Safety and efficacy of percutaneous plasma resection of renal cyst roofing in the treatment of renal cyst
-
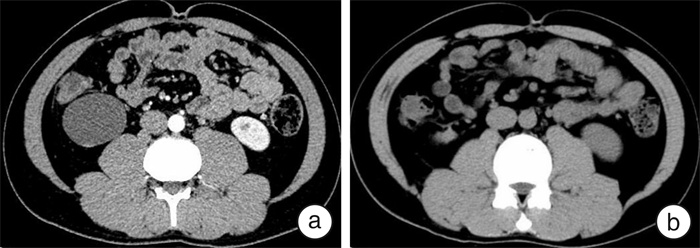
摘要: 目的 探讨经皮等离子电切镜囊肿去顶术治疗肾囊肿的安全性及有效性。方法 回顾性分析2020年1月—2021年5月深圳市人民医院收治的11例经CT检查确诊为单纯性肾囊肿且满足手术指征的患者,男4例,女7例。中位年龄46(35,62)岁。所有患者均因体检发现,经增强CT确诊为单纯性肾囊肿,非腹侧。囊肿最大径中位数7.52(6.26,8.21) cm。术中在超声定位下行经皮肾穿刺后,用等离子电切镜分离切除囊肿壁,术后留置引流管。同时,将其与15例同期采取传统腹腔镜下肾囊肿去顶减压术的患者临床资料进行比较。结果 26例手术均顺利完成,无严重出血、尿漏、肾实质或邻近器官血管损伤等并发症。等离子电切镜组和腹腔镜组手术时间[47(42,55) min vs 68(35,102) min]、引流管拔除时间[1(1,2) d vs 2(2,4) d]、术后住院时间[1(1,2) d vs 2(2,4) d]、住院费用[0.92(0.82,1.26)万元vs 1.34(1.18,1.56)万元]、疼痛评分[2(2,3)分vs 3(2,4)分],差异均有统计学意义(P < 0.05)。等离子电切镜组和腹腔镜组术后中位随访时间分别为12(10,18)个月和15(9,20)个月,均无囊肿复发。结论 经皮等离子电切镜治疗单纯性肾囊肿安全、有效,具有手术时间短、创伤小、患者恢复快、住院时间短且费用低等优势。Abstract: Objective To investigate the safety and efficacy of percutaneous plasma electron microscopy cyst debulking for renal cysts.Methods A retrospective analysis was made on 11 cases of simple renal cyst confirmed by CT examination in Shenzhen People's Hospital from January 2020 to May 2021, including 4 males and 7 females. The median age was 46 (35, 62) years. All patients were diagnosed as simple renal cyst, not ventral, by enhanced CT due to physical examination findings. The median diameter of cyst was 7.52 (6.26, 8.21) cm. During the operation, after percutaneous renal puncture under ultrasonic localization, the cyst wall was separated and removed with plasma resectoscope, and a drainage tube was retained after the operation. At the same time, it was compared with the clinical data of 15 patients who were treated with traditional laparoscopic unroofing decompression of renal cysts at the same time.Results The operation was successfully completed in all 26 cases without severe bleeding, urine leakage, renal parenchyma or adjacent organ vascular injury or other complications. The operation time (47[42, 55] min vs 68[35, 102] min), drainage tube removal time (1[1, 2] d vs 2[2, 4] d), postoperative hospitalization time(1[1, 2] d vs 2[2, 4] d), hospitalization expense (9200[8200, 12600] yuan vs 13400[11800, 15600] yuan), and pain score(2[2, 3] points vs 3[2, 4] points) in the plasma resectoscope group and laparoscope group were statistically significant (P < 0.05). The median follow-up time was 12 (10, 18) months and 15 (9, 20) months in the plasma resectoscope group and laparoscope group, respectively. No recurrence of cysts was found.Conclusion Percutaneous plasma electron microscopy is safe and effective in the treatment of simple renal cysts, with the advantages of short operation time, little trauma, quick recovery of patients, short hospital stay and low cost.
-
Key words:
- electrosurgical resection /
- simple renal cyst /
- safety /
- efficacy
-

-
[1] Ozveren B, Onganer E, Türkeri LN. Simple Renal Cysts: Prevalence, Associated Risk Factors and Follow-Up in a Health Screening Cohort[J]. Urol J, 2016, 13(1): 2569-2575.
[2] Bas O, Nalbant I, Can Sener N, et al. Management of renal cysts[J]. JSLS, 2015, 19(1): e2014.00097. doi: 10.4293/JSLS.2014.00097
[3] Hommos MS, Glassock RJ, Rule AD. Structural and Functional Changes in Human Kidneys with Healthy Aging[J]. J Am Soc Nephrol, 2017, 28(10): 2838-2844. doi: 10.1681/ASN.2017040421
[4] Choi JD. Clinical characteristics and long-term observation of simple renal cysts in a healthy Korean population[J]. Int Urol Nephrol, 2016, 48(3): 319-324. doi: 10.1007/s11255-015-1186-7
[5] Skolarikos A, Laguna MP, de la Rosette JJ. Conservative and radiological management of simple renal cysts: a comprehensive review[J]. BJU Int, 2012, 110(2): 170-178. doi: 10.1111/j.1464-410X.2011.10847.x
[6] Li YZ, Li MX, Wang T, et al. Efficacy and safety of alcohol sclerotherapy involving single-session multiple injections to treat simple renal cysts: a multicenter, prospective, randomized, controlled trial[J]. Chin Med J(Engl), 2013, 126(5): 803-807.
[7] Kavoussi LR, Clayman RV, Mikkelsen DJ, et al. Ureteronephroscopic marsupialization of obstructing peripelvic renal cyst[J]. J Urol, 1991, 146(2): 411-414.
[8] Shen J, Chen Y, Wang R. Efficacy and Complication of Flexible Ureteroscopic Holmium Laser Incision for Simple Renal Cysts: A Retrospective Study[J]. J Endourol, 2019, 33(11): 881-886. doi: 10.1089/end.2019.0515
[9] Chen Y, Wang R, Shen X, et al. Ultrasonography-assisted flexible ureteroscope for the treatment of parapelvic renal cysts: A comparison between the 1470-nm diode laser and the holmium laser[J]. Exp Ther Med, 2021, 21(2): 172.
[10] Yan KW, Tian XF, Meng N, et al. Flexible ureteroscopy with ultrasound guidance for the treatment of parapelvic renal cysts: A complementary approach for locating the cystic wall[J]. BMC Urol, 2022, 22(1): 7. doi: 10.1186/s12894-022-00960-6
[11] Yang D, Xue B, Zang Y, et al. A modified laparoendoscopic single-site renal cyst decortication: single-channel retroperitoneal laparoscopic decortication of simple renal cyst[J]. J Laparoendosc Adv Surg Tech A, 2013, 23(6): 506-510. doi: 10.1089/lap.2012.0411
[12] Korth K. Limits of percutaneous calculus surgery. Results and new possibilities of the percutaneous approach to the kidney[J]. Urologe A, 1984, 23(6): 302-307.
[13] Hong Y, Chen X, Wu M, et al. Percutaneous vs Laparoscopic Treatment for Simple Renal Cysts: A Meta-analysis[J]. J Endourol, 2021, 35(12): 1793-1800. doi: 10.1089/end.2021.0264
[14] Plas EG, Hübner WA. Percutaneous resection of renal cysts: a long-term followup[J]. J Urol, 1993, 149(4): 703-705. doi: 10.1016/S0022-5347(17)36187-6
[15] Korets R, Mues AC, Gupta M. Minimally invasive percutaneous ablation of parapelvic renal cysts and caliceal diverticula using bipolar energy[J]. J Endourol, 2011, 25(5): 769-773. doi: 10.1089/end.2010.0525
[16] 王军, 刘雍, 刘磊, 等. 经皮囊内入路电切去顶术治疗单纯性肾囊肿16例报告[J]. 中华泌尿外科杂志, 2014, 29(10): 889-891. https://www.cnki.com.cn/Article/CJFDTOTAL-LCMW201410013.htm
[17] Hu J, Dirie NI, Yang J, et al. Percutaneous ureteroscopy laser unroofing-a minimally invasive approach for renal cyst treatment[J]. Sci Rep, 2017, 7(1): 14445.
[18] Chen H, Li Y, Zeng F, et al. Percutaneous nephrostomic decortication: a microinvasive surgery for posterior renal cyst[J]. Transl Androl Urol, 2020, 9(6): 2764-2770.
[19] 陈煜, 王荣江, 沈旭峰, 等. 输尿管软镜下1470 nm激光与钬激光开窗内引流术治疗内生性肾囊肿的临床疗效比较[J]. 临床泌尿外科杂志, 2022, 37(3): 189-195. https://lcmw.whuhzzs.com/article/doi/10.13201/j.issn.1001-1420.2022.03.007
-




 下载:
下载: