Precise anatomy combined with "sickle" suture technique in laparoscopic partial nephrectomy for T1b renal hilar tumors
-
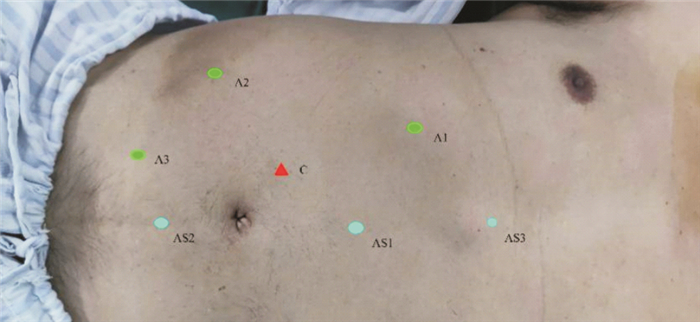
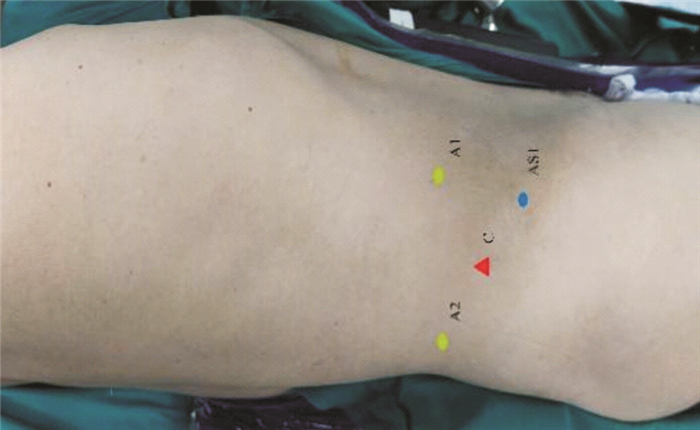
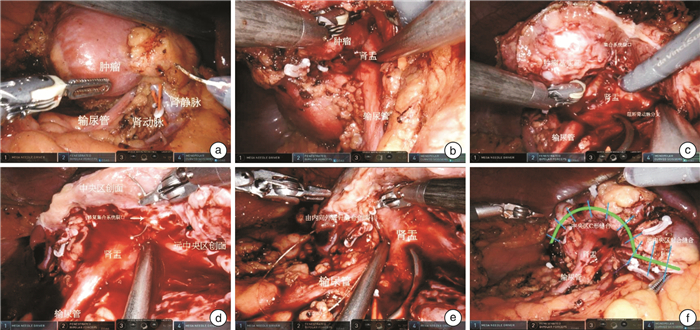
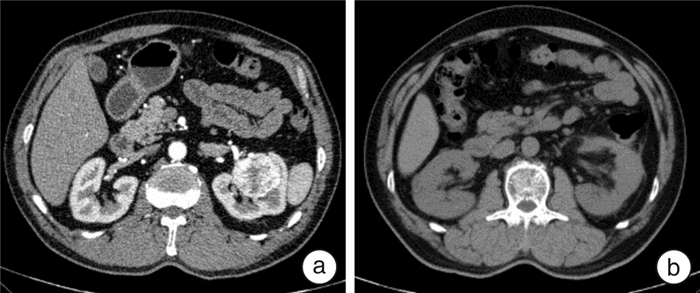
摘要: 目的 分析深度解剖结合“镰形”缝合(PACSS)技术在腹腔镜肾部分切除术治疗T1b期肾门部肿瘤保留肾单位手术中的可行性、有效性和安全性。方法 2018年5月—2022年3月对18例T1b期肾门部肿瘤患者行肾部分切除术,术中应用PACSS技术,其中男16例,女2例。平均年龄(53.35±8.60)岁,平均BMI(25.08±2.35) kg/m2,平均肿瘤最大径为(5.09±0.81) cm,平均R.E.N.A.L.评分为(8.67±0.97)分,平均美国麻醉医师协会(ASA)评分为(1.76±0.56)分。观察记录并分析手术时间、热缺血时间、术中出血量、术后拔管时间、术后住院天数、手术并发症发生率、病理分型、手术切缘阳性发生率、术后随访时间、术后并发症及复发情况、术后1周患肾sGFR下降率及肌酐升高百分比。结果 18例手术均成功,无中转开放,其中1例因术中发现肾静脉瘤栓,1例因术中发现肾窦脂肪侵犯改行根治性肾切除术。平均手术时间(147.41±43.27) min,平均热缺血时间(26.29±8.10) min,平均术中出血量(110.00±101.12) mL,平均术后拔管时间(5.13±2.00) d,平均术后住院时间(7.88±3.76) d。病理回报:18例均为肾透明细胞癌;WHO/ISUPⅠ级1例,Ⅱ级12例,Ⅲ级4例,Ⅳ级1例;术后诊断T1bN0M0 16例,T3aN0M0 2例;无切缘阳性病例。术后平均随访(29.94±17.36)个月,2例因术后轻度血尿延长术后放置引流管时间,无转移、复发、死亡等情况,术后复查肾功能,术后1周患肾sGFR下降率(13.49±3.31)%,肌酐较术前平均升高百分比(21.89±16.32)%。结论 PACSS技术应用于T1b期肾门部肿瘤保留肾单位手术是可行、安全和有效的,值得进一步研究。Abstract: Objective To analyze the feasibility, efficacy and safety of precise anatomy combined with "sickle" suture (PACSS) technique in laparoscopic partial nephrectomy for T1brenal hilar tumors.Methods Eighteen patients with T1b renal hilar tumor underwent nephron sparing surgery using this new technique between May 2018 and March 2022, including 16 males and 2 females, with an average age of (53.35±8.60) years old. Patients' average BMI was (25.08±2.35) kg/m2, and tumor's maximum diameter was (5.09±0.81) cm. The average R.E.N.A.L. score was (8.67±0.97), and ASA score was (1.76±0.56). We observed, recorded and analyzed the operation time, warm ischemia time, estimated blood loss, postoperative tube removal time, postoperative hospital stay, incidence of complications, pathological results, positive rate of surgical margin, postoperative follow-up time, postoperative recurrence and complications, change rate of sGFR and creatinine.Results All 18 cases were successfully operated without conversion to open surgery. Two cases were converted to radical nephrectomy due to the discovery of renal vein tumor thrombus and invasion of renal sinus fat during the operation. The mean operation time was (147.41±43.27) min, and warm ischemia time was (26.29±8.10) min. The mean estimated blood loss was (110.00±101.12) mL, and postoperative tube removal time was (5.13±2.00) d. The mean postoperative hospital stay was (7.88±3.76) d. Pathological findings of all 18 cases were renal clear cell carcinoma, and surgical margins were negative. After follow-up for (29.94±17.36) months, 2 patients had prolonged postoperative drainage tube placement time due to postoperative hematuria. No distant metastasis, local recurrence or death was found. The single-nephron glomerular filtration rate (sGFR) decreased by (13.49±3.31)% and creatinine increased by (21.89±16.32)% one week after operation.Conclusion PACSS technique in laparoscopic partial nephrectomy for T1b renal hilar tumors is feasible, safe and effective. Long follow-up involving more patients is required.
-
Key words:
- precise anatomy /
- sickle suture /
- renal hilar tumor /
- laparoscopic partial nephrectomy
-

-
[1] Lebacle C, Pooli A, Bessede T, et al. Epidemiology, biology and treatment of sarcomatoid RCC: current state of the art[J]. World J Urol, 2019, 37(1): 115-123. doi: 10.1007/s00345-018-2355-y
[2] Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020[J]. CA Cancer J Clin, 2020, 70(1): 7-30. doi: 10.3322/caac.21590
[3] Ljungberg B, Albiges L, Abu-Ghanem Y, et al. European Association of Urology Guidelines on Renal Cell Carcinoma: The 2022 Update[J]. Eur Urol, 2022.
[4] Campbell SC, Clark PE, Chang SS, et al. Renal Mass and Localized Renal Cancer: Evaluation, Management, and Follow-Up: AUA Guideline: Part Ⅰ[J]. J Urol, 2021, 206(2): 199-208. doi: 10.1097/JU.0000000000001911
[5] Gu L, Ma X, Wang B, et al. Laparoscopic vs robot-assisted partial nephrectomy for renal tumours of>4 cm: a propensity score-based analysis[J]. BJU Int, 2018, 122(3): 449-455. doi: 10.1111/bju.14386
[6] Yang C, Wang Z, Huang S, et al. Retroperitoneal Laparoscopic Partial Nephrectomy Versus Radical Nephrectomy for Clinical T1 Renal Hilar Tumor: Comparison of Perioperative Characteristics and Short-Term Functional and Oncologic Outcomes[J]. J Laparoendosc Adv Surg Tech A, 2018, 28(10): 1183-1187. doi: 10.1089/lap.2018.0064
[7] Bertolo R, Autorino R, Simone G, et al. Outcomes of robot-assisted partial nephrectomy for clinical T2 renal tumors: a multicenter analysis(ROSULA collaborative group)[J]. Eur Urol, 2018, 74(2): 226-232. doi: 10.1016/j.eururo.2018.05.004
[8] Yim K, Aron M, Rha KH, et al. Outcomes of robot-assisted partial nephrectomy for clinical T3a renal masses: a multicenter analysis[J]. Eur Urol Focus, 2020, (20): 30295-30299.
[9] Gill IS, Colombo JR Jr, Frank I, et al. Laparoscopic partial nephrectomy for hilar tumors[J]. J Urol, 2005, 174(3): 850-853;discussion 853-854. doi: 10.1097/01.ju.0000169493.05498.c3
[10] 龙嘉辉, 刘霄强, 陈路遥, 等. 肾部分切除术肾组织重建缝合方式的研究进展[J]. 微创泌尿外科杂志, 2021, 10(5): 353-359. https://www.cnki.com.cn/Article/CJFDTOTAL-WCMN202105015.htm
[11] 李南南, 叶云林. 腹腔镜肾部分切除术治疗T1a期肾门肿瘤的临床疗效评价[J]. 国际泌尿系统杂志, 2021, 41(2): 340-342. doi: 10.3760/cma.j.cn431460-20200511-00037
[12] 张战宏, 夏勇, 拓智勇, 等. 两种缝合技术在T1b期肾癌后腹腔镜保留肾单位手术中的效果[J]. 临床医学研究与实践, 2018, 3(25): 11-12, 45. https://www.cnki.com.cn/Article/CJFDTOTAL-YLYS201825005.htm
[13] 刘承宗, 时佳子, 王坚超, 等. 单中心肾门部肿瘤行肾部分切除术经验总结[J]. 临床泌尿外科杂志, 2019, 34(1): 32-35. https://www.cnki.com.cn/Article/CJFDTOTAL-LCMW201901008.htm
[14] Garisto J, Bertolo R, Dagenais J, et al. Robotic versus open partial nephrectomy for highly complex renal masses: Comparison of perioperative, functional, and oncological outcomes[J]. Urol Oncol, 2018, 36(10): 471.e1-471.e9. doi: 10.1016/j.urolonc.2018.06.012
[15] Leibovich BC, Blute M, Cheville JC, et al. Nephron sparing surgery for appropriately selected renal cell carcinoma between 4 and7 cm results in outcome similar to radical nephrectomy[J]. J Urol, 2004, 171(3): 1066-1070. doi: 10.1097/01.ju.0000113274.40885.db
[16] Lee HJ, LissI MA, Derweesh IH. Outcomes of partial nephrectomy for clinical T1b and T2 renal tumors[J]. Curr Opin Urol, 2014, 24(5): 448-452. doi: 10.1097/MOU.0000000000000081
[17] Huang AJ, Cai J, Simmons MN, et al. "Trifecta"in partial nephrectomy[J]. J Urol, 2013, 189(1): 36-42. doi: 10.1016/j.juro.2012.09.042
[18] Rogers CG, Metwalli A, Blatt AM, et al. Robotic partial nephrectomy for renal hilar tumors: A multi-institutional analysis[J]. J Urol, 2008, 180: 2353-2356;discussion 2356. doi: 10.1016/j.juro.2008.08.022
[19] Dulabon LM, Kaouk JH, Haber GP, et al. Multi-institutional analysis of robotic partial nephrectomy for hilar versus nonhilar lesions in 446 consecutive cases[J]. Eur Urol, 2011, 59(3): 325-330. doi: 10.1016/j.eururo.2010.11.017
[20] 王欢, 种铁, 李波涌, 等. 后腹腔镜肾部分切除术治疗T1a期肾门旁肿瘤[J]. 西安交通大学学报(医学版), 2019, 40(3): 451-454, 458. https://www.cnki.com.cn/Article/CJFDTOTAL-XAYX201903022.htm
[21] 管维, 张宗彪, 杨俊, 等. 机器人辅助腹腔镜肾部分切除术处理肾门偏上极骑跨肾血管及肾门前后唇部位肾门肿瘤[J]. 第二军医大学学报, 2020, 41(7): 714-720. https://www.cnki.com.cn/Article/CJFDTOTAL-DEJD202007006.htm
[22] Lattouf JB, Eeri A, D'Ambros OF, et al. Laparoscopic partial nephrectomy for hilar tumors: technique and results[J]. Eur Urol, 2008, 54(2): 409-416. doi: 10.1016/j.eururo.2008.04.007
[23] Eyraud R, Long JA, Snow-Lisy D, et al. Robot-assisted partial nephrectomy for hilar tumors: perioperative outcomes[J]. Urology, 2013, 81(6): 1246-51. doi: 10.1016/j.urology.2012.10.072
[24] Gao Y, Li HZ, Yao YX, et al. Vessel and Tension-Free Reconstruction During Robot-Assisted Partial Nephrectomy for Hilar Tumors: "Garland"Technique and Midterm Outcomes[J]. J Endourol, 2020, 34(4): 469-474. doi: 10.1089/end.2019.0792
[25] 周建, 聂黎虹, 田国林, 等. R. E. N. A. L. 肾肿瘤评分联合MAP肾周脂肪评分用于肾部分切除手术的临床意义[J]. 临床泌尿外科杂志, 2021, 36(9): 699-703. https://www.cnki.com.cn/Article/CJFDTOTAL-LCMW202109005.htm
[26] 李霖, 潘秀武, 崔心刚. 肾门肿瘤的腹腔镜手术难点和技巧改进[J]. 临床外科杂志, 2021, 29(2): 195-198. https://www.cnki.com.cn/Article/CJFDTOTAL-LCWK202102035.htm
[27] Klatte T, Ficarra V, Gratzke C, et al. A literature review of renal surgical anatomy and surgical strategies for partial nephrectomy[J]. Eur Urol, 2015, 68: 980-992.
[28] Knag HW, Lee SK, Kim WT, et al. Surgical margin does not influence recurrence rate in pT1 clear cell renal cell carcinoma after partial nephrectomy: A multicenter study[J]. J Surg Oncol, 2016, 114(1): 70-74.
[29] 富智斌, 董凯, 顾迪, 等. 机器人辅助腹腔镜肾动脉无阻断肾部分切除术与分支阻断肾部分切除术治疗cT1期肾癌的疗效比较[J]. 临床泌尿外科杂志, 2021, 36(3): 173-177. https://www.cnki.com.cn/Article/CJFDTOTAL-LCMW202103002.htm
-




 下载:
下载: