Advantages and technical points of ThuLEP with preservation of dorsal longitudinal urethral mucosa for benign prostatic hyperplasia with small-medium gland
-
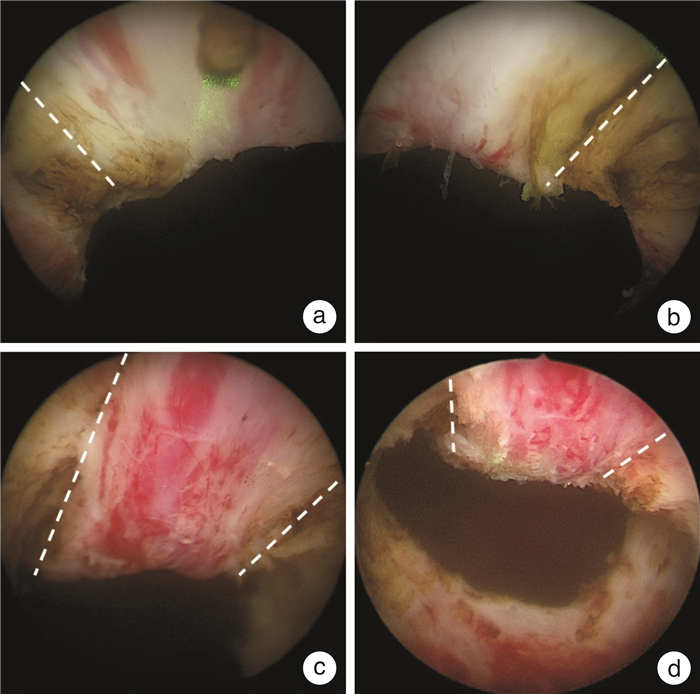
摘要: 经尿道前列腺铥激光剜除术(ThuLEP)在临床上已得到广泛应用,但剜除术后出现暂时性尿失禁、膀胱颈挛缩和尿路刺激症状等并发症的风险仍较高,限制了该技术的推广。本文提出保留背侧纵行尿道黏膜的ThuLEP在治疗中小体积良性前列腺增生中具有独特的优势,既能降低术后暂时性尿失禁、膀胱颈挛缩和肉眼血尿的发生率,又能减轻术后尿路刺激症状。本文就保留背侧纵行尿道黏膜的ThuLEP的技术要点进行阐述。Abstract: Thulium laser enucleation of prostate (ThuLEP) has been widely used clinically. However, the risk of complications such as temporary urinary incontinence, bladder neck contracture and urinary tract irritation after enucleation remains high, which limits the spread of the technology. In the article, it was proposed that ThuLEP with preservation of dorsal longitudinal urethral mucosa has unique advantages in the treatment of BPH with small-medium volume, which can not only reduce the incidence of temporary urinary incontinence, bladder neck contracture and gross hematuria, but also reduce the symptoms of postoperative urinary tract irritation. At the same time, the technical points of ThuLEP with preservation of dorsal longitudinal urethral mucosa were elaborated in the article.
-

-
表 1 两组BPH患者基本情况比较
X±S 项目 常规组
(48例)改良组
(54例)P值 年龄/岁 70.3±4.5 68.6±3.6 0.565 Qmax/(mL/s) 8.6±2.7 7.8±2.3 0.642 IPSS评分 20.6±2.6 21.5±3.5 0.439 QoL评分 4.5±1.3 4.8±1.6 0.416 OAB症状评分 1.4±0.7 1.2±0.5 0.652 残余尿/mL 128.5±28.6 137.6±30.8 0.319 PSA/(ng/mL) 2.4±1.1 2.7±1.2 0.298 经直肠前列腺体积/mL 39.3±9.6 41.5±10.8 0.484 注:Qmax为最大尿流率,IPSS为国际前列腺症状评分,QoL为生活质量评分,OAB为膀胱过度活动症,PSA为前列腺特异性抗原。 表 2 两组BPH患者术中和术后情况比较
X±S 项目 常规组
(48例)改良组
(54例)P值 手术时间/min 26.3±8.3 29.4±9.5 0.431 剜除时间/min 20.5±4.5 22.8±5.8 0.543 剜除腺体重量/g 20.4±6.1 21.7±7.9 0.468 血红蛋白下降值/(g/L) 2.7±1.9 2.6±2.2 0.254 术后住院时间/d 1.0±0.3 1.3±0.2 0.097 术后留置尿管时间/d 2.4±1.2 2.2±1.1 0.463 Qmax/(mL/s) 21.6±8.7 20.2±10.2 0.327 IPSS评分 6.0±2.2 5.4±1.7 0.289 QoL评分 1.4±0.6 1.7±0.8 0.148 残余尿/mL 5.9±4.3 7.0±5.1 0.154 OAB症状评分 8.0±2.3 2.4±1.2 0.032 肉眼血尿/例(%) 9(18.8) 3(5.6) 0.039 暂时性尿失禁/例(%) 10(20.8) 2(3.7) 0.007 膀胱颈挛缩/例(%) 4(8.3) 0 0.030 注:两组均行“两叶法”ThuLEP手术,改良组在常规组手术方式的基础上保留自膀胱颈至前列腺尖部的背侧纵行尿道黏膜。 -
[1] 王成明, 李普, 张倩, 等. 经尿道前列腺钬激光剜除术治疗小体积前列腺增生的疗效和安全性分析[J]. 中华泌尿外科杂志, 2021, 42(11): 839-843. https://www.cnki.com.cn/Article/CJFDTOTAL-TJYX202101015.htm
[2] 安子彦, 符伟军, 宋勇, 等. 经尿道前列腺铥光纤激光分叶剜除术的临床疗效分析[J]. 中华泌尿外科杂志, 2021, 42(11): 834-838.
[3] Fallara G, Capogrosso P, Schifano N, et al. Ten-year follow-up results after holmium laser enucleation of the prostate[J]. Eur Urol Focus, 2021, 7(3): 612-617. doi: 10.1016/j.euf.2020.05.012
[4] 邹志辉, 胡永涛, 张礼刚, 等. 日间手术模式下开展铥激光腔内解剖性前列腺剜除术的临床研究[J]. 微创泌尿外科杂志, 2022, 11(2): 100-105. https://www.cnki.com.cn/Article/CJFDTOTAL-WCMN202202007.htm
[5] Castellani D, Wroclawski ML, Pirola GM, et al. Bladder neck stenosis after transurethral prostate surgery: a systematic review and meta-analysis[J]. World J Urol, 2021, 39(11): 4073-4083. doi: 10.1007/s00345-021-03718-1
[6] Chen YZ, Lin WR, Chow YC, et al. Analysis of risk factors of bladder neck contracture following transurethral surgery of prostate[J]. BMC Urol, 2021, 21(1): 59. doi: 10.1186/s12894-021-00831-6
[7] 黄建文, 罗志强, 曹乃龙, 等. 保留12点纵行尿道黏膜的前列腺钬激光剜除术治疗中小体积BPH的疗效分析[J]. 中华泌尿外科杂志, 2022, 43(4): 261-265.
[8] Fried NM. High-power laser vaporization of the canine prostate using a 110 W Thulium fiber laser at 1.91 microm[J]. Lasers Surg Med, 2005, 36(1): 52-56.
[9] Lumen N, Campos-Juanatey F, Greenwell T, et al. European Association of Urology Guidelines on Urethral Stricture Disease (Part 1)[J]. Eur Urol, 2021, 80(2): 190-200.
-




 下载:
下载: