-
摘要: 目的 探讨125I粒子植入放疗对前列腺癌免疫微环境的影响。方法 利用免疫组织化学技术检测、比较cT1~3N0M0期前列腺癌行125I粒子植入治疗前、后前列腺癌细胞PD-L1表达情况,以及肿瘤微环境中CD3+T、CD4+T、CD8+T、PD-1+T细胞的表达情况变化。结果 前列腺肿瘤细胞PD-L1阳性表达率为55.6%(35/63);肿瘤组织中均可见CD3+、CD4+、CD8+T细胞浸润; 55.6%的组织中可见PD-1+T细胞表达,但数量较少; 经125I粒子植入治疗后行经尿道前列腺切除术的前列腺癌组织中,肿瘤细胞PD-L1表达率明显上调95.8%(22/23),而且表达强度也增加。结论 前列腺癌肿瘤微环境中均可见浸润性T淋巴细胞,但肿瘤抗原特异性T细胞很少; 125I粒子植入放疗可以促进前列腺癌患者的肿瘤免疫反应,但具有一定时间窗; 联合免疫检查点阻断治疗是合理的,或许也很有必要。Abstract: Objective To evaluate the effects of iodine-125 permanent brachytherapy on prostate cancer immune microenvironment.Methods Immunohistological analyses and comparison of the expression of PD-L1 and tumor infiltrating lymphocytes (TILs, CD3+, CD4+, CD8+, PD-1+) on tissue sections between archival prostate biopsy samples and corresponding TURP or RP were performed for≤cT3 prostate cancer patients before receiving brachytherapy.Results PD-L1 were expressed in 55.6% (35/63) cases, and tumor-infiltrating T lymphocytes were seen in all cases. PD-1+T cells were seen in 55.6% cases, but with very small density. After brachytherapy, CD3+, CD4+, CD8+T cells were increased significantly. PD-1+T cells had a moderate raise, and the expression of PD-L1 on PCa cell significantly raised.Conclusion All PCa had TILs expression in cancer immune microenvironment, but may be not tumor antigen-specific T-cell. Iodine-125 permanent brachytherapy can stimulate anti-tumor immunity in a particular time window, and when combined with immunotherapy (Immune Checkpoint Inhibitors), it's reasonable, even necessary.
-

-
[1] Reimers MA, Slane KE, Pachynski RK. Immunotherapy in Metastatic Castration-Resistant Prostate Cancer: Past and Future Strategies for Optimization[J]. Curr Urol Rep, 2019, 20(10): 64. doi: 10.1007/s11934-019-0931-3
[2] Graff JN, Alumkal JJ, Drake CG, et al. Early evidence of anti-PD-1 activity in enzalutamide-resistant prostate cancer[J]. Oncotarget, 2016, 7(33): 52810-52817. doi: 10.18632/oncotarget.10547
[3] Movassaghi M, Chung R, Anderson CB, et al. Overcoming Immune Resistance in Prostate Cancer: Challenges and Advances[J]. Cancers(Basel), 2021, 13(19): 4757.
[4] Ness N, Andersen S, Khanehkenari MR, et al. The prognostic role of immune checkpoint markers programmed cell death protein 1(PD-1) and programmed death ligand 1(PD-L1) in a large, multicenter prostate cancer cohort[J]. Oncotarget, 2017, 8(16): 26789-26801. doi: 10.18632/oncotarget.15817
[5] Nardone V, Botta C, Caraglia M, et al. Tumor infiltrating T lymphocytes expressing FoxP3, CCR7 or PD-1 predict the outcome of prostate cancer patients subjected to salvage radiotherapy after biochemical relapse[J]. Cancer Biol Ther, 2016, 17(11): 1213-1220. doi: 10.1080/15384047.2016.1235666
[6] Hegde PS, Karanikas V, Evers S. The Where, the When, and the How of Immune Monitoring for Cancer Immunotherapies in the Era of Checkpoint Inhibition[J]. Clin Cancer Res, 2016, 22(8): 1865-1874. doi: 10.1158/1078-0432.CCR-15-1507
[7] Hegde PS, Chen DS. Top 10 Challenges in Cancer Immunotherapy[J]. Immunity, 2020, 52(1): 17-35. doi: 10.1016/j.immuni.2019.12.011
[8] Vitkin N, Nersesian S, Siemens DR, et al. The Tumor Immune Contexture of Prostate Cancer[J]. Front Immunol, 2019, 10: 603. doi: 10.3389/fimmu.2019.00603
[9] Nair SS, Weil R, Dovey Z, et al. The Tumor Microenvironment and Immunotherapy in Prostate and Bladder Cancer[J]. Urol Clin North Am, 2020, 47(4S): e17-e54.
[10] Cabel L, Loir E, Gravis G, et al. Long-term complete remission with Ipilimumab in metastatic castrate-resistant prostate cancer: case report of two patients[J]. J Immunother Cancer, 2017, 5: 31. doi: 10.1186/s40425-017-0232-7
[11] Ness N, Andersen S, Valkov A, et al. Infiltration of CD8+ lymphocytes is an independent prognostic factor of biochemical failure-free survival in prostate cancer[J]. Prostate, 2014, 74(14): 1452-1461. doi: 10.1002/pros.22862
[12] Ebelt K, Babaryka G, Figel AM, et al. Dominance of CD4+ lymphocytic infiltrates with disturbed effector cell characteristics in the tumor microenvironment of prostate carcinoma[J]. Prostate, 2008, 68(1): 1-10. doi: 10.1002/pros.20661
[13] Massari F, Ciccarese C, Caliò A, et al. Magnitude of PD-1, PD-L1 and T Lymphocyte Expression on Tissue from Castration-ResistantProstate Adenocarcinoma: An Exploratory Analysis[J]. Target Oncol, 2016, 11(3): 345-351. doi: 10.1007/s11523-015-0396-3
[14] Gevensleben H, Dietrich D, Golletz C, et al. The Immune Checkpoint Regulator PD-L1 Is Highly Expressed in Aggressive Primary Prostate Cancer[J]. Clin Cancer Res, 2016, 22(8): 1969-1977. doi: 10.1158/1078-0432.CCR-15-2042
[15] Han J, Duan J, Bai H, et al. TCR Repertoire Diversity of Peripheral PD-1+ CD8+ T Cells Predicts Clinical Outcomes after Immunotherapy in Patients with Non-Small Cell Lung Cancer[J]. Cancer Immunol Res, 2020, 8(1): 146-154. doi: 10.1158/2326-6066.CIR-19-0398
[16] Gros A, Parkhurst MR, Tran E, et al. Prospective identification of neoantigen-specific lymphocytes in the peripheral blood of melanoma patients[J]. Nat Med, 2016, 22(4): 433-438. doi: 10.1038/nm.4051
[17] Ness N, Andersen S, Khanehkenari MR, et al. The prognostic role of immune checkpoint markers programmed cell death protein 1(PD-1) and programmed death ligand 1(PD-L1) in a large, multicenter prostate cancer cohort[J]. Oncotarget, 2017, 8(16): 26789-26801. doi: 10.18632/oncotarget.15817
[18] Herrera FG, Bourhis J, Coukos G. Radiotherapy combination opportunities leveraging immunity for the next oncology practice[J]. CA Cancer J Clin, 2017, 67(1): 65-85. doi: 10.3322/caac.21358
[19] Finkelstein SE, Salenius S, Mantz CA, et al. Combining immunotherapy and radiation for prostate cancer[J]. Clin Genitourin Cancer, 2015, 13(1): 1-9. doi: 10.1016/j.clgc.2014.09.001
[20] Du E, Wang L, Li CY, et al. Analysis of immune status after iodine-125 permanent brachytherapy in prostate cancer[J]. Onco Targets Ther, 2017, 10: 2561-2567. doi: 10.2147/OTT.S137491
[21] Sudoyo AW, Kurniawan AN, Kusumo GD, et al. Increased CD8 Tumor Infiltrating Lymphocytes in Colorectal Cancer Microenvironment Supports an Adaptive Immune Resistance Mechanism of PD-L1 Expression[J]. Asian Pac J Cancer Prev, 2019, 20(11): 3421-3427. doi: 10.31557/APJCP.2019.20.11.3421
[22] Abiko K, Matsumura N, Hamanishi J, et al. IFN-γ from lymphocytes induces PD-L1 expression and promotes progression of ovarian cancer[J]. Br J Cancer, 2015, 112(9): 1501-1509. doi: 10.1038/bjc.2015.101
[23] Tumeh PC, Harview CL, Yearley JH, et al. PD-1 blockade induces responses by inhibiting adaptive immune resistance[J]. Nature, 2014, 515(7528): 568-871 doi: 10.1038/nature13954
[24] Ishihara D, Pop L, Takeshima T, et al. Rationale and evidence to combine radiation therapy and immunotherapy for cancer treatment[J]. Cancer Immunol Immunother, 2017, 66(3): 281-298. doi: 10.1007/s00262-016-1914-6
[25] Cabel L, Loir E, Gravis G, et al. Long-term complete remission with Ipilimumab in metastatic castrate-resistant prostate cancer: case report of two patients[J]. J Immunother Cancer, 2017, 5: 31. doi: 10.1186/s40425-017-0232-7
[26] Tumeh PC, Harview CL, Yearley JH, et al. PD-1 blockade induces responses by inhibiting adaptive immune resistance[J]. Nature, 2014, 515(7528): 568-571. doi: 10.1038/nature13954
[27] Spitzer MH, Carmi Y, Reticker-Flynn NE, et al. Systemic Immunity Is Required for Effective Cancer Immunotherapy[J]. Cell, 2017, 168(3): 487-502. e15. doi: 10.1016/j.cell.2016.12.022
[28] Arina A, Karrison T, Galka E, et al. Transfer of Allogeneic CD4+ T Cells Rescues CD8+ T Cells in Anti-PD-L1-Resistant Tumors Leading to Tumor Eradication[J]. Cancer Immunol Res, 2017, 5(2): 127-136. doi: 10.1158/2326-6066.CIR-16-0293
[29] Wada S, Harris TJ, Tryggestad E, et al. Combined treatment effects of radiation and immunotherapy: studies in an autochthonous prostate cancer model[J]. Int J Radiat Oncol Biol Phys, 2013, 87(4): 769-776. doi: 10.1016/j.ijrobp.2013.07.015
[30] Nardone V, Botta C, Caraglia M, et al. Tumor infiltrating T lymphocytes expressing FoxP3, CCR7 or PD-1 predict the outcome of prostate cancer patients subjected to salvage radiotherapy after biochemical relapse[J]. Cancer Biol Ther, 2016, 17(11): 1213-1220. doi: 10.1080/15384047.2016.1235666
[31] Mittal D, Gubin MM, Schreiber RD, et al. New insights into cancer immunoediting and its three component phases--elimination, equilibrium and escape[J]. Curr Opin Immunol, 2014, 27: 16-25. doi: 10.1016/j.coi.2014.01.004
[32] Harris TJ, Hipkiss EL, Borzillary S, et al. Radiotherapy augments the immune response to prostate cancer in a time-dependent manner[J]. Prostate, 2008, 68(12): 1319-1329. doi: 10.1002/pros.20794
[33] Hoffmann E, Paulsen F, Schaedle P, et al. Radiotherapy planning parameters correlate with changes in the peripheral immune status of patients undergoing curative radiotherapy for localized prostate cancer[J]. Cancer Immunol Immunother, 2022, 71(3): 541-552. doi: 10.1007/s00262-021-03002-6
[34] Greten FR, Grivennikov SI. Inflammation and Cancer: Triggers, Mechanisms, and Consequences[J]. Immunity, 2019, 51(1): 27-41. doi: 10.1016/j.immuni.2019.06.025
-

| 引用本文: | 王增增, 徐勇. 125I粒子植入放疗对前列腺癌免疫微环境影响的初步分析[J]. 临床泌尿外科杂志, 2022, 37(4): 261-267. doi: 10.13201/j.issn.1001-1420.2022.04.004 |
| Citation: | WANG Zengzeng, XU Yong. Effect of iodine-125 brachytherapy in prostate cancer on immune microenvironment[J]. J Clin Urol, 2022, 37(4): 261-267. doi: 10.13201/j.issn.1001-1420.2022.04.004 |
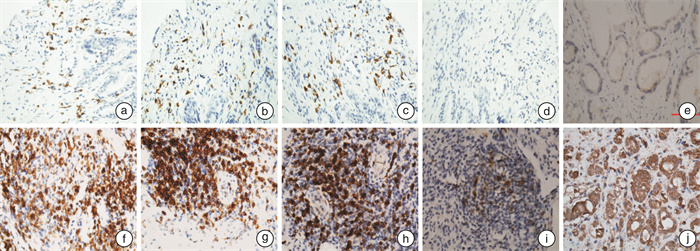
- Figure 1.
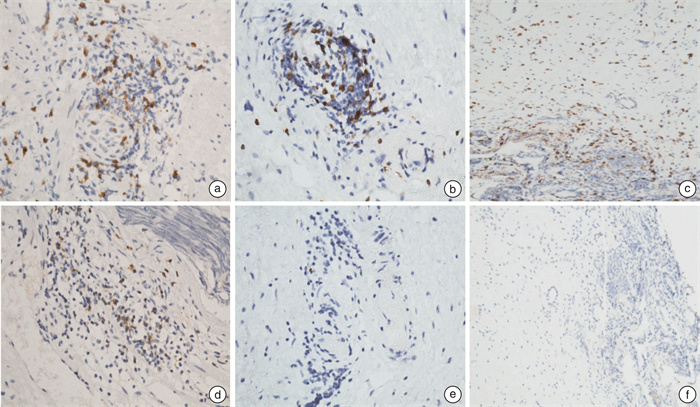
- Figure 2.
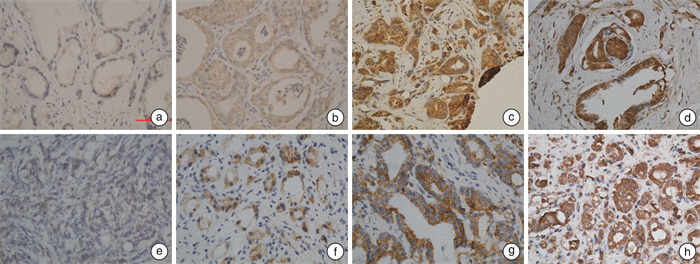
- Figure 3.



 下载:
下载: