The value of 24 h urine metabolic assessment combined with renal function in the diagnosis of upper urinary tract uric acid stones
-
摘要: 目的探讨24 h尿液代谢评估联合肾功能指标在上尿路尿酸结石诊断中的价值。方法回顾性分析2019年2月—2022年1月我院495例上尿路结石患者的临床资料,根据术后结石成分分析结果分为尿酸结石组(43例)与非尿酸结石组(452例),比较两组间的临床指标差异。应用ROC曲线确定不同指标的最佳截断值并进行分组,通过单因素及多因素logistic回归分析上尿路尿酸结石形成的独立危险因素。结果尿酸结石组与非尿酸结石组年龄、血尿素、肌酐、尿酸、尿pH、24 h尿枸橼酸、24 h尿钙以及BMI≥25 kg/m2、高血压、高血糖、高血脂比例均差异有统计学意义(均P < 0.05)。logistic回归分析结果显示,年龄≥49.5岁(OR=2.767,95%CI:1.026~7.463)、高血糖(OR=3.362,95%CI:1.216~8.750)、血肌酐≥92.4 μmol/L(OR=3.462,95%CI:1.366~8.776)、血尿酸≥443.6 μmol/L(OR=2.564,95%CI:1.093~6.018)、尿pH≤5.7(OR=7.586,95%CI:3.158~18.226)、尿钙≤3.15 mmol/24 h(OR=3.753,95%CI:1.439~9.787)是上尿路尿酸结石的独立危险因素。结论年龄、高血糖、血肌酐、血尿酸、尿pH及24 h尿钙是上尿路尿酸结石形成的危险因素,可作为上尿路尿酸结石诊疗的临床依据。Abstract: ObjectiveTo explore the value of 24 h urine metabolic assessment combined with renal function indexes in the diagnosis of uric acid stones in the upper urinary tract.MethodsThe clinical data of 495 patients with upper urinary tract stones in our hospital from February 2019 to January 2022 were retrospectively analyzed. According to the results of stone composition analysis after surgery, they were divided into uric acid stone group(n=43) and non uric acid stone group(n=452), the differences of clinical indexes between the two groups were compared. Receiver operating characteristic(ROC) curve was performed on these indexes to obtain the cut-off value and the patients were grouped according to it. The independent risk factors of upper urinary tract uric acid stone were analyzed by univariate and multivariate logistic regression.ResultsThe differences in age, blood urea, serum creatinine, blood uric acid, urine pH, 24 h urinary citrate, 24 h urinary calcium, BMI≥25 kg/m2, hypertension, hyperglycemia and hyperlipidemia between the two groups were statistically significant(all P < 0.05). Logistic regression analysis showed that age≥49.5 years old(OR=2.767, 95%CI: 1.026-7.463), hyperglycemia(OR=3.362, 95%CI: 1.216-8.750), serum creatinine≥92.4 μmol/L(OR=3.462, 95%CI: 1.366-8.776), blood uric acid≥443.6 μmol/L(OR=2.564, 95%CI: 1.093-6.018), urine pH≤5.7(OR=7.586, 95%CI: 3.158-18.226), and urinary calcium≤3.15 mmol/24 h(OR=3.753, 95%CI: 1.439-9.787) were independent risk factors of upper urinary tract uric acid stones.ConclusionAge, hyperglycemia, serum creatinine, blood uric acid, urinary pH, and 24 h urinary calcium are risk factors for the formation of upper urinary tract uric acid stones, and they can be used as clinical basis for the diagnosis and treatment of it.
-

-
表 1 尿酸结石组与非尿酸结石组临床资料比较
例(%),X±S 项目 尿酸结石组(43例) 非尿酸结石组(452例) Z/χ2值 P值 年龄/岁 58.30±12.79 48.31±12.56 -4.340 < 0.01 性别 1.326 0.25 男 31(72.1) 286(63.3) 女 12(27.9) 166(36.7) BMI≥25 kg/m2 26(60.5) 195(43.1) 4.768 0.03 高血压 31(72.1) 245(54.2) 5.094 0.02 高血糖 18(41.9) 52(11.5) 29.80 < 0.01 高血脂 30(69.8) 231(51.1) 5.486 0.02 血尿素/(mmol·L-1) 9.00±4.00 5.61±1.96 -6.325 < 0.01 血肌酐/(μmol·L-1) 129.41±85.17 77.42±41.60 -6.195 < 0.01 血尿酸/(μmol·L-1) 470.09±129.82 372.61±97.03 -4.873 < 0.01 尿pH 5.51±0.44 6.15±0.56 -6.961 < 0.01 尿尿酸/[μmol·(24 h)-1] 3171.47±1005.01 3237.77±1113.62 -0.106 0.92 尿草酸/[mmol·(24 h)-1] 0.43±0.27 0.42±0.26 -0.131 0.90 尿枸橼酸/[mmol·(24 h)-1] 0.66±0.63 0.98±0.74 -3.371 < 0.01 尿磷酸/[mmol·(24 h)-1] 16.26±7.26 16.51±7.00 -0.052 0.96 尿氯/[mmol·(24 h)-1] 168.74±65.91 182.71±88.17 -0.687 0.49 尿钾/[mmol·(24 h)-1] 25.98±8.18 28.92±11.42 -1.601 0.11 尿钠/[mmol·(24 h)-1] 172.06±68.61 185.04±89.69 -0.590 0.56 尿钙/[mmol·(24 h)-1] 2.41±1.51 4.62±2.25 -6.792 < 0.01 尿镁/[mmol·(24 h)-1] 3.24±1.35 3.14±1.68 -0.77 0.44 表 2 不同指标诊断上尿路尿酸结石的ROC曲线分析
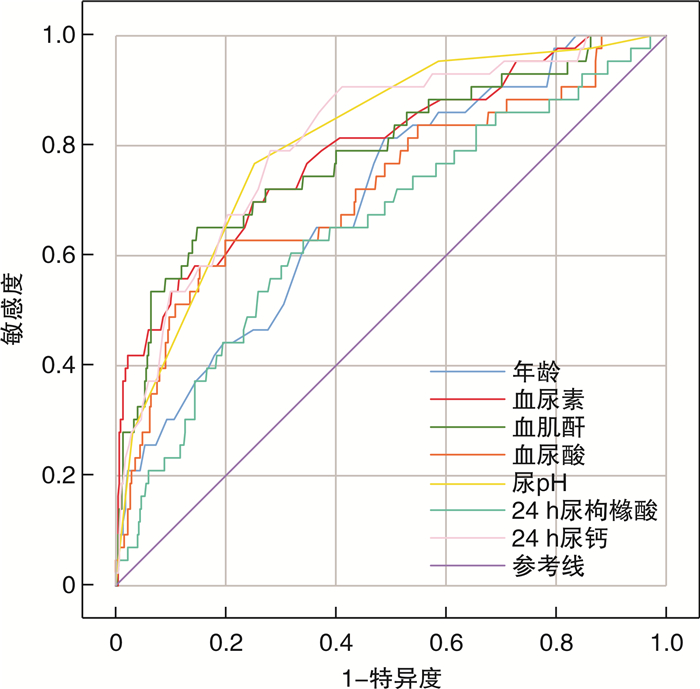
项目 AUC 标准误 P值 95%CI 截断值 敏感度 特异度 年龄 0.700 0.040 < 0.01 0.621~0.779 49.50 0.814 0.511 血尿素 0.792 0.039 < 0.01 0.714~0.869 6.35 0.698 0.750 血肌酐 0.786 0.041 < 0.01 0.706~0.866 92.40 0.651 0.852 血尿酸 0.725 0.045 < 0.01 0.636~0.814 443.60 0.628 0.801 pH 0.810 0.033 < 0.01 0.745~0.875 5.74 0.767 0.748 24 h尿枸橼酸 0.655 0.046 < 0.01 0.566~0.745 0.52 0.628 0.659 24 h尿钙 0.813 0.034 < 0.01 0.746~0.880 3.15 0.791 0.719 表 3 尿酸结石组与非尿酸结石组单因素logistic回归分析
项目 B值 OR(95%CI) P值 年龄≥49.5岁 1.520 4.573(2.076~10.075) < 0.01 BMI≥25 kg/m2 0.701 2.016(1.064~3.819) 0.03 高血压 0.781 2.183(1.093~4.358) 0.03 高血糖 1.712 5.538(2.831~10.837) < 0.01 高血脂 0.792 2.208(1.123~4.342) 0.02 血尿素≥6.35 mmol/L 1.935 6.923(3.491~13.730) < 0.01 血肌酐≥92.4 μmol/L 2.373 10.726(5.441~21.145) < 0.01 血尿酸≥443.6 μmol/L 1.915 6.787(3.508~13.133) < 0.01 尿pH≤5.7 2.281 9.784(4.674~20.480) < 0.01 尿枸橼酸≤0.52 mmol/24 h 1.095 2.989(1.573~5.677) < 0.01 尿钙≤3.15 mmol/24 h 2.269 9.668(4.508~20.730) < 0.01 表 4 尿酸结石组与非尿酸结石组多因素logistic回归分析
项目 B值 OR(95%CI) P值 年龄≥49.5岁 1.018 2.767(1.026~7.463) 0.04 BMI≥25 kg/m2 0.400 1.492(0.625~3.562) 0.37 高血压 -0.002 0.998(0.408~2.443) 0.99 高血糖 1.182 3.262(1.216~8.750) 0.02 高血脂 0.255 1.291(0.524~3.178) 0.58 血尿素≥6.35 mmol/L 0.182 1.200(0.452~3.185) 0.72 血肌酐≥92.4 μmol/L 1.242 3.462(1.366~8.776) < 0.01 血尿酸≥443.6 μmol/L 0.942 2.564(1.093~6.018) 0.03 尿pH≤5.7 2.026 7.586(3.158~18.226) < 0.01 尿枸橼酸≤0.52 mmol/24 h 0.539 1.714(0.682~4.309) 0.25 尿钙≤3.15 mmol/24 h 1.323 3.753(1.439~9.787) < 0.01 -
[1] Sorokin I, Mamoulakis C, Miyazawa K, et al. Epidemiology of stone disease across the world[J]. World J Urol, 2017, 35(9): 1301-1320. doi: 10.1007/s00345-017-2008-6
[2] 邓华, 杨义, 陆丽兰, 等. 结石类型与血脂代谢的相关性研究[J]. 临床泌尿外科杂志, 2020, 35(4): 287-290, 296. doi: 10.13201/j.issn.1001-1420.2020.04.007
[3] Boyd C, Wood K, Whitaker D, et al. The influence of metabolic syndrome and its components on the development of nephrolithiasis[J]. Asian J Urol, 2018, 5(4): 215-222. doi: 10.1016/j.ajur.2018.06.002
[4] Chang CW, Ke HL, Lee JI, et al. Metabolic syndrome increases the risk of kidney stone disease: a cross-sectional and longitudinal cohort study[J]. J Pers Med, 2021, 11(11): 1154-1162. doi: 10.3390/jpm11111154
[5] 张勇, 陈站, 陈建刚, 等. 尿酸结石致病相关基因的研究进展[J]. 临床泌尿外科杂志, 2021, 36(2): 148-151. https://www.cnki.com.cn/Article/CJFDTOTAL-LCMW202102016.htm
[6] Ma Q, Fang L, Su R, et al. Uric acid stones, clinical manifestations and therapeutic considerations[J]. Postgrad Med J, 2018, 94(1114): 458-462. doi: 10.1136/postgradmedj-2017-135332
[7] Heilberg IP. Treatment of patients with uric acid stones[J]. Urolithiasis, 2016, 44(1): 57-63. doi: 10.1007/s00240-015-0843-8
[8] Lombardo F, Bonatti M, Zambozl GA, et al. Uric acid versus non-uric acid renal stones: in vivo differentiation with spectral CT[J]. Clin Radiol, 2017, 72(6): 490-496. doi: 10.1016/j.crad.2017.01.018
[9] Stewart G, Johnson L, Ganesh H, et al. Stone size limits the use of Hounsfield units for prediction of calcium oxalate stone composition[J]. Urology, 2015, 85(2): 292-295. doi: 10.1016/j.urology.2014.10.006
[10] Nourian A, Ghiraldi E, Friedlander JI. Dual-energy CT for urinary stone evaluation[J]. Curr Urol Rep, 2020, 22(1): 1.
[11] Damor M, Songra MC, Patbamniya NK. Study of urine Ph, hypercalciuria, urinary tract infection and its correlation with stone composition in bhopal region[J]. J Evolution Med Dent Sci, 2015, 4(88): 15298-15304. doi: 10.14260/jemds/2015/2175
[12] Wiederkehr MR, Moe OW. Uric acid nephrolithiasis: a systemic metabolic disorder[J]. Clin Rev Bone Miner Metab, 2011, 9(3-4): 207-217. doi: 10.1007/s12018-011-9106-6
[13] Torricelli FC, Brown R, Berto FC, et al. Nomogram to predict uric acid kidney stones based on patient's age, BMI and 24-hour urine profiles: A multicentre validation[J]. Can Urol Assoc J, 2015, 9(3-4): 178-182. doi: 10.5489/cuaj.2682
[14] Tilahun A, Beyene P. Kidney stone disease: an update on current concepts[J]. Adv Urol, 2018, 2(4): 1-12.
[15] Chou YH, Li CC, Hsu H, et al. Renal function in patients with urinary stones of varying compositions[J]. Kaohsiung J Med Sci, 2011, 27(7): 264-267. doi: 10.1016/j.kjms.2010.11.008
[16] Li CC, Chien TM, Wu WJ, et al. Uric acid stones increase the risk of chronic kidney disease[J]. Urolithiasis, 2018, 46(6): 543-547. doi: 10.1007/s00240-018-1050-1
[17] Ling H, Chen H, Wei M, et al. The Effect of autophagy on inflammation cytokines in renal ischemia/reperfusion injury[J]. Inflammation, 2016, 39(1): 347-356. doi: 10.1007/s10753-015-0255-5
[18] Katz JE, Soodana-Prakash N, Jain A, et al. Influence of age and geography on chemical composition of 98043 urinary stones from the USA[J]. Eur Urol Open Sci, 2021, 34: 19-26. doi: 10.1016/j.euros.2021.09.011
[19] 魏汉平, 焦志敏, 刘晓武, 等. 江苏常州885例泌尿系结石成分特点及与患者临床特征的关系[J]. 临床泌尿外科杂志, 2020, 35(10): 791-794, 799. https://www.cnki.com.cn/Article/CJFDTOTAL-LCMW202010007.htm
[20] Menezes CJ, Worcester EM, Coe FL, et al. Mechanisms for falling urine pH with age in stone formers[J]. Am J Physiol Renal Physiol, 2019, 317(7): F65-F72.
[21] Hess B. Metabolic syndrome, obesity and kidney stones[J]. Arab J Urol, 2012, 10(3): 258-264.
[22] Abate N, Chandalia M, Cabo-Chan AV, et al. The metabolic syndrome and uric acid nephrolithiasis: novel features of renal manifestation of insulin resistance[J]. Kidney Int, 2004, 65(2): 386-392.
[23] Hashimoto Y, Hamaguchi M, Nakanishi N, et al. Urinary pH is a predictor of diabetes in men; a population based large scale cohort study[J]. Diabetes Res Clin Pract, 2017, 130: 9-14.
[24] Hartman C, Friedlander JI, Moreira DM, et al. Does hypertension impact 24-hour urine parameters in patients with nephrolithiasis?[J]. Urology, 2015, 85(3): 539-543.
[25] Almannie RM, Al-Nasser KA, Al-Barraq KM, et al. The effect of the body mass index on the types of urinary tract stones[J]. Urol Ann, 2020, 12(1): 42-48.
-




 下载:
下载: