Prognostic value of combined fibrinogen concentration and neutrophil-to-lymphocyte ratio in prostate cancer
-
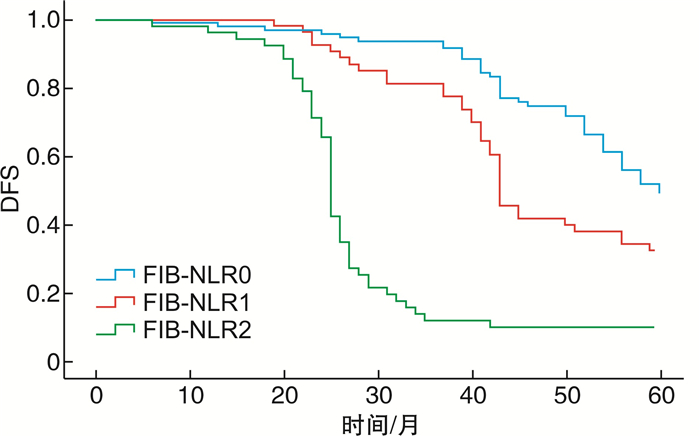
摘要: 目的 探讨术前纤维蛋白原(FIB)联合中性粒细胞与淋巴细胞比值(NLR)形成的FIB-NLR评分系统对前列腺癌(PCa)的预后价值。方法 回顾性分析新疆生产建设兵团医院泌尿外科2012年1月1日—2022年1月1日收治的210例经前列腺穿刺活检及前列腺根治性切除术后病理首次确诊为PCa患者的临床病例资料。用受试者工作特征曲线(ROC)确定NLR与FIB区分组织分级的最佳截断值分别为2.24 g/L和3.88 g/L,并对FIB-NLR评分值进行分组,分别计为FIB-NLR 0、1、2分。用χ2检验分析FIB-NLR评分与PCa患者的临床病理特征间的关系。通过Kapian-Meier法进行生存分析,建立单因素及多因素Cox比例风险模型,探讨影响PCa预后的危险因素和独立危险因子。结果 根据ROC曲线最佳截点分组为FIB-NLR 0分组:FIB≤3.88 g/L且NLR≤2.24;FIB-NLR 1分组:FIB>3.88 g/L或NLR>2.24;FIB-NLR 2分组:FIB>3.88 g/L且NLR>2.24。FIB-NLR 0分95例(47.5%)、FIB-NLR 1分53例(26.5%)、FIB-NLR 2分52例(26.0%);FIB-NLR 0、1、2分患者的5年生存期分别为91.88%、87.15%、59.72%,5年无疾病进展生存期分别为87.83%、77.18%、43.95%,差异均有统计学意义(P < 0.001)。PCa患者术前不同FIB-NLR评分肿瘤病理分期、Gleason评分、危险程度分级、术前tPSA差异有统计学意义(P < 0.05)。单因素分析结果表示FIB-NLR评分、FIB浓度、NLR值、肿瘤病理分期、Gleason评分、术前tPSA浓度是影响PCa患者总生存期与无病生存期的危险因素;多因素分析结果表明FIB-NLR评分是PCa患者的独立预后因子。结论 FIB-NLR评分对预测PCa患者预后有一定的价值。
-
关键词:
- 前列腺癌 /
- 纤维蛋白原 /
- 中性粒细胞与淋巴细胞比值 /
- FIB-NLR评分 /
- 预后
Abstract: Objective To investigate the prognostic value of fibrinogen (FIB)-neutrophil-to-lymphocyte ratio (NLR) scoring system formed by FIB level combined with NLR in prostate cancer (PCa).Methods We retrospectively analyzed the clinical data of 210 patients with PCa diagnosed by prostate biopsy and postoperative pathology in the Department of Urology, Xinjiang Production and Construction Corps Hospital from January 1st, 2012 to January 1st, 2022. Receiver operating characteristic (ROC) curve was used to determine the optimal cut-off values of NLR and FIB to differentiate tissue grading, and optimal cut-off values were 2.24 and 3.88 g/L, respectively. FIB-NLR scores were divided into three groups, which were 0, 1 and 2 FIB-NLR scores. Chi-square test was used to analyze the relationship between FIB-NLR score and clinical pathological features of patients with PCa. Kaplan-Meier method was used for survival analysis, and log rank method was used for difference type test. Univariate and multivariate Cox proportional hazard models were established to explore the risk factors and independent risk factors affecting the prognosis of PCa.Results According to the results of ROC curve, FIB-NLR 0 score group inclouded FIB ≤3.88 g/L and NLR ≤ 2.24; FIB-NLR 1 group: FIB >3.88 g/L or NLR >2.24; FIB-NLR 2 group: FIB >3.88 g/L and NLR >2.24. There were 95 cases (47.5%) with FIB-NLR 0, 53 cases (26.5%) with FIB-NLR 1 and 52 cases (26.0%) with FIB-NLR 2. The 5-year survival time of patients with FIB-NLR 0, 1, 2 points were 91.88%, 87.15%, 59.72%, respectively, and the 5-year progression free survival time were 87.83%, 77.18%, 43.95%, respectively (P < 0.001). There were significant differences in tumor pathological stage, Gleason score, risk grade and TPSA (P < 0.05) among different FIB-NLR score groups. Univariate analysis showed that FIB-NLR score, FIB concentration, NLR value, tumor pathological stage, Gleason score and preoperative TPSA concentration were risk factors for overall survival (OS) and disease-free survival (DFS) of PCa patients (P < 0.05). Multivariate analysis showed that FIB-NLR score was an independent prognostic factor.Conclusion Preoperative FIB-NLR score can be used as a useful index to predict the prognosis of patients with PCa.-
Key words:
- prostate cancer /
- fibrinogen /
- neutrophil lymphocyte ratio /
- FIB-NLR score /
- prognosis
-

-
表 1 FIB-NLR与PCa患者临床病理特征和临床资料之间的相关性
例(%) 项目 FIB-NLR评分 χ2 P 0分 1分 2分 年龄 1.39 0.531 < 65岁 25(26.3) 11(20.8) 9(17.3) ≥65岁 70(73.7) 42(79.2) 43(83.7) BMI 4.58 0.118 < 24 kg/m2 52(54.7) 36(67.9) 26(50.0) ≥24 kg/m2 43(45.3) 17(32.1) 26(50.0) 前列腺体积 6.71 0.152 < 30 mL 29(30.5) 13(24.5) 9(17.3) 30~50 mL 40(42.1) 34(58.5) 31(59.6) >50 mL 26(27.4) 9(17.0) 12(23.1) 高血压史 1.129 0.569 有 50(52.7) 30(56.6) 29(55.8) 无 45(47.3) 23(43.4) 23(44.2) 糖尿病史 0.369 0.831 有 52(54.7) 33(62.3) 27(51.9) 无 43(45.3) 20(37.7) 25(48.1) 吸烟史 0.112 0.946 有 50(52.6) 19(35.9) 23(44.2) 无 45(47.4) 34(64.1) 29(55.8) 术前tPSA 27.986 < 0.001 < 10 ng/mL 54(56.8) 17(32.1) 11(21.2) 10~20 ng/mL 33(34.7) 26(49.1) 22(42.3) >20 ng/mL 8(8.4) 10(18.9) 19(36.5) Gleason评分 26.624 < 0.001 < 7分 14(14.7) 4(7.5) 0(0) 7分 74(77.9) 36(67.9) 32(61.5) >7分 7(7.4) 13(24.5) 20(38.5) 病理分期 50.416 < 0.001 ≤T2c(Ⅰ、Ⅱ) 85(89.5) 35(66.0) 17(32.7) >T2c(Ⅲ、Ⅳ) 10(10.5) 18(34.0) 35(67.3) 危险程度分级 38.858 < 0.001 低 43(45.3) 22(41.5) 6(11.5) 中 44(46.3) 21(39.6) 20(38.5) 高 8(8.4) 10(18.9) 26(50.0) 辅助治疗 50.416 < 0.001 否 85(89.5) 35(66.0) 17(32.7) 是 10(10.5) 18(34.0) 35(67.3) 表 2 影响PCa患者预后的单因素Cox回归分析
变量 DFS OS P HR 95%CI P HR 95%CI 年龄 0.143 1.385 0.885~2.145 0.173 1.362 0.873~2.144 BMI 0.883 1.025 0.726~1.47 0.843 1.036 0.735~1.464 前列腺体积 0.485 0.918 0.725~1.167 0.505 0.923 0.729~1.168 高血压史 0.085 1.373 0.955~1.974 0.083 1.375 0.957~1.984 糖尿病史 0.408 1.201 0.777~1.855 0.462 1.176 0.762~1.83 吸烟史 0.435 0.834 0.527~1.317 0.424 0.833 0.525~1.312 术前tPSA < 0.001 1.778 1.417~2.227 < 0.001 1.728 1.382~2.167 Gleason评分 0.001 1.703 1.235~2.347 0.002 1.672 1.214~2.315 病理分期 0.000 2.335 1.639~3.328 < 0.001 2.137 1.499~3.046 危险程度分级 < 0.001 1.896 1.494~2.405 < 0.001 1.729 1.365~2.186 FIB-NLR评分 < 0.001 2.468 1.975~3.086 < 0.001 2.327 1.872~2.894 淋巴细胞 0.124 0.603 0.313~1.152 0.231 1.263 0.863~1.844 中性粒细胞 0.195 1.287 0.878~1.886 0.063 0.537 0.281~1.028 FIB < 0.001 3.026 2.139~4.218 < 0.001 2.814 1.989~3.982 NLR值 < 0.001 3.092 2.182~4.382 < 0.001 3.317 2.334~4.715 表 3 影响PCa患者预后的多因素Cox回归分析
变量 DFS OS P HR 95%CI P HR 95%CI tPSA 0.115 1.263 0.945~1.679 0.079 1.301 0.98~1.744 Gleason评分 0.777 0.948 0.662~1.365 0.787 1.053 0.732~1.514 病理分期 < 0.001 2.073 1.685~2.687 < 0.001 1.996 1.634~2.563 危险程度分级 0.058 1.376 0.993~1.908 0.328 1.183 0.846~1.654 FIB-NLR评分 < 0.001 2.237 1.753~2.852 < 0.001 2.112 1.658~2.685 -
[1] Xie DD, Chen YH, Xu S, et al. Low vitamin D status is associated with inflammation in patients with prostate cancer[J]. Oncotarget, 2017, 8(13): 22076-22085. doi: 10.18632/oncotarget.16195
[2] Szor DJ, Roncon Dias A, Pereira MA, et al. Neutrophil-lymphocyte ratio is associated with prognosis in patients who underwent potentially curative resection for gastric cancer[J]. J Surg Oncol, 2018, 117(5): 851-857. doi: 10.1002/jso.25036
[3] Wang H, Zhao J, Zhang M, et al. The combination of plasma fibrinogen and neutrophil lymphocyte ratio(F-NLR)is a predictive factor in patients with resectable non small cell lung cancer[J]. J Cell Physiol, 2018, 233(5): 4216-4224. doi: 10.1002/jcp.26239
[4] Kakehi Y, Sugimoto M, Taoka R. Evidenced-based clinical practice guideline for prostate cancer(summary: Japanese Urological Association, 2016 edition)[J]. Int J Urol, 2017, 24(9): 648-666. doi: 10.1111/iju.13380
[5] Kimura T, Egawa S. Epidemiology of prostate cancer in Asian countries[J]. Int J Urol, 2018, 25(6): 524-531. doi: 10.1111/iju.13593
[6] Dirican N, Karakaya YA, Gunes S, et al. Association of intra-tumoral tumour-infiltrating lymphocytes and neutrophil-to-lymphocyte ratio is an independent prognostic factor in non-small cell lung cancer[J]. Clin Respir J, 2017, 11(6): 789-796. doi: 10.1111/crj.12417
[7] Liu X, Liu Z, Lin E, et al. A cumulative score based on preoperative fibrinogen and the neutrophil-lymphocyte ratio to predict outcomes in resectable gastric cancer[J]. Cancer Manag Res, 2018, 10: 3007-3014. doi: 10.2147/CMAR.S174656
[8] Kijima T, Arigami T, Uchikado Y, et al. Combined fibrinogen and neutrophil-lymphocyte ratio as a prognostic marker of advanced esophageal squamous cell carcinoma[J]. Cancer Sci, 2017, 108(2): 193-199. doi: 10.1111/cas.13127
[9] Lee S, Huh SJ, Oh SY, et al. Clinical significance of coagulation factors in operable colorectal cancer[J]. Oncol Lett, 2017, 13(6): 4669-4674. doi: 10.3892/ol.2017.6058
[10] Liu Z, Guo H, Gao F, et al. Fibrinogen and D-dimer levels elevate in advanced hepatocellular carcinoma: High pretreatment fibrinogen levels predict poor outcomes[J]. Hepatol Res, 2017, 47(11): 1108-1117. doi: 10.1111/hepr.12848
[11] 冷区, 苏维, 李军, 等. 血浆纤维蛋白原水平与前列腺癌临床病理特征的关系研究[J]. 中华腔镜泌尿外科杂志(电子版), 2020, 14(1): 12-15. https://www.cnki.com.cn/Article/CJFDTOTAL-ZHQJ202001004.htm
[12] Shimada H, Takiguchi N, Kainuma O, et al. High preoperative neutrophillymphocyte ratio predicts poor survival in patients with gastric cancer[J]. Gastric Cancer, 2010, 13(3): 170-176. doi: 10.1007/s10120-010-0554-3
[13] Keizman D, Ish-Shalom M, Huang P, et al. The association of pre-treatment neutrophil to lymphocyte ratio with response rate, progression free survival and overall survival of patients treated with sunitinib for metastatic renal cell carcinoma[J]. Eur J Cancer, 2012, 48(2): 202-208. doi: 10.1016/j.ejca.2011.09.001
[14] 陈一鸣, 徐仁芳, 许贤林, 等. 血小板淋巴细胞比和中性粒细胞淋巴细胞比对前列腺癌内分泌治疗后早期去势抵抗预测价值的研究[J]. 中华泌尿外科杂志, 2017, 38(2): 110-114.
[15] 张鹏举, 袁静, 耿彪, 等. 术前NLR、PLR及RDW预测前列腺癌患者术后复发转移的价值[J]. 现代肿瘤医学, 2022, 30(6): 1047-1051. https://www.cnki.com.cn/Article/CJFDTOTAL-SXZL202206019.htm
[16] Liu X, Liu Z, Lin E, et al. A cumulative score based on preoperative fibrinogen and the neutrophil-lymphocyte ratio to predict outcomes in resectable gastric cancer[J]. Cancer Manag Res, 2018, 10: 3007-3014. doi: 10.2147/CMAR.S174656
[17] Arigami T, Uenosono Y, Matsushita D, et al. Combined fibrinogen concentration and neutrophil-lymphocyte ratio as a prognostic marker of gastric cancer[J]. Oncol Lett, 2016, 11(2): 1537-1544. doi: 10.3892/ol.2015.4049
[18] Kijima T, Arigami T, Uchikado Y, et al. Combined fibrinogen and neutrophil-lymphocyte ratio as a prognostic marker of advanced esophageal squamous cell carcinoma[J]. Cancer Sci, 2017, 108(2): 193-199. doi: 10.1111/cas.13127
-





 下载:
下载: