-
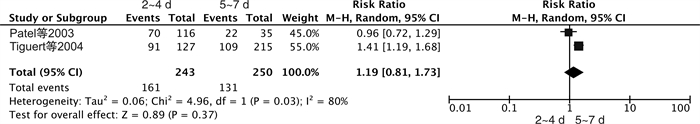
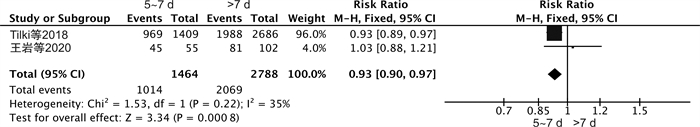
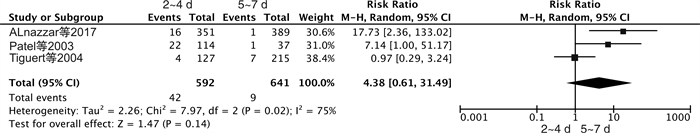
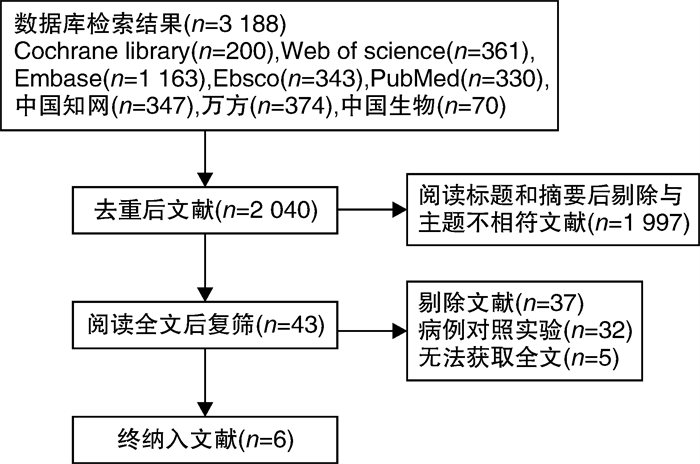
摘要: 目的 系统评价前列腺癌根治术术后不同时间拔除导尿管的临床效果和安全性, 探讨术后拔除尿管的最佳时间。方法 计算机检索PubMed、EBSCO、Web of Science、Cochrane Library、中国生物医学文献数据库、中国知网、万方数据库和维普数据库中关于前列腺癌根治术术后导尿管拔除时间对排尿影响的病例对照研究, 检索时间为建库至2023年2月。所有文献依据纳入和排除标准筛选, 由2名研究者独立完成质量评价, 并采用RvMan 5.4软件进行meta分析。结果 纳入6篇文献, 涉及5959例患者。Meta分析结果显示, 与术后>7 d比较, 5~7 d拔除导尿管可以预防术后尿失禁(RR=0.93, 95%CI: 0.90~0.97, P < 0.05), 术后2~4 d与5~7 d拔除导尿管对尿失禁发生率的影响差异无统计学意义(RR=1.19, 95%CI: 0.81~1.73, P=0.37)。前列腺癌根治术后患者拔除导尿管的时间对尿潴留发生率的影响差异无统计学意义(RR=4.38, 95%CI: 0.61~31.49, P=0.14)。结论 与>7 d比较, 术后5~7 d拔除尿管能降低尿失禁的发生率。前列腺癌根治术后5~7 d内拔除导尿管是预防尿失禁发生的最佳时间。Abstract: Objective To systematically evaluate the clinical effect and safety of different timing of urinary catheter removal after radical prostatectomy, and to explore the best timing of urinary catheter removal after radical prostatectomy.Methods PubMed was searched by computer EBSCO, Web of Science, The Cochrane Library, CNKI, Wanfang, CBM and VIP databases were searched by computer for case-control studies on the effect of different removal time of instillation catheter on urination after radical prostatectomy. The literature was screened according to the inclusion and exclusion criteria, and the quality of the literature was evaluated. RevMan5.4 software was used for meta-analysis.Results Six studies involving 5959 patients were included in the meta-analysis. The results showed that compared with the removal time of urinary catheter >7 days, the removal of urinary catheter within 5-7 days could prevent the occurrence of urinary incontinence (RR=0.93, 95%CI: 0.90-0.97, P < 0.05). There was no significant difference in the incidence of urinary incontinence between 2-4 days and 5-7 days after radical prostatectomy(RR=1.19, 95%CI: 0.81-1.73, P=0.37). However, there was no significant difference in the incidence of urinary retention among different time of catheter removal after radical prostatectomy(RR=4.38, 95%CI: 0.61-31.49, P=0.14).Conclusion Compared with catheter removal time>7 days, catheter removal time 5-7 days can reduce the incidence of urinary incontinence. Therefore, the best time to prevent urinary incontinence is to remove the catheter within 5 to 7 days after radical prostatectomy.
-
Key words:
- radical prostatectomy /
- retained catheter /
- timing of extubation /
- meta-analysis
-

-
表 1 文献质量评价工具——病例对照研究(NOS)
条目 评价标准 研究人群选择 病例定义是否恰当(1分) ①恰当,有独立的确定方法或人员☆;②恰当,如基于档案记录或自我报告;③未描述 病例的代表性(1分) ①连续或有代表性系列病例☆;②有潜在偏倚或未描述 对照的选择(1分) ①与病例同一人群的对照☆;②与病例同一人群的住院人员为对照;③未描述 对照的确定(1分) ①无目标疾病史☆;②未描述来源 组间可比性 设计和统计分析时考虑病例和对照的可比性(2分) ①研究控制了最重要的混杂因素☆;②研究控制了任何其他的混杂因素☆ 暴露因素的测量 暴露因素的确定(1分) ①固定的档案记录☆;②采用结构式访谈且不知访谈者是病例或对照☆;③采用未实施盲法的访谈;④未描述 采用相同方法确定病例和对照组暴露因素(1分) ①是☆;②否 无应答率(1分) ①2组无应答率相同☆;②描述了无应答情况;③2组无应答率不同且未描述 表 2 纳入文献的特征
作者 年份 国家 拔管时间/d 样本量/例 手术方式 结局指标 有无利益冲突 Patel等[6] 2003 美国 3或4
737
231RP 尿潴留、尿失禁 无利益冲突 Alnazari等[7] 2017 加拿大 4
7351
389机器人辅助前列腺切除术 尿失禁、尿潴留 无利益冲突 王岩等[8] 2020 中国 7
1455
102机器人辅助前列腺切除术 尿失禁、尿潴留 无利益冲突 Hao等[9] 2022 中国 7
10
≥14124
88
220机器人辅助前列腺切除术 尿失禁、尿潴留 无利益冲突 Tiguert等[10] 2004 加拿大 4
>4127
215双侧盆腔淋巴结切除术和RP 尿失禁、尿潴留 无利益冲突 Tilki等[11] 2018 德国 ≤7
8~14
≥151409
2285
401RP 尿失禁 无利益冲突 表 3 文献质量评价
条目 Patel等 Alnazari等 王岩等 Hao等 Tiguert等 Tilki等 研究人群选择 病例定义是否恰当 1 1 1 1 1 1 病例的代表性 1 1 1 1 1 1 对照的选择 1 1 1 1 1 1 对照的确定 1 1 1 1 1 1 组间可比性 设计和统计分析时考虑病例 0 0 0 0 0 0 暴露因素的测量 暴露因素的确定 1 1 1 1 1 1 采用相同方法确定病例和对照组暴露因素 1 1 1 1 1 1 无应答率 1 0 1 1 1 1 总分 7 6 7 7 7 7 -
[1] Brassetti A, Proietti F, Cardi A, et al. Removing the urinary catheter on post-operative day 2 after robot-assisted laparoscopic radical prostatectomy: a feasibility study from a single high-volume referral centre[J]. J Robot Surg, 2018, 12(3): 467-473. doi: 10.1007/s11701-017-0765-2
[2] Siegel RL, Miller KD, Fuchs HE, et al. Cancer Statistics, 2021[J]. CA Cancer J Clin, 2021, 71(1): 7-33. doi: 10.3322/caac.21654
[3] Liu X, Yu C, Bi Y, et al. Trends and age-period-cohort effect on incidence and mortality of prostate cancer from 1990 to 2017 in China[J]. Public Health, 2019, 172: 70-80. doi: 10.1016/j.puhe.2019.04.016
[4] 沈群, 杨波, 王燕, 等. 机器人辅助腹腔镜下前列腺癌根治术护理团队的建设和培训[J]. 解放军护理杂志, 2014, 31(22): 58-60. https://www.cnki.com.cn/Article/CJFDTOTAL-JFHL201422025.htm
[5] 屈晓玲, 方汉萍, 陈小芹, 等. 机器人辅助腹腔镜前列腺癌根治性切除术患者快速康复护理[J]. 护理学杂志, 2015, 30(20): 47-48. doi: 10.3870/j.issn.1001-4152.2015.20.047
[6] Patel R, Lepor H. Removal of urinary catheter on postoperative day 3 or 4 after radical retropubic prostatectomy[J]. Urology, 2003, 61(1): 156-160. doi: 10.1016/S0090-4295(02)02105-2
[7] Alnazari M, Zanaty M, Ajib K, et al. The risk of urinary retention following robot-assisted radical prostatectomy and its impact on early continence outcomes[J]. Can UrolAssoc J, 2018, 12(3): E121-E125.
[8] 王岩, 费笑晨, 樊连城, 等. 机器人辅助腹腔镜下根治性前列腺切除术后早期拔除导尿管的临床疗效[J]. 现代泌尿外科杂志, 2020, 25(9): 806-809. doi: 10.3969/j.issn.1009-8291.2020.09.010
[9] Hao H, Chen X, Liu Y, et al. The impact of catheter removal time on urinary continence and overactive bladder symptoms after robot-assisted radical prostatectomy: a retrospective analysis of consecutive 432 cases from a single institution[J]. Transl Androl Urol, 2022, 11(10): 1389-1398. doi: 10.21037/tau-22-397
[10] Tiguert R, Rigaud J, Fradet Y. Safety and outcome of early catheter removal after radical retropubic prostatectomy[J]. Urology, 2004, 63(3): 513-517. doi: 10.1016/j.urology.2003.10.042
[11] Tilki D, Preisser F, Karakiewicz P, et al. The impact of time to catheter removal on short-, intermediate-and long-term urinary continence after radical prostatectomy[J]. World J Urol, 2018, 36(8): 1247-1253. doi: 10.1007/s00345-018-2274-y
[12] 张彦, 余伟, 嵇秀明, 等. 剖宫产术后产妇早期拔除尿管的最佳证据总结[J]. 护士进修杂志, 2022, 37(16): 1472-1477. https://www.cnki.com.cn/Article/CJFDTOTAL-FSJX202216006.htm
[13] 李晓丹, 梁熠, 龚晶晶, 等. 尿管拔除时间对盆底功能障碍性疾病术后尿潴留影响的Meta分析[J]. 现代妇产科进展, 2020, 29(8): 584-587, 592. https://www.cnki.com.cn/Article/CJFDTOTAL-XDFC202008006.htm
[14] 林健. 腹腔镜前列腺癌根治切除术后早期拔除尿管[J]. 中华泌尿外科杂志, 2002, 23(4): 62-63. https://www.cnki.com.cn/Article/CJFDTOTAL-ZHMN200204031.htm
[15] 袁秀群, 孟晓红. 机器人辅助前列腺癌根治术后拔除导尿管时间研究进展[J]. 护理研究, 2017, 31(36): 4612-4615. doi: 10.3969/j.issn.1009-6493.2017.36.007
[16] 杨静, 吴小燕, 卢婕楠, 等. 加速康复外科理念下导尿管早期拔除的研究进展[J]. 加速康复外科杂志, 2019, 2(3): 142-144. https://cdmd.cnki.com.cn/Article/CDMD-10315-1017010742.htm
[17] 尤朝香, 贾梦滢, 李霜, 等. 单孔腹腔镜结直肠癌根治术后早期导尿管拔除的研究进展[J]. 临床医学研究与实践, 2022, 7(10): 193-195. https://www.cnki.com.cn/Article/CJFDTOTAL-YLYS202210054.htm
[18] 孙景茹. 基于快速康复理念指导早期拔除导尿管对腹腔镜手术患者术后恢复的影响[J]. 山西医药杂志, 2021, 50(1): 143-146. https://www.cnki.com.cn/Article/CJFDTOTAL-SXYY202101064.htm
[19] Ramirez D, Ganesan V, Nelson RJ, et al. Reducing Costs for Robotic Radical Prostatectomy: Three-instrument Technique[J]. Urology, 2016, 95: 213-215.
[20] 高丽娟, 吕晓倩. 导尿管拔除后重置原因及预防措施研究进展[J]. 国际护理学杂志, 2021, 40(1): 187-190.
[21] 刘洪娟, 王颖, 尹世玉, 等. 短期留置尿管患者拔管前不进行夹管训练的可行性研究[J]. 护理学杂志, 2018, 33(18): 49-50. https://www.cnki.com.cn/Article/CJFDTOTAL-HLXZ201818017.htm
[22] de Lira G, Fornari A, Cardoso LF, et al. Effects of perioperative pelvic floor muscle training on early recovery of urinary continence and erectile function in men undergoing radical prostatectomy: a randomized clinical trial[J]. Int Braz J Urol, 2019, 45(6): 1196-1203.
[23] Aydın Sayılan A, Özbaş A. The Effect of Pelvic Floor Muscle Training On Incontinence Problems After Radical Prostatectomy[J]. Am J Mens Health, 2018, 12(4): 1007-1015.
[24] 杨超, 陈新, 方露, 等. 腹腔镜输尿管修复术后导尿管留置时间研究: 单中心100例回顾性研究[J]. 临床泌尿外科杂志, 2023, 38(2): 99-102. https://lcmw.chinajournal.net.cn/WKC/WebPublication/paperDigest.aspx?paperID=6506e93e-637d-4333-a055-95709fa7764c
-

| 引用本文: | 高梦昕, 陈媛, 华小玲, 等. 前列腺癌根治术后拔除尿管时间的meta分析[J]. 临床泌尿外科杂志, 2023, 38(7): 500-504. doi: 10.13201/j.issn.1001-1420.2023.07.004 |
| Citation: | GAO Mengxin, CHEN Yuan, HUA Xiaoling, et al. Time of urinary catheter removal after radical prostatectomy: a meta-analysis[J]. J Clin Urol, 2023, 38(7): 500-504. doi: 10.13201/j.issn.1001-1420.2023.07.004 |
- Figure 1.
- Figure 2.
- Figure 3.
- Figure 4.



 下载:
下载: