Role and consideration of medical imaging in the diagnosis and treatment of renal cell carcinoma
-
摘要: 随着影像学技术的发展和多学科治疗(multi-disciplinary treatment,MDT)模式的推进,肾癌的个体化治疗对影像学精准评估的要求日益增高。传统单纯的影像学定位和定性评判已无法满足现阶段肾癌外科综合治疗的需求,因此需要将影像学的应用场景在肾癌诊疗领域持续拓展。本文总结了医学影像在肾癌诊疗中的应用和研究进展,着重强调了泌尿外科医生最关注的临床痛点和瓶颈问题。从术前临床分期、术中引导治疗、术后随访到肾功能评价等方面,影像学已深度融入到肾癌诊断-治疗-随访的多环节、全过程,发挥指导临床诊疗的作用,但后续仍需突破机器分辨率低、模态单一、主观性干扰等局限,提供全方位、有价值的信息,使患者获益最大化。Abstract: With the development of imaging techniques and the advancement of multi-disciplinary treatment, there is an increasing demand for accurate imaging evaluation in the individualized treatment of renal cell carcinoma. The conventional imaging localization and qualitative diagnosis have been unable to meet the current needs of comprehensive surgical treatment of renal cell carcinoma, so it is necessary to expand the application scene of imaging in the diagnosis and treatment of renal cell carcinoma. This paper summarizes the application and research progress of medical imaging in the diagnosis and treatment of renal cell carcinoma, and emphasizes the difficulties and bottlenecks that are the most concerns among urologists. In terms of preoperative clinical staging, intraoperative guidance, postoperative follow-up, and the evaluation of renal function, imaging has been deeply integrated into the whole process of diagnosis, treatment and follow-up of renal cell carcinoma, and plays an important role in guiding clinical diagnosis and treatment. However, the limitations of low resolution, single mode and subjective interference remain to be resolved to provide omni-directional and valuable information to maximize the benefits of patients.
-
Key words:
- renal cell carcinoma /
- medical imaging /
- diagnosis and treatment
-

-
[1] Türkvatan A, Akdur PO, Altinel M, et al. Preoperative staging of renal cell carcinoma with multidetector CT[J]. Diagn Interv Radiol, 2009, 15(1): 22-30.
[2] Sheth S, Scatarige JC, Horton KM, et al. Current concepts in the diagnosis and management of renal cell carcinoma: role of multidetector ct and three-dimensional CT[J]. Radiographics, 2001, 21 Spec No: S237-S254.
[3] Hamilton ZA, Capitanio U, Pruthi D, et al. Risk Factors for Upstaging, Recurrence, and Mortality in Clinical T1-2 Renal Cell Carcinoma Patients Upstaged to pT3a Disease: An International Analysis Utilizing the 8th Edition of the Tumor-Node-Metastasis Staging Criteria[J]. Urology, 2020, 138: 60-68. doi: 10.1016/j.urology.2019.11.036
[4] Krishna S, Schieda N, Flood TA, et al. Magnetic resonance imaging(MRI)of the renal sinus[J]. Abdom Radiol(NY), 2018, 43(11): 3082-3100. doi: 10.1007/s00261-018-1593-1
[5] Liu BX, Sun W, Kong XQ. Perirenal Fat: A Unique Fat Pad and Potential Target for Cardiovascular Disease[J]. Angiology, 2019, 70(7): 584-593. doi: 10.1177/0003319718799967
[6] Margulis V, Wood CG. Update on staging controversies for locally advanced renal cell carcinoma[J]. Expert Rev Anticancer Ther, 2007, 7(7): 909-914. doi: 10.1586/14737140.7.7.909
[7] Teishima J, Hayashi T, Kitano H, et al. Impact of radiological morphology of clinical T1 renal cell carcinoma on the prediction of upstaging to pathological T3[J]. Jpn J Clin Oncol, 2020, 50(4): 473-478. doi: 10.1093/jjco/hyz154
[8] Damgaci L, Ozer H, Rona G. Diagnostic value of MDCT in determining the perinephric fat tissue and renal sinus invasion in patients with clear cell renal cell carcinoma[J]. Niger J Clin Pract, 2021, 24(4): 489-495.
[9] Lal H, Singh P, Jain M, et al. Role of MRI in staging and surgical planning and its clinicopathological correlation in patients with renal cell carcinoma[J]. Indian J Radiol Imaging, 2019, 29(3): 277-283. doi: 10.4103/ijri.IJRI_177_19
[10] Thompson RH, Leibovich BC, Cheville JC, et al. Is renal sinus fat invasion the same as perinephric fat invasion for pT3a renal cell carcinoma?[J]. J Urol, 2005, 174(4 Pt 1): 1218-1221.
[11] Gill IS, Cacciamani GE, Duddalwar V, et al. Renal cancer with extensive level IV intracardiac tumour thrombus removed by robot[J]. Lancet, 2020, 396(10262): e88. doi: 10.1016/S0140-6736(20)32291-1
[12] Reese AC, Whitson JM, Meng MV. Natural history of untreated renal cell carcinoma with venous tumor thrombus[J]. Urol Oncol, 2013, 31(7): 1305-1309. doi: 10.1016/j.urolonc.2011.12.006
[13] Blute ML, Leibovich BC, Lohse CM, et al. The Mayo Clinic experience with surgical management, complications and outcome for patients with renal cell carcinoma and venous tumour thrombus[J]. BJU Int, 2004, 94(1): 33-41. doi: 10.1111/j.1464-410X.2004.04897.x
[14] Moinzadeh A, Libertino JA. Prognostic significance of tumor thrombus level in patients with renal cell carcinoma and venous tumor thrombus extension. Is all T3b the same?[J]. J Urol, 2004, 171(2 Pt 1): 598-601.
[15] 冯翔, 吕晨, 陈锐, 等. 下腔静脉延迟阻断法在Mayo 2级静脉癌栓取出术中的应用(附光盘)[J]. 现代泌尿外科杂志, 2019, 24(5): 332-335. doi: 10.3969/j.issn.1009-8291.2019.05.002
[16] Liu Z, Li L, Hong P, et al. A Predictive Model for Tumor Invasion of the Inferior Vena Cava Wall Using Multimodal Imaging in Patients with Renal Cell Carcinoma and Inferior Vena Cava Tumor Thrombus[J]. Biomed Res Int, 2020, 2020: 9530618.
[17] 时佳子, 叶华茂, 徐志鹏, 等. 专用超声在机器人辅助腹腔镜肾部分切除术中的应用初探[J]. 临床泌尿外科杂志, 2016, 31(1): 29-30, 34. http://www.cnki.com.cn/Article/CJFDTotal-LCMW201601010.htm
[18] Gill IS, Patil MB, Abreu AL, et al. Zero ischemia anatomical partial nephrectomy: a novel approach[J]. J Urol, 2012, 187(3): 807-814. doi: 10.1016/j.juro.2011.10.146
[19] 范小明, 王力, 张大宏, 等. 腹腔镜超声在中央型肾肿瘤腹腔镜切除术中的应用价值[J]. 中华超声影像学杂志, 2011, 20(9): 772-774. doi: 10.3760/cma.j.issn.1004-4477.2011.09.014
[20] Bates AS, Patel VR. Applications of indocyanine green in robotic urology[J]. J Robot Surg, 2016, 10(4): 357-359. doi: 10.1007/s11701-016-0641-5
[21] 刘承宗, 时佳子, 吴震杰, 等. 术中荧光在机器人辅助腹腔镜下肾部分切除术中的应用初探[J]. 临床泌尿外科杂志, 2018, 33(6): 446-449. http://www.cnki.com.cn/Article/CJFDTotal-LCMW201806007.htm
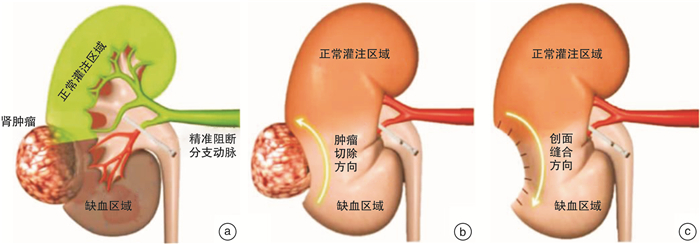
[22] 吴震杰, 王坚超, 刘承宗, 等. 区域血流荧光可视化成像在机器人肾部分切除术中的初步应用体会[J]. 中华泌尿外科杂志, 2017, 38(7): 489-492. doi: 10.3760/cma.j.issn.1000-6702.2017.07.003
[23] 吴震杰, 刘冰, 时佳子, 等. 荧光引导肾动脉分支阻断的机器人腹腔镜肾部分切除术("大家泌尿网"观看手术视频)[J]. 现代泌尿外科杂志, 2021, 26(9): 723-725. doi: 10.3969/j.issn.1009-8291.2021.09.002
[24] Bruno JJ 2nd, Snyder ME, Motzer RJ, et al. Renal cell carcinoma local recurrences: impact of surgical treatment and concomitant metastasis on survival[J]. BJU Int, 2006, 97(5): 933-938. doi: 10.1111/j.1464-410X.2006.06076.x
[25] Wu Q, Huang G, Wei W, et al. Molecular Imaging of Renal Cell Carcinoma in Precision Medicine[J]. Mol Pharm, 2022.
[26] Muselaers CH, Stillebroer AB, Desar IM, et al. Tyrosine kinase inhibitor sorafenib decreases 111In-girentuximab uptake in patients with clear cell renal cell carcinoma[J]. J Nucl Med, 2014, 55(2): 242-247. doi: 10.2967/jnumed.113.131110
[27] Mittlmeier LM, Unterrainer M, Rodler S, et al. 18F-PSMA-1007 PET/CT for response assessment in patients with metastatic renal cell carcinoma undergoing tyrosine kinase or checkpoint inhibitor therapy: preliminary results[J]. Eur J Nucl Med Mol Imaging, 2021, 48(6): 2031-2037. doi: 10.1007/s00259-020-05165-3
[28] Oosting SF, Brouwers AH, van Es SC, et al. 89Zr-bevacizumab PET visualizes heterogeneous tracer accumulation in tumor lesions of renal cell carcinoma patients and differential effects of antiangiogenic treatment[J]. J Nucl Med, 2015, 56(1): 63-69. doi: 10.2967/jnumed.114.144840
[29] Kayani I, Avril N, Bomanji J, et al. Sequential FDG-PET/CT as a biomarker of response to Sunitinib in metastatic clear cell renal cancer[J]. Clin Cancer Res, 2011, 17(18): 6021-6028. doi: 10.1158/1078-0432.CCR-10-3309
[30] Liu G, Jeraj R, Vanderhoek M, et al. Pharmacodynamic study using FLT PET/CT in patients with renal cell cancer and other solid malignancies treated with sunitinib malate[J]. Clin Cancer Res, 2011, 17(24): 7634-7644. doi: 10.1158/1078-0432.CCR-11-1677
-




 下载:
下载: