Clinical features and prognosis in patients with testicular yolk sac tumor: a SEER Database analysis
-
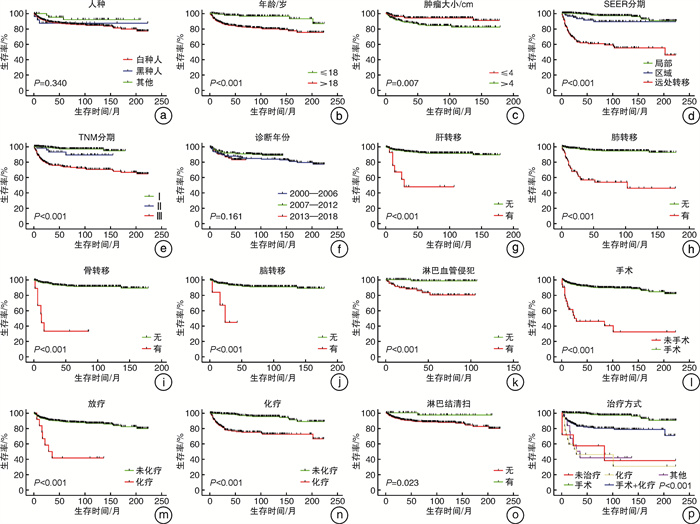
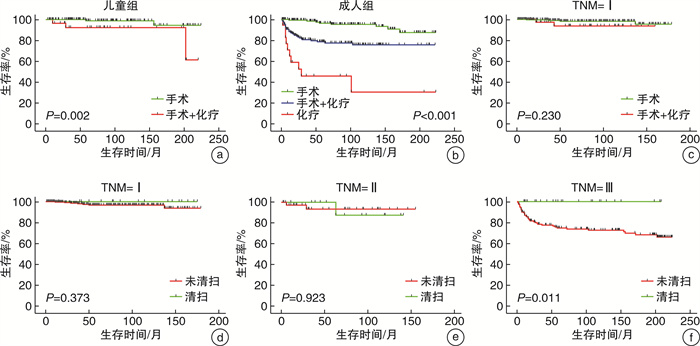
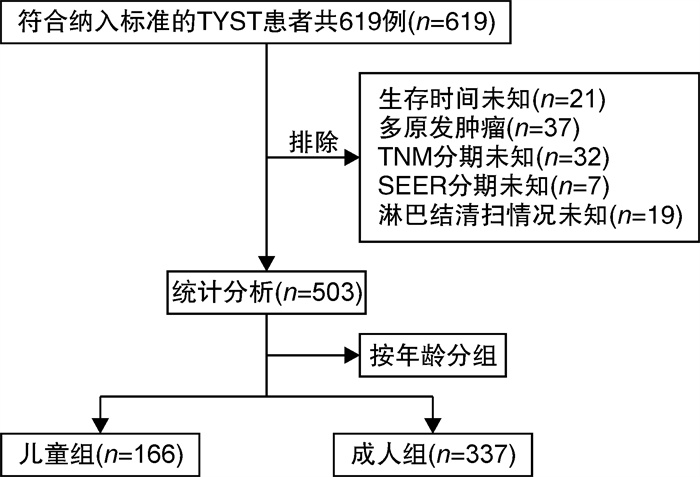
摘要: 目的 基于美国监测、流行病学和结局数据库(SEER数据库)分析男性睾丸卵黄囊瘤(TYST)患者的临床特征、预后及影响因素。方法 使用SEER数据库收集2000—2018年诊断为TYST的患者作为研究对象,根据患者年龄分为儿童组(≤18岁)和成人组(>18岁),采用卡方检验对比两组患者病例构成比,采用Kaplan-Meier法绘制生存曲线并用log-rank法进行检验,采用单因素和多因素Cox回归模型分析其预后影响因素。结果 共503例TYST患者纳入本研究,其中儿童组166例,成人组337例,儿童和成人组TYST患者的3、5、10年总生存率(overall survival,OS)分别为97.3%、96.3%、93.0%和84.9%、82.3%、78.9%。儿童组单纯手术治疗者5年OS优于手术联合化疗者(98.8% vs 92.2%,P=0.02);成人组单纯手术治疗者(96.3%)5年OS优于手术联合化疗者(78.6%),也优于单纯化疗者(45.9%)(均P < 0.001)。单因素和多因素分析结果显示行淋巴结清扫(HR=0.086,95%CI:0.012-0.625,P=0.015)为所有患者的预后良好因素;淋巴血管侵犯(HR=11.924,95%CI:1.537-92.497,P=0.018)和SEER分期位于远处转移(HR=12.374,95%CI:6.199-24.700,P < 0.001)为预后不良因素。结论 TYST是极为罕见的恶性肿瘤,预后不佳。儿童与成人患者在一般临床特征、治疗及预后方面有较大差异。淋巴结清扫、SEER分期及淋巴血管侵犯是TYST重要的预后独立影响因素。Abstract: Objective To investigate the clinical features, prognosis, and prognostic factors of patients with testicular yolk sac tumor(TYST) based upon the database of National Cancer Institute's Surveillance, Epidemiology, and End Results(SEER).Methods Patients diagnosed as TYST from 2000 to 2018 were extracted from the SEER database. Patients were divided into an adult(>18 years) and pediatric(≤18 years) cohort for comparison. Chi-squared tests were used to examine the categorical variables between the two groups. Survival analysis was assessed by the Kaplan-Meier methods, and the differences between survival curves were analyzed using the log-rank test. Univariate and multivariate Cox regression analyses were used to evaluate prognostic factors.Results A total of 503 cases were included in the study(166 children, 337 adults). The overall 3-, 5-and 10-year survival rates of pediatric patients were 97.3%、96.3%、93.0%, respectively; The overall 3-, 5-and 10-year survival rates of adult patients were 84.9%、82.3%、78.9%, respectively. Pediatric patients with surgery had a significantly better survival than those with surgery plus chemotherapy(5-year OS: 98.8% vs 92.2%, P=0.02). Adult patients with surgery had a significantly better survival than those with surgery plus chemotherapy and chemotherapy only(5-year OS: 96.3% vs 78.6%, 96.3% vs 45.9%, all P < 0.001). The results of the univariate and multivariate Cox regression analysis indicated that lymph node dissection was good prognostic factors(HR=0.086, 95%CI: 0.012-0.625, P=0.015), while lymphovascular invasion(HR=11.924, 95%CI: 1.537-92.497, P=0.018) and distant metastasis(HR=12.374, 95%CI: 6.199-24.700, P < 0.001) were poor prognostic factors for TYST patients.Conclusion TYST is an extremely rare malignancy with poor prognosis. The clinicopathological characteristics, outcomes and prognostic factors differed among pediatric patients compared to adult patients. Lymph node dissection, SEER stage and lymphovascular invasion are important independent prognostic factors for TYST patients.
-
Key words:
- testis /
- yolk sac tumor /
- SEER database /
- prognosis /
- surgery /
- RPLND
-

-
表 1 儿童及成人TYST患者一般临床资料比较
例(%) 变量 儿童组(166例) 成人组(337例) P值 变量 儿童组(166例) 成人组(337例) P值 人种 0.006 脑转移 0.041 白种人 132(79.5) 301(89.3) 无 137(82.5) 249(73.9) 黑种人 10(6.0) 15(4.5) 有 0(0) 6(1.8) 其他 24(14.5) 21(6.2) 未知 29(17.5) 82(24.3) 诊断年份 0.066 肺转移 < 0.001 2000—2006年 49(29.5) 90(26.7) 无 132(79.5) 216(64.1) 2007—2012年 73(44.0) 123(36.5) 有 5(3.0) 53(15.7) 2013—2018年 44(26.5) 124(33.4) 未知 29(17.5) 68(20.2) 肿瘤大小 < 0.001 肝转移 0.005 ≤4 cm 95(57.2) 110(32.6) 无 137(82.5) 242(71.8) >4 cm 35(21.1) 154(45.7) 有 0(0) 13(3.9) 未知 36(21.7) 73(21.7) 未知 29(17.5) 82(24.3) 手术 < 0.001 淋巴血管侵犯 0.903 未手术 0(0) 29(8.6) 无 34(20.5) 66(19.6) 手术 166(100.0) 308(91.4) 有 27(16.3) 60(17.8) 淋巴结清扫 < 0.001 未知 105(63.3) 211(62.6) 无 156(94.0) 258(83.8) SEER分期 有 10(6.0) 50(16.2) 局部 142(85.5) 163(48.4) < 0.001 放疗 0.353 区域 12(7.2) 67(19.9) 未放疗 164(98.8) 327(97.0) 远处转移 12(7.2) 107(31.8) 放疗 2(1.2) 10(3.0) TNM分期 < 0.001 化疗 < 0.001 Ⅰ 118(71.1) 141(41.8) 未化疗 135(81.3) 150(44.5) Ⅱ 11(6.6) 43(12.8) 化疗 31(18.7) 187(55.5) Ⅲ 37(22.3) 153(45.4) 骨转移 0.017 治疗方式 < 0.001 无 137(82.5) 246(73.0) 未治疗 0(0) 7(2.1) 有 0(0) 9(2.7) 手术 135(81.3) 140(41.5) 未知 29(17.5) 82(24.3) 化疗 0(0) 18(5.3) 手术+化疗 29(17.5) 162(48.1) 其他 2(1.2) 10(3.0) 表 2 影响TYST患者预后的单因素和多因素Cox回归分析
变量 单因素分析 多因素分析 HR(95%CI) P值 HR(95%CI) P值 人种 黑种人 1.045(0.327~3.337) 0.941 其他 0.432(0.135~1.378) 0.156 诊断年份 2007-2012年 0.652(0.356~1.194) 0.166 2013-2018年 1.175(0.623~2.215) 0.618 肿瘤>4 cm 2.511(1.261~4.998) 0.009 年龄>18岁 4.620(2.110~10.116) < 0.001 手术 0.130(0.075~0.227) < 0.001 淋巴结清扫 0.110(0.015~0.795) 0.029 0.086(0.012~0.625) 0.015 放疗 5.786(2.632~12.720) < 0.001 化疗 5.539(3.107~9.873) < 0.001 骨转移 13.859(5.714~33.616) < 0.001 脑转移 8.784(2.669~28.906) < 0.001 肺转移 11.612(6.253~21.565) < 0.001 肝转移 7.833(3.233~18.977) < 0.001 淋巴血管侵犯 15.680(2.039~120.603) 0.008 11.924(1.537~92.497) 0.018 SEER分期 区域 2.611(1.012~6.738) 0.047 2.645(1.005~6.964) 0.049 远处转移 14.651(7.595~28.263) < 0.001 12.374(6.199~24.700) < 0.001 TNM分期 Ⅱ 3.074(0.900~10.506) 0.073 Ⅲ 10.563(4.797~23.258) < 0.001 治疗方式 手术 0.05(0.016~0.159) < 0.001 化疗 1.134(0.355~3.623) 0.832 手术+化疗 0.310(0.110~0.873) 0.027 -
[1] 陈子英, 徐国栋, 张富义, 等. 52例儿童睾丸肿瘤的临床特点分析[J]. 临床泌尿外科杂志, 2021, 36(2): 116-119. https://www.cnki.com.cn/Article/CJFDTOTAL-LCMW202102007.htm
[2] Thakur S, Kakkar A, Jana M, et al. Pediatric primary yolk sac tumour of the kidney: recommendations for pretreatment diagnosis[J]. Fetal Pediatr Pathol, 2022, 10: 1-8. http://www.tandfonline.com/doi/full/10.1080/15513815.2022.2042631
[3] Liu W, Ma Y, Tang B, et al. Predictive model of early death of resectable pancreatic ductal adenocarcinoma after curative resection: A SEER-Based Study[J]. Cancer Control, 2022, 29: 1389464395.
[4] Trabert B, Chen J, Devesa SS, et al. International patterns and trends in testicular cancer incidence, overall and by histologic subtype, 1973-2007[J]. Andrology, 2015, 3(1): 4-12. doi: 10.1111/andr.293
[5] 李兵兵, 顾朝辉, 贾占奎, 等. 腹腔镜腹膜后淋巴结清扫术治疗临床Ⅰ~Ⅱ期睾丸非精原细胞瘤的疗效观察[J]. 中华泌尿外科杂志, 2015, 30(9): 801-803. https://www.cnki.com.cn/Article/CJFDTOTAL-LCMW201509011.htm
[6] Alshamsi H, Sarhan OM, Almatar A, et al. Unusual presentation, relapse, and metastasis of a pediatric testicular yolk sac tumor: case report[J]. Urology, 2021, 149: e40-e43. doi: 10.1016/j.urology.2020.10.014
[7] Kato N, Tamura G, Fukase M, et al. Hypermethylation of the RUNX3 gene promoter in testicular yolk sac tumor of infants[J]. Am J Pathol, 2003, 163(2): 387-391. doi: 10.1016/S0002-9440(10)63668-1
[8] Salonen J, Rajpert-De ME, Mannisto S, et al. Differential developmental expression of transcription factors GATA-4 and GATA-6, their cofactor FOG-2 and downstream target genes in testicular carcinoma in situ and germ cell tumors[J]. Eur J Endocrinol, 2010, 162(3): 625-631. doi: 10.1530/EJE-09-0734
[9] Geng R, Zheng Z, Lin Y, et al. Clinical characteristics and prognostic factors of male yolk sac tumor: a Surveillance, Epidemiology, and End Results program study[J]. World J Urol, 2021, 39(4): 1211-1217. doi: 10.1007/s00345-020-03311-y
[10] 于顺利, 罗彬杰, 翟天元, 等. 儿童与成人单纯性睾丸卵黄囊瘤临床特点对比分析[J]. 中华男科学杂志, 2019, 25(2): 144-149. https://www.cnki.com.cn/Article/CJFDTOTAL-NKXB201902010.htm
[11] 包楠, 张晓伦, 刘菁. 小儿卵黄囊瘤的诊断与治疗[J]. 中华小儿外科杂志, 2011, 10(1): 10-12. https://cpfd.cnki.com.cn/Article/CPFDTOTAL-GZKX201008003794.htm
[12] Kliesch S, Schmidt S, Wilborn D, et al. Management of germ cell tumours of the testes in adult patients: german clinical practice guideline, PART Ⅱ-recommendations for the treatment of advanced, recurrent, and refractory disease and extragonadal and sex cord/stromal tumours and for the management of follow-up, toxicity, quality of life, palliative care, and supportive therapy[J]. Urol Int, 2021, 105(3-4): 181-191. doi: 10.1159/000511245
[13] Wei Y, Wu S, Lin T, et al. Testicular yolk sac tumors in children: a review of 61 patients over 19 years[J]. World J Surg Oncol, 2014, 12: 400.
[14] Grady RW, Ross JH, Kay R. Patterns of metastatic spread in prepubertal yolk sac tumor of the testis[J]. J Urol, 1995, 153(4): 1259-1261.
[15] Albers P, Albrecht W, Algaba F, et al. Guidelines on testicular cancer: 2015 update[J]. Eur Urol, 2015, 68(6): 1054-1068.
-




 下载:
下载: