Efficacy and safety of tamsulosin combined with diclofenac sodium in the treatment of ureteral calculi: a meta-analysis
-
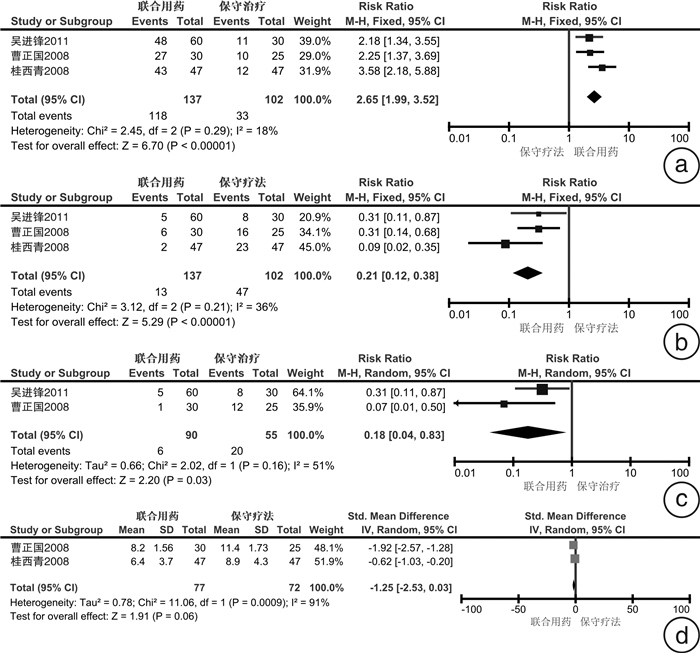
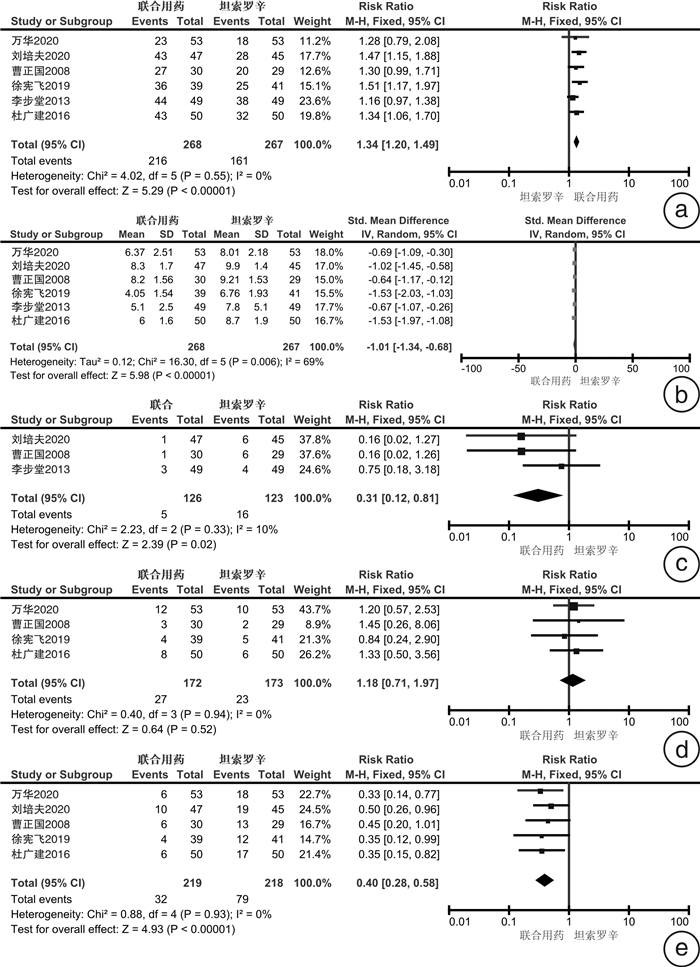
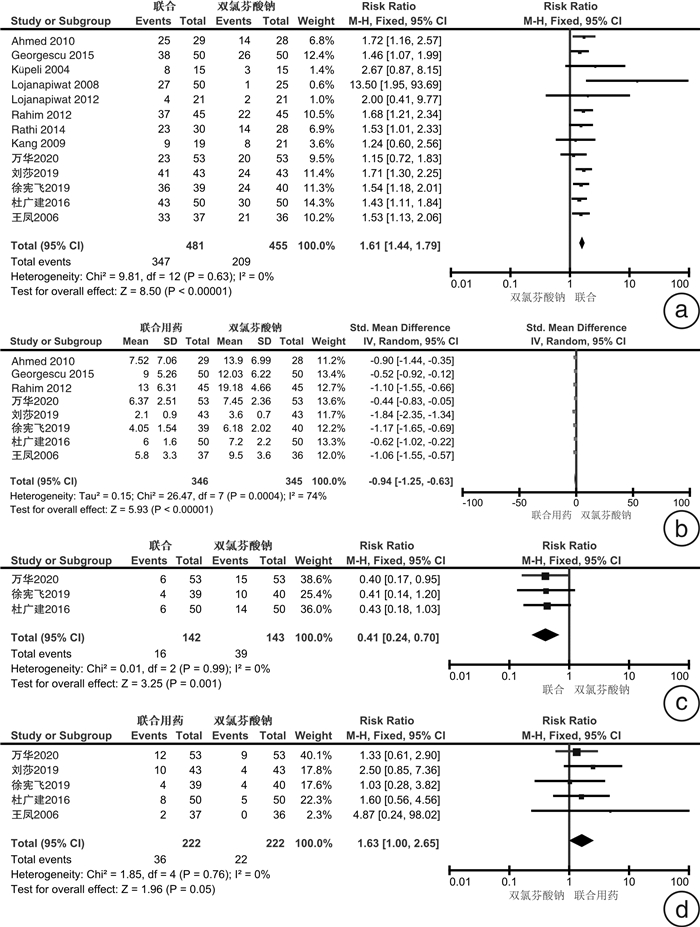
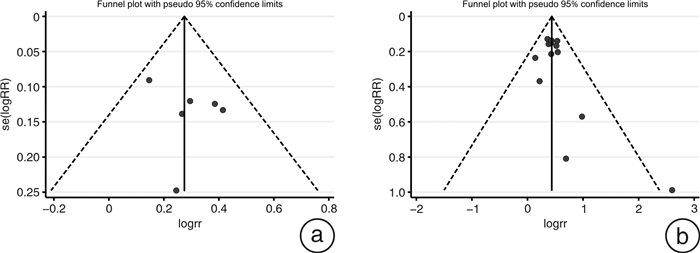
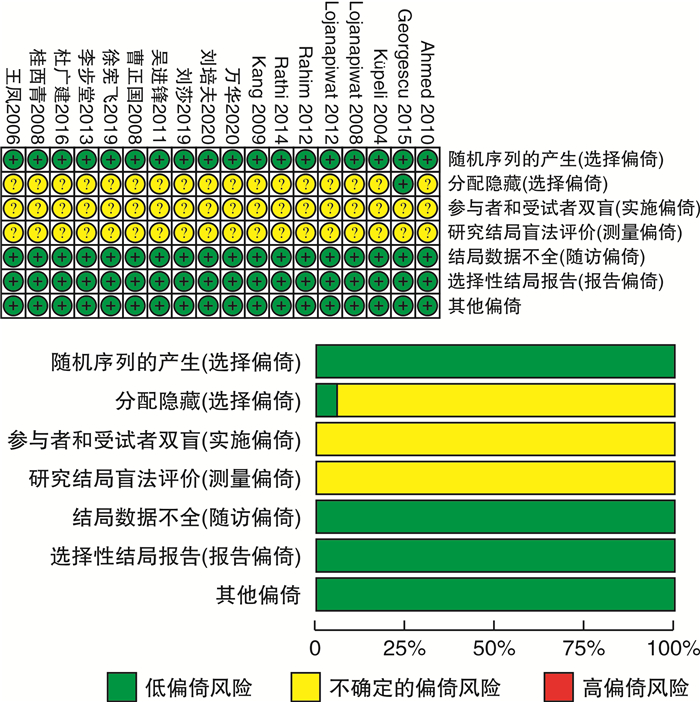
摘要: 目的 系统评价坦索罗辛联合双氯芬酸钠治疗输尿管结石的疗效及安全性。方法 计算机检索PubMed、EMbase、Web of Science、The Cochrane Library、万方、维普及知网数据库,搜集坦索罗辛联合双氯芬酸钠治疗输尿管结石的随机对照试验,检索时限均从建库至2020年9月,采用RevMan 5.3软件进行meta分析。结果 共纳入18个RCT。meta分析结果显示:①联合用药比保守疗法结石排出率更高(RR=2.65,95%CI:1.99~3.52),肾绞痛发生率更低(RR=0.21,95%CI:0.12~0.38)。②联合用药与单用坦索罗辛相比,患者排石率更高(RR=1.34,95%CI:1.20~1.49),排石时间更短(SMD随机=-1.01,95%CI:-1.34~-0.68),肾绞痛发生率更低(RR=0.4,95%CI:0.28~0.58)。③联合用药与单用双氯芬酸钠比较,排石率更高(RR=1.61,95%CI:1.44~1.79),排石时间更短(SMD随机=-0.94,95%CI:-1.25~-0.63),肾绞痛发生率更低(RR=0.41,95%CI:0.24~0.70)。结论 坦索罗辛联合双氯芬酸钠治疗输尿管结石安全有效,有较高排石率,降低了肾绞痛的发生率,但仍需更多大样本,高质量研究予以验证。Abstract: Objective To systematically evaluate the efficacy and safety of tamsulosin combined with diclofenac sodium in the treatment of ureteral calculi.Methods The randomized controlled trials of tamsulosin combined with diclofenac sodium in the treatment of ureteral calculi were retrieved from PubMed, EMbase, Web of Science, The Cochrane Library, Wanfang, VIP and CNKI databases. The retrieval time was from the establishment of the database to September 2020. The meta-analysis was performed using RevMan 5.3 software.Results A total of 18 RCTs were included. The results of meta-analysis showed that: ① Combined therapy had a higher rate of stone removal than conservative therapy[RR=2.65, 95%CI: 1.99-3.52], and a lower incidence of renal colic[RR=0.21, 95%CI: 0.12-0.38]. ② Compared with tamsulosin alone, combined treatment had higher stone discharge rate[RR=1.34, 95%CI: 1.20-1.49], shorter stone discharge time[SMDrandomization=-1.01, 95%CI: -1.34 to-0.68], and lower incidence of renal colic[RR=0.4, 95%CI: 0.28-0.58]. ③ Compared with diclofenac sodium alone, the combined treatment had higher stone discharge rate[RR=1.61, 95%CI: 1.44-1.79], shorter stone discharge time[SMDrandomization=-0.94, 95%CI: -1.25 to-0.63], and lower incidence of renal colic[RR=0.41, 95%CI: 0.24-0.70].Conclusion The combination of tamsulosin and diclofenac sodium is safe and effective in the treatment of ureteral calculi, with a high rate of stone removal and a reduced incidence of renal colic. However, more large samples and high-quality studies are needed for verification.
-
Key words:
- ureteral calculi /
- meta-analysis /
- drug stone removal /
- tamsulosin /
- diclofenac sodium
-

-
表 1 纳入研究的基本特征
纳入研究 结石位置 样本量 随访时间 治疗方案 结石大小/mm 桂西青等,2008[4] 输尿管下段结石 94 2周 试验组(n=47):坦索罗辛(0.2 mg,qd)+双氯芬酸钠栓(50 mg,bid,肛塞)
对照组(n=47):饮水6.7±1.9
7.0±1.8吴进锋,2011[5] 输尿管下段结石 90 2周 试验组1(n=30):坦索罗辛(0.2 mg,qn)+双氯芬酸治疗(50 mg,bid)
试验组2(n=30):坦索罗辛(0.4 mg,qn)+双氯芬酸治疗(50 mg,bid)
对照组(n=30):饮水,运动6.7±2.1
6.8±2.0
6.9±1.8曹正国等,2008[6] 输尿管下段结石 84 3周 试验组(n=30):坦索罗辛(0.2 mg,qn)+双氯芬酸钠(50 mg,bid)
对照组1(n=29):坦索罗辛(0.2mg,qn)
对照组2(n=25):饮水6.4±1.1
6.3±1.0
6.3±1.1李步堂,2013[7] 输尿管中下段 98 - 试验组(n=49):坦索罗辛(0.2 mg,bid)+双氯芬酸钠栓(50 mg,bid,塞肛)
对照组(n=49):坦索罗辛(0.2 mg,bid)5.1±2.5
7.8±5.1万华等,2020[8] 输尿管远端结石 159 - 试验组(n=53):双氯芬酸钠(50 mg,qd,塞肛)+坦索罗辛(0.4 mg,qd)
对照组1(n=53):坦索罗辛(0.4 mg,qd)
对照组2(n=53):双氯芬酸钠(50 mg,qd,塞肛)徐宪飞,2019[9] 输尿管远端结石 120 2周 试验组(n=39):坦索罗辛(0.2 mg/次,qd)+双氯芬酸钠栓(塞肛,50 mg/次,qd)
对照组1(n=41):坦索罗辛(0.2 mg/次,qd)
对照组2(n=40):双氯芬酸钠栓(塞肛50 mg/次,qd)5.16±1.17
5.15±0.98
5.14±1.29杜广建等,2016[10] 输尿管远端结石 150 3周 试验组(n=50):坦索罗辛胶囊(0.2 mg,qd)+双氯芬酸钠栓(50 mg,qd,塞肛)
对照组1(n=50):坦索罗辛胶囊(0.2 mg,qd)
对照组2(n=50):双氯芬酸钠栓(50 mg,qd,塞肛)5.2±1.1
5.1±0.9
5.1±1.0刘培夫,2020[11] 输尿管下段结石 92 2周 试验组(n=47):坦索罗辛(0.2 mg,qd)+双氯芬酸钠(50 mg,qd)
对照组(n=45):坦索罗辛(0.2 mg,qd)6.8±1.3
6.1±0.9刘莎,2019[12] 输尿管下段结石 86 - 试验组(n=43):坦索罗辛(0.2 mg,qd)+双氯芬酸钠栓剂(肛塞,每日50~100 mg)
对照组(n=43):双氯芬酸钠栓剂(肛塞,每日50~100 mg)王凤等,2006[13] 输尿管远段结石 73 2周 试验组(n=37):双氯芬酸(25 mg,tid)+盐酸坦索罗辛(0.4 mg,qd)
对照组(n=36):双氯芬酸(25 mg,tid)6.1±1.5
5.9±1.7Lojanapiwat et al,
2008[14]输尿管远端结石 75 4周 试验组1(n=25):双氯芬酸钠(50 mg,bid,持续10日,后按需肌注)+坦索罗辛(0.2 mg,qd)
试验组2(n=25):双氯芬酸钠(50 mg,bid,持续10 d,后按需肌注)+坦索罗辛(0.4 mg,qd)
对照组(n=25):双氯芬酸钠(50 mg,bid,持续10 d,后按需肌注)6.42 ± 1.48
6.26 ± 1.27
6.70 ± 1.66Ahmed et al,
2010[15]输尿管远端结石 57 30 d 试验组(n=29):坦索罗辛(0.4 mg,qd)+双氯芬酸钠(50 mg,bid,持续1周,后按需肌注)
对照组(n=28):双氯芬酸钠(50 mg,bid,持续1周,后按需肌注)4.97±2.2
5.39±1.81Küpeli et al,
2004[16]输尿管下段结石 30 15 d 试验组(n=15):坦索罗辛(0.4 mg,qd)+双氯芬酸钠(100 mg,qd)
对照组(n=15):双氯芬酸钠(100 mg,qd)4.7(3~5)
4.9(3~5)Rahim et al, 2012[17] 输尿管远端结石 90 4周 试验组(n=45):双氯芬酸钠(50 mg,bid)+坦索罗辛(0.4 mg,qd)
对照组(n=45):双氯芬酸钠(50 mg,bid)6.21±0.70
6.00±0.53Lojanapiwat et al,
2012[18]输尿管近端结石 42 4周 试验组(n=21):双氯芬酸钠(50 mg,bid,持续10 d,后按需肌注)+坦索罗辛(0.4 mg,qd)
对照组(n=21):双氯芬酸钠(50 mg,bid,持续10 d,后按需肌注)Rathi et al,2014[19] 输尿管远端结石 58 4周 试验组(n=30):坦索罗辛(0.4 mg,qd)+双氯芬酸钠(1周,然后按需给予)
对照组(n=28):双氯芬酸钠(1周,然后按需给予)Georgescu et al,
2015[20]输尿管上中下段均有 100 4周 试验组(n=50):坦索罗辛(0.4 mg,qd)+双氯芬酸钠(50 mg,bid,持续1周,后按需给予)
对照组(n=50):双氯芬酸钠(50 mg,bid,持续1周,后按需给予)5.08±2.09
5.1±2.02Kang et al, 2009[21] 输尿管上中下段均有 40 1周 试验组(n=19):双氯芬酸钠(100 mg,qd)+坦索罗辛(0.2 mg,qd)
对照组(n=21):双氯芬酸钠(100 mg,qd)5.1±1.1
4.7±0.8表 2 联合用药组与单用坦索罗辛组排石率比较
组别 纳入研究数 异质性检验结果 效应模型 meta分析结果 P值 I2 RR(95%CI) P值 T:0.2 mg+D:50 mg vs. T: 50 mg 3 0.78 0 固定 1.44(1.24,1.65) <0.00 001 T:0.2 mg+D:100 mg vs. T: 100 mg 1 1.30(0.99,1.71) 0.05 T:0.4 mg+D:100 mg vs. T: 100 mg 1 1.16(0.97,1.38) 0.11 T:0.4 mg+D:50 mg vs. T: 50 mg 1 1.28(0.79,2.08) 0.32 双氯芬酸钠口服 2 0.52 0 固定 1.40(1.17,1.68) 0.000 3 双氯芬酸钠塞肛 4 0.38 2% 固定 1.31(1.15,1.49) <0.000 1 注:T:坦索罗辛,D:双氯芬酸钠 表 3 联合用药组与单用坦索罗辛组排石时间比较
组别 纳入研究数 异质性检验结果 效应模型 meta分析结果 P值 I2 SMD(95%CI) P值 T:0.2 mg+D:50 mg vs. T: 50 mg 3 0.19 40% 固定 -1.34(-1.6,-1.07) <0.000 01 T:0.2 mg+D:100 mg vs. T: 100 mg 1 -0.64(-1.17,-0.12) 0.02 T:0.4 mg+D:100 mg vs. T: 100 mg 1 -0.67(-1.07,-0.26) 0.001 T:0.4 mg+D:50 mg vs. T: 50 mg 1 -0.69(-1.09,-0.30) 0.000 5 双氯芬酸钠口服 2 0.29 12% 固定 -0.86(-1.20,0.53) <0.000 01 双氯芬酸钠塞肛 4 0.002 79% 随机 -1.09(-1.57,-0.61) <0.000 01 表 4 联合用药与单用双氯芬酸钠排石率比较的亚组分析
组别 纳入研究数 异质性检验结果 效应模型 meta分析结果 P值 I2 RR(95%CI) P值 双氯芬酸钠全程使用 8 0.79 0 固定 1.52(1.34,1.72) <0.00001 双氯芬酸钠短程使用 5 0.38 5% 固定 1.70(1.42,2.03) <0.000 01 双氯芬酸钠口服 9 0.68 0 固定 1.66(1.43,1.94) <0.000 01 双氯芬酸钠塞肛 4 0.49 0 固定 1.47(1.26,1.71) <0.000 01 T:0.4 mg+D:100 mg vs. D: 100 mg 6 0.13 42% 固定 1.88(1.54,2.3) <0.000 01 T:0.2 mg+D:100 mg vs. D: 100 mg 2 0.03 79% 随机 2.99(0.31,29.17) 0.35 T:0.2 mg+D:50 mg vs. D: 50 mg 2 0.71 0 固定 1.48(1.23,1.78) <0.000 1 T:0.4 mg+D:50 mg vs. D: 50 mg 1 1.15(0.72,1.83) 0.55 T:0.4 mg+D:75 mg vs. D: 75 mg 1 1.53(1.13,2.06) 0.005 表 5 联合用药与单用双氯芬酸钠排石时间比较
组别 纳入研究数 异质性检验结果 效应模型 meta分析结果 P值 I2 SMD(95%CI) P值 双氯芬酸钠全程使用 6 0.000 4 78% 随机 -1.02(-1.41,-0.63) <0.000 01 双氯芬酸钠短程使用 2 0.28 15% 固定 -0.65(-0.97,-0.33) <0.000 1 双氯芬酸钠口服 4 0.21 34% 固定 -0.86(-1.09,-0.63) <0.000 01 双氯芬酸钠塞肛 4 <0.000 1 86% 随机 -1.00(-1.59,-0.41) 0.000 9 T:0.4 mg+D:100 mg vs. D: 100 mg 3 0.15 47% 固定 -0.81(-1.07,-0.55) <0.000 01 T:0.2 mg+D:50 mg vs. D: 50 mg 2 0.08 67% 随机 -0.88(-1.42,-0.34) 0.001 T:0.4 mg+D:50 mg vs. D: 50 mg 1 -0.44(-0.83,-0.05) 0.03 T:0.4 mg+D:75 mg vs. D: 75 mg 1 -1.06(-1.55,-0.57) <0.000 1 T:坦索罗辛D:双氯芬酸钠 -
[1] 魏汉平, 焦志敏, 刘晓武, 等. 江苏常州885例泌尿系结石成分特点及与患者临床特征的关系[J]. 临床泌尿外科杂志, 2020, 35(10): 791-794, 799. http://lcmw.cbpt.cnki.net/WKC/WebPublication/paperDigest.aspx?paperID=25a3a167-39eb-41df-b191-5641041d7374
[2] Sudah M. Re: Christian Türk, Aleš Petřík, Kemal Sarica, et al. EAU Guidelines on Diagnosis and Conservative Management of Urolithiasis. Eur Urol 2016;69: 468-74: Magnetic Resonance Urography Can be Used to Detect Urinary Stones[J]. Eur Urol, 2016, 69(4): e76-e77. doi: 10.1016/j.eururo.2015.11.009
[3] Kicinski M, Springate DA, Kontopantelis E. Publication bias in meta-analyses from the Cochrane Database of Systematic Reviews[J]. Stat Med, 2015, 34(20): 2781-2793. doi: 10.1002/sim.6525
[4] 桂西青, 郭振宇, 孙华宾, 等. 坦索罗辛联合双氯芬酸钠栓治疗下段输尿管结石的随机对照临床研究[J]. 中国基层医药, 2008, 15(12): 1982-1984. doi: 10.3760/cma.j.issn.1008-6706.2008.12.023
[5] 吴进锋. 坦索罗辛联合双氯芬酸钠对输尿管下段结石的疗效研究[J]. 海峡药学, 2011, 23(10): 89-91. doi: 10.3969/j.issn.1006-3765.2011.10.041
[6] 曹正国, 孙友文, 诸禹平, 等. 坦索罗辛联合双氯芬酸钠在输尿管下段结石辅助排石中的作用[J]. 现代泌尿外科杂志, 2008, 13(6): 435-437. doi: 10.3969/j.issn.1009-8291.2008.06.008
[7] 李步堂. 坦索罗辛联合双氯芬酸钠栓治疗输尿管中下段小结石疗效观察[J]. 中国保健营养, 2013, 23(1): 327-328. https://www.cnki.com.cn/Article/CJFDTOTAL-ZHBJ201301397.htm
[8] 万华, 曾安军, 李金贵. 输尿管远端结石联合应用双氯芬酸钠与坦索罗辛的临床价值[J]. 中国医药指南, 2020, 18(11): 124-125. https://www.cnki.com.cn/Article/CJFDTOTAL-YYXK202011058.htm
[9] 徐宪飞. 双氯芬酸钠栓联合坦索罗辛治疗输尿管远端结石的临床疗效[J]. 现代诊断与治疗, 2019, 30(14): 2402-2403. https://www.cnki.com.cn/Article/CJFDTOTAL-XDZD201914024.htm
[10] 杜广建, 艾克拜尔·阿布拉, 袁留亚, 等. 双氯芬酸钠栓和坦索罗辛及两药联用治疗输尿管远端结石的疗效比较[J]. 药学与临床研究, 2016, 24(2): 151-153. https://www.cnki.com.cn/Article/CJFDTOTAL-YXLY201602015.htm
[11] 刘培夫. 坦索罗辛联合双氯芬酸钠在输尿管下段结石辅助排石中的作用[J]. 北方药学, 2020, 17(6): 99. https://www.cnki.com.cn/Article/CJFDTOTAL-BFYX202006077.htm
[12] 刘莎. 坦索罗辛联合双氯芬酸钠栓剂对泌尿系结石引起肾绞痛缓解处理观察[J]. 世界最新医学信息文摘, 2019, 19(11): 1-2. https://www.cnki.com.cn/Article/CJFDTOTAL-WMIA201911001.htm
[13] 王风, 曹清丽, 张瑜, 等. 盐酸坦索罗辛治疗输尿管远段小结石的临床研究[J]. 中国医师进修杂志, 2006, 29(1): 52-53. doi: 10.3760/cma.j.issn.1673-4904.2006.01.020
[14] Lojanapiwat B, Kochakarn W, Suparatchatpan N, et al. Effectiveness of low-dose and standard-dose tamsulosin in the treatment of distal ureteric stones: a randomized controlled study[J]. J Int Med Res, 2008, 36(3): 529-536. doi: 10.1177/147323000803600318
[15] Ahmed AF, Al-Sayed AY. Tamsulosin versus Alfuzosin in the Treatment of Patients with Distal Ureteral Stones: Prospective, Randomized, Comparative Study[J]. Korean J Urol, 2010, 51(3): 193-197. doi: 10.4111/kju.2010.51.3.193
[16] Küpeli B, Irkilata L, Gürocak S, et al. Does tamsulosin enhance lower ureteral stone clearance with or without shock wave lithotripsy?[J]. Urology, 2004, 64(6): 1111-1115. doi: 10.1016/j.urology.2004.07.020
[17] Rahim J, Mahmood A, Ashraf S, et al. Efficacy of tamsulosin spontaneous expulsion in the treatment of distal ureteric stones[J]. J Comb Theory, 2012, 6(1): 191-194.
[18] Lojanapiwat, B. Role of tamsulosin as medical expulsive therapy for proximal ureteral calculi: A randomized controlled study[J]. Urology, 2012, 80(3): S176.
[19] Rathi S, Agarwal A, Patnaik P, et al. Evaluation of medical expulsive therapy for distal ureteral stone: A prospective randomized controlled study to compare silodosin versus tamsulosin[J]. Ind J Urol, 2014, (30): S83.
[20] Georgescu D, Ioniṭǎradu F, Mulṭescu R, et al. The role of alpha 1-blockers in the medical expulsive therapy for ureteral calculi-a prospective controlled randomized study comparing tamsulosin and silodosint[J]. Farmacia, 2015, 63(2): 184-188.
[21] Kang DI, Cho WY, Kim TH, et al. Effect of Tamsulosin 0.2 mg on the Short-Term Treatment of Urinary Stones: Multicenter, Prospective, Randomized Study[J]. Kore J Urol, 2009, 50(6): 586-590. doi: 10.4111/kju.2009.50.6.586
[22] Ye Z, Zeng G, Chen Z, et al. Reply to Taimur T. Shah, Graeme MacLennan, Rob Pickard, Samuel McClinton and Veeru Kasivisvanathan's Letter to the Editor re: Zhangqun Ye, Guohua Zeng, Huan Yang, et al. Efficacy and Safety of Tamsulosin in Medical Expulsive Therapy for Distal Ureteral Stones with Renal Colic: A Multicenter, Randomized, Double-blind, Placebo-controlled Trial. Eur Urol 2018;73: 385-91[J]. Eur Urol, 2018, 74(2): e45-e47.
[23] Cui Y, Chen J, Zeng F, et al. Tamsulosin as a Medical Expulsive Therapy for Ureteral Stones: A Systematic Review and Meta-Analysis of Randomized Controlled Trials[J]. J Urol, 2019, 201(5): 950-955. doi: 10.1097/JU.0000000000000029
[24] Afshar K, Jafari S, Marks AJ, et al. Nonsteroidal anti-inflammatory drugs(NSAIDs)and non-opioids for acute renal colic[J]. Cochrane Database Syst Rev, 2015, (6): CD006027.
[25] Pathan SA, Mitra B, Cameron PA. A Systematic Review and Meta-analysis Comparing the Efficacy of Nonsteroidal Anti-inflammatory Drugs, Opioids, and Paracetamol in the Treatment of Acute Renal Colic[J]. Eur Urol, 2018, 73(4): 583-595. doi: 10.1016/j.eururo.2017.11.001
[26] Kaynar M, Koyuncu F, Buldu İ, et al. Comparison of the efficacy of diclofenac, acupuncture, and acetaminophen in the treatment of renal colic[J]. Am J Emerg Med, 2015, 33(6): 749-753. doi: 10.1016/j.ajem.2015.02.033
[27] 刘建军, 谷磊. 坦索罗辛在输尿管结石治疗中对急性肾绞痛发生的预防价值[J]. 同济大学学报(医学版), 2016, 37(3): 112-117, 128. https://www.cnki.com.cn/Article/CJFDTOTAL-TJIY201603024.htm
[28] 景婕黎, 魏琴. 双氯芬酸不同剂型联合丁溴东莨菪碱治疗结石性肾绞痛临床疗效比较[J]. 中国药师, 2016, 19(8): 1523-1525. doi: 10.3969/j.issn.1008-049X.2016.08.030
[29] 王跃平, 朱扬进, 陶宏平, 等. 双氯芬酸钠栓联合坦索罗辛治疗肾绞痛疗效分析[J]. 浙江创伤外科, 2016, 21(2): 333-334. doi: 10.3969/j.issn.1009-7147.2016.02.059
[30] Pathan SA, Mitra B, Straney LD, et al. Delivering safe and effective analgesia for management of renal colic in the emergency department: a double-blind, multigroup, randomised controlled trial[J]. Lancet, 2016: 1999-2007.
[31] Bhala N, Emberson J, Merhi A, et al. Vascularand upper gastrointestinal effects of non-steroidal anti-inflammatory drugs: meta-analyses of individual participant data from randomised trials[J]. Lancet, 2013, 382(9894): 769-779. doi: 10.1016/S0140-6736(13)60900-9
-




 下载:
下载: