Micro-ureteroscopy for treatment of ureteral stones in pediatric patients younger than 3 years
-
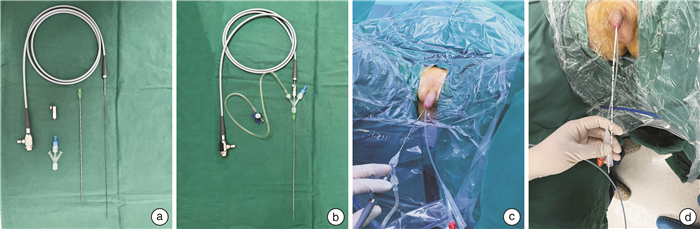
摘要: 目的 评价超微输尿管镜(micro-ureterocopy,m-URS)一期处理3岁以下儿童输尿管结石的有效性和安全性。方法 回顾性分析2018年7月—2022年8月我院收治的34例3岁以下接受m-URS手术的患儿资料。手术在全身麻醉下进行,采用F4.8可视穿刺镜用作m-URS。描述分析患儿术前一般资料、手术资料、结石清除率(SFR)以及术中术后并发症。结果 患儿年龄9~36个月,平均(22.9±9.6)个月;男24例,女10例;结石最大直径0.3~1.5 cm,平均(0.8±0.3) cm;结石CT值400~1420 HU,平均(976±264) HU;伴肾积水28例(82.4%)。m-URS一期手术成功率为79.4%(27/34),输尿管上、中、下段结石手术成功率分别为69.2%、77.8%和91.7%。手术时间15~60 min,平均(33.3±14.0) min;碎石时间8~35 min,平均(16.0±6.2) min;液体灌注量50~800 mL,平均(285±225) mL。23例患儿术后留置输尿管支架管,4例留置输尿管导管。7例患儿因输尿管狭窄、扭曲、结石移位等因素改行二期输尿管镜或经皮肾镜手术。术后2例患儿出现发热,抗炎对症处理好转。术后住院时间2~11 d,平均(3.2±1.6) d。术后1个月SFR为92.6%。27例患儿完成结石处理所需麻醉次数平均为1.8次。结论 m-URS一期处理3岁以下儿童输尿管结石安全有效,具有较高的成功率,m-URS可有效减少患儿麻醉和手术次数,可作为3岁以下儿童输尿管结石处理的首选治疗方案之一。Abstract: Objective To demonstrate the efficacy and safety of micro-ureteroscopy (m-URS) in the treatment of ureteral stones in pediatric patients younger than 3 years.Methods A retrospective analysis was performed on the data of 34 children under 3 years old who received m-URS surgery in our hospital from July 2018 to August 2022. The procedures were performed under general anesthesia using the standard ureteroscopic technique with a micro-ureterocope that has a caliber of 4.8 Fr all along its length. Demographics, perioperative data, stone free rate (SFR) and complications were analyzed.Results The patients'mean age was (22.9±9.6) months (9-36 months), and there were 24 males and 10 females. The mean maximum diameter of the stone was (0.8±0.3) cm (0.3-1.5 cm). The mean CT value of calculi was (976±264) HU (400-1420 HU), and 28 cases (82.4%) were accompanied by hydronephrosis. The one-stage success rate of m-URS was 79.4% (27/34), and the success rates for upper, middle and lower ureter stones were 69.2%, 77.8% and 91.7%, respectively. The mean operation time was (33.3±14.0) min (15-60 min), and the mean lithotripsy time was (16.0±6.2) min (8-35 min). The mean irrigation fluid volume was (285±225) mL (50-800 mL). Ureteral stents were indwelled in 23 cases and ureteral catheters were indwelled in 4 cases. Seven cases underwent second-stage ureteroscopic surgery or percutaneous nephrolithotomy due to ureteral stricture, distortion or stone displacement. As a postoperative complication, fever was observed in two cases and required antibiotic treatment. The mean postoperative hospital stay was (3.2±1.6) days (2-11 days). The SFR at 1 month after operation was 92.6%. The mean number of anesthesia required for stone treatment in 27 children was 1.8 times.Conclusion Micro-URS is safe and effective for the treatment of ureteral stones in children with a high success rate. It can effectively reduce the number of anesthesia and surgery in children, and can be used as one of the first choices in pediatric patients under three years of age.
-
Key words:
- micro-ureteroscopy /
- ureteral stone /
- pediatric
-

-
[1] 中华医学会泌尿外科学分会结石学组, 中国泌尿系结石联盟. 儿童泌尿系结石诊疗中国专家共识[J]. 中华泌尿外科杂志, 2021, 42(2): 81-88. doi: 10.3760/cma.j.cn112330-20210111-00017
[2] 李玮, 满立波, 王海, 等. 经尿道输尿管软镜碎石术前留置双J管预扩张输尿管时间的临床分析[J]. 临床泌尿外科杂志, 2022, 37(2): 90-94. https://www.cnki.com.cn/Article/CJFDTOTAL-LCMW202202003.htm
[3] Caballero-Romeu JP, Budia-Alba A, Galan-Llopis JA, et al. Microureteroscopy in Children: Two First Cases[J]. J Endourol Case Rep, 2016, 2(1): 44-47. doi: 10.1089/cren.2016.0005
[4] Baydilli N, Selvi, Akınsal EC, et al. Micro-ureteroscopy(m-URS)for treatment of upper ureteral stones in children: A new, different approach[J]. Turk J Urol, 2021, 47(3): 248-249. doi: 10.5152/tud.2020.20452
[5] Parente A, Ortiz R, Fernández-Bautista B, et al. Micro-Ureteroscopy as a Treatment of Renal Pelvis Lithiasis in Young Children[J]. Front Pediatr, 2021, 9: 593743. doi: 10.3389/fped.2021.593743
[6] Reddy SV. Effect of general anesthetics on the developing brain[J]. J Anaesthesiol Clin Pharmacol, 2012, 28(1): 6-10. doi: 10.4103/0970-9185.92426
[7] Pinyavat T, Saraiya NR, Chen J, et al. Anesthesia Exposure in Children: Practitioners Respond to the 2016 FDA Drug Safety Communication[J]. J Neurosurg Anesthesiol, 2019, 31(1): 129-133. doi: 10.1097/ANA.0000000000000545
[8] Sun LS, Li G, Miller TL, et al. Association Between a Single General Anesthesia Exposure Before Age 36 Months and Neurocognitive Outcomes in Later Childhood[J]. JAMA, 2016, 315(21): 2312-2320. doi: 10.1001/jama.2016.6967
[9] Atar M, Sancaktutar AA, Penbegul N, et al. Comparison of a 4.5 F semi-rigid ureteroscope with a 7.5 F rigid ureteroscope in the treatment of ureteral stones in preschool-age children[J]. Urol Res, 2012, 40(6): 733-738. doi: 10.1007/s00240-012-0489-8
[10] Kim SS, Kolon TF, Canter D, et al. Pediatric flexible ureteroscopic lithotripsy: the children's hospital of Philadelphia experience[J]. J Urol, 2008, 180(6): 2616-2619;discussion 2619. doi: 10.1016/j.juro.2008.08.051
[11] Utanǧaç MM, Sancaktutar AA, Tepeler A. Micro-ureteroscopy for the treatment of distal ureteral calculi in children[J]. J Pediatr Surg, 2017, 52(3): 512-516. doi: 10.1016/j.jpedsurg.2016.11.032
[12] 但超, 王黎, 姚启盛, 等. 微输尿管镜治疗儿童输尿管下段结石11例疗效分析[J]. 现代泌尿外科杂志, 2021, 26(6): 510-513. doi: 10.3969/j.issn.1009-8291.2021.06.013
[13] Caballero-Romeu JP, Galán-Llopis JA, Soria F, et al. Micro-ureteroscopy vs. ureteroscopy: effects of miniaturization on renal vascularization and intrapelvic pressure[J]. World J Urol, 2018, 36(5): 811-817. doi: 10.1007/s00345-018-2205-y
[14] Caballero-Romeu JP, Galán-Llopis JA, Soria F, et al. Outcomes of ureteroscopy miniaturization on tissue damage and tissue hypoxia in a pig model[J]. Sci Rep, 2018, 8(1): 431. doi: 10.1038/s41598-017-18885-8
[15] Hernández RP, Caballero Romeu JP, Galiano Baena JF, et al. Technical considerations about micro-ureteroscopy in children[J]. J Pediatr Surg, 2017, 52(7): 1216. doi: 10.1016/j.jpedsurg.2017.03.053
-




 下载:
下载: