID-DC12>3.0.CO;2-K
[10] Huo Z, Gao Y, Yu Z, et al. Metastasis of breast cancer to renal cancer: report of a rare case[J]. Int J Clin Exp Pathol, 2015, 8(11): 15417-15421.
[11] Wu PS, Pan CC. Lung adenocarcinoma metastasizing into a renal angiomyolipoma[J]. Int J Surg Pathol, 2015, 23(3): 230-233. doi: 10.1177/1066896915572224
[12] Richardson JF, Katayama I. Neoplasm to neoplasm metastasis. An acidophil adenoma harbouring metastatic carcinoma: a case report[J]. Arch Pathol, 1971, 91(2): 135-139.
[13] Lall C, Houshyar R, Landman J, et al. Renal Collision and Composite Tumors: Imaging and Pathophysiology[J]. Urology, 2015, 86(6): 1159-1164. doi: 10.1016/j.urology.2015.07.032
[14] Huo Z, Gao Y, Yu Z, et al. Metastasis of breast cancer to renal cancer: report of a rare case[J]. Int J Clin Exp Pathol, 2015, 8(11): 15417-15421.
[15] Ichimatsu K, Morii A, Nishio R, et al. Metastatic renal tumor originating from lung cancer: report of two cases[J]. J Urol Surg, 1998, 18(10): 1259-1262.
[16] Honda H, Coffman CE, Berbaum KS, et al. CT analysis of metastatic neoplasms of the kidney. Comparison with primary renal cell carcinoma[J]. Acta Radiol, 1992, 33(1): 39-44. doi: 10.1177/028418519203300108
[17] Lin EC, Alavi A. Urologic Tumors[M]. In: Lin EC, Alavi A, editors. PET and PET/CT: A clinical guide. New York: Thieme, 2009: 204-211.
[18] Aras M, Dede F, Ones T, et al. Is The Value of FDG PET/CT In Evaluating Renal Metastasis Underestimated? A Case Report And Review of The Literature[J]. Mol Imaging Radionucl Ther, 2013, 22(3): 109-112. doi: 10.4274/Mirt.130
[19] Alexander M, Kim SY, Cheng H. Update 2020: Management of Non-Small Cell Lung Cancer[J]. Lung, 2020, 198(6): 897-907. doi: 10.1007/s00408-020-00407-5
[20] Tumati V, Iyengar P. The current state of oligometastatic and oligoprogressive non-small cell lung cancer[J]. J Thorac Dis, 2018, 10(Suppl 21): S2537-S2544.
[21] Fernandez R, Lau R, Ho J, et al. Evidence for surgical resections in oligometastatic lung cancer[J]. J Thorac Dis, 2019, 11(Suppl 7): S969-S975.
[22] Verma V, Simone CB 2nd. Stereotactic body radiation therapy for metastases to the kidney in patients with non-small cell lung cancer: a new treatment paradigm for durable palliation[J]. Ann Palliat Med, 2017, 6(2): 96-103. doi: 10.21037/apm.2017.03.06
-




 下载:
下载: