Single center application of a new baseline assessment model for renal function in the evaluation of renal function after radical or partial nephrectomy
-
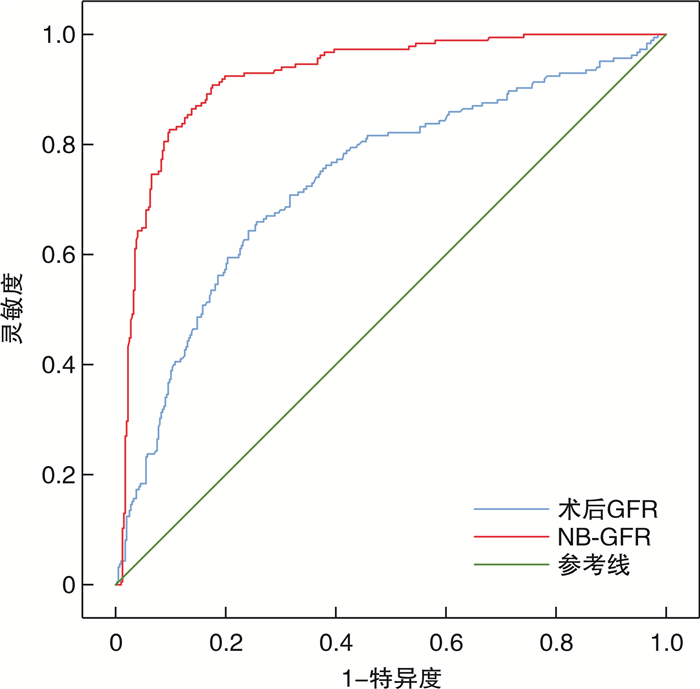
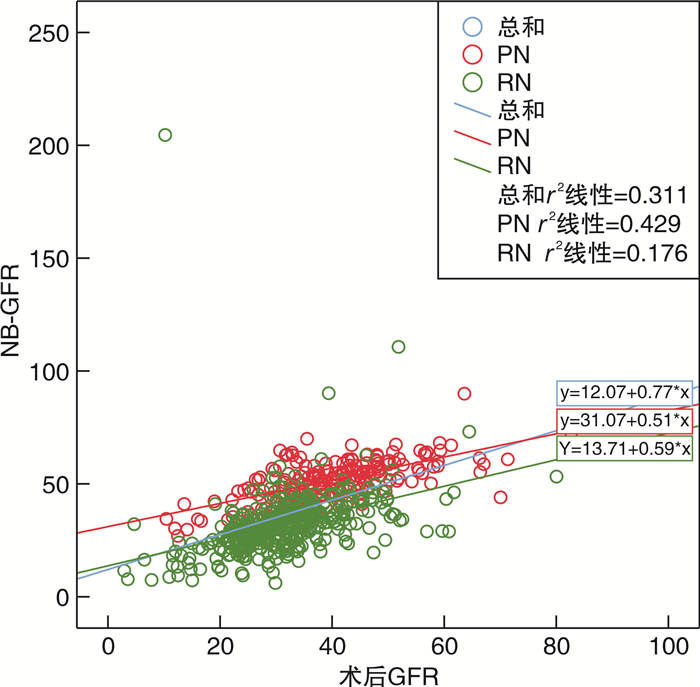
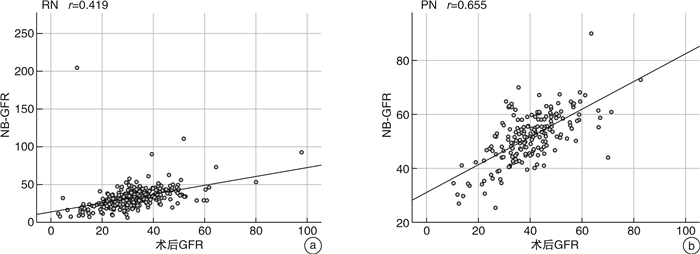
摘要: 目的 检验肾功能新基线评估模型在根治性肾切除术(radical nephrectomy,RN)或肾部分切除术(partial nephrectomy,PN)后评估肾功能的能力,评判其是否适用于中国人群。方法 对广西医科大学第一附属医院2015—2022年进行RN的患者398例及PN的患者185例进行回顾性分析,对肾功能新基线评估模型预测出的术后新基线肾小球滤过率(new baseline glomerular filtration rate,NB-GFR)与患者实际GFR进行相关性分析并进行吻合度检验。结果 RN和PN 2组患者一般信息及临床资料进行检验,结果显示差异无统计学意义。采用Pearson相关评价术后GFR和NB-GFR的关系。行PN术后GFR和NB-GFR存在较强的正相关关系(r=0.655,95%CI:0.564~0.731,P < 0.001)。行RN术后GFR和NB-GFR之间的相关系数为中等强度(r=0.419,95%CI:0.334~0.497,P < 0.001)。而采用Spearman相关评价术后GFR和NB-GFR的关系,行RN术后GFR和NB-GFR存在较强的正相关关系(r=0.586,95%CI:0.516~0.649,P < 0.001);行PN术后GFR和NB-GFR存在较强的正相关关系(r=0.606,95%CI:0.503~0.692,P < 0.001)。采用受试者工作特征(receiver operating characteristic,ROC)曲线对总的术后GFR与NB-GFR进行吻合度检验,可知术后GFR与NB-GFR吻合度较高。组内相关性检验可得术后GFR与NB-GFR间相关性的值为0.508(P < 0.001)。结论 NB-GFR的预测方程预测中国南方人群行RN或PN的NB-GFR与实际术后GFR吻合度较高,有十分广泛的应用前景;且在行PN患者中应用该预测方程较行RN的患者更为准确,更值得在临床上推广应用。Abstract: Objective To test the ability of a new baseline assessment model for renal function after radical nephrectomy (RN) or partial nephrectomy (PN) to evaluate renal function and assess its applicability to the Chinese population.Methods A retrospective of 398 cases of RN patients and 185 cases of PN patients in the First Affiliated Hospital of Guangxi Medical University from 2015 to 2022 was performed, and the correlation analysis between the postoperative new baseline glomerular filtration rate(NB-GFR) predicted by the formula and the actual GFR of the patients was carried out, and the degree of agreement was tested.Results First of all, the general information and clinical data of the two groups of patients were tested, and the results showed no significant difference. Pearson correlation was used to evaluate the relationship between postoperative GFR and NB-GFR. There was a strong positive correlation between GFR and NB-GFR after PN, with correlation coefficient r=0.655, 95%CI: 0.564-0.731, P < 0.001. The correlation coefficient between GFR and NB-GFR after RN was moderate, with correlation coefficient r=0.419, 95%CI: 0.334-0.497, P < 0.001. The Spearman correlation was used to evaluate the relationship between postoperative GFR and NB-GFR. There was a strong positive correlation between GFR and NB-GFR after RN, the correlation coefficient was r=0.586, 95%CI: 0.516-0.649, P < 0.001. There was a strong positive correlation between GFR and NB-GFR after PN, r=0.606, 95%CI: 0.503-0.692, P < 0.001. ROC was used to test the agreement between the total postoperative GFR and NB-GFR. The intra-group correlation test showed that the correlation value between postoperative GFR and NB-GFR was 0.508, P < 0.001.Conclusion The prediction equation of NB-GFR predicts that the NB-GFR of RN or PN in southern Chinese population is in good agreement with the actual postoperative GFR, and has a very broad application prospect. The application of this prediction equation in patients with PN is better than that in patients with RN, so it is more accurate and more worthy of clinical promotion.
-

-
表 1 2组基线资料比较
例(%),X±S,M(P25,P75) 基线资料 RN组(398例) PN组(185例) t/U/χ2 P值 年龄/岁 53.82±12.29 50.65±12.67 2.875 0.004 性别 0.021 0.885 男 273(68.60) 128(69.20) 女 125(31.40) 57(30.80) 民族 0.214 0.898 汉族 270(67.80) 127(68.60) 壮族 112(28.10) 52(28.10) 其他 16(4.00) 6(3.20) 糖尿病 0.473 0.492 是 37(9.30) 14(7.60) 否 361(90.70) 171(92.40) 肿瘤直径>7 cm 54.387 < 0.001 是 117(29.40) 5(2.70) 否 281(70.60) 180(97.30) 身高/cm 165.00(160.00, 170.00) 165.00(159.25, 170.00) -0.181 0.856 体重/kg 63.00(55.00, 72.00) 64.00(56.00, 73.00) -1.140 0.254 BMI 23.44(21.23, 25.51) 23.89(21.49, 26.16) -1.482 0.138 术前血清肌酐/(μmol/L) 83.00(68.00, 100.00) 78.00(66.00, 94.00) -2.179 0.029 术后3~12个月内血清肌酐/(μmol/L) 109.00(88.00, 128.00) 87.00(71.50,106.50) -7.233 < 0.001 术前GFR/[mL/(min·1.73 m2)] 41.95(34.76, 49.78) 45.94(38.13, 52.35) -3.361 0.001 术后GFR/[mL/(min·1.73 m2)] 30.60(25.68, 35.84) 40.07(32.90, 46.28) -9.135 < 0.001 NB-GFR/[mL/(min·1.73 m2)] 31.14(25.09, 36.89) 52.45(45.64, 58.1) -16.490 < 0.001 表 2 术后GFR与NB-GFR吻合度检验
指标 AUC 灵敏度 特异度 约登指数 P值 术后GFR 0.735 0.659 0.744 0.403 < 0.001 NB-GFR 0.924 0.908 0.824 0.732 < 0.001 -
[1] Siegel R, DeSantis C, Virgo K, et al. Cancer treatment and survivorship statistics, 2012[J]. CA Cancer J Clin, 2012, 62(4): 220-241. doi: 10.3322/caac.21149
[2] Pierorazio PM, Johnson MH, Patel HD, et al. Management of renal masses and localized renal cancer: systematic review and meta-analysis[J]. J Urol, 2016, 196(4): 989-999. doi: 10.1016/j.juro.2016.04.081
[3] Lane BR, Demirjian S, Derweesh IH, et al. Survival and functional stability in chronic kidney disease due to surgical removal of nephrons: importance of the new baseline glomerular filtration rate[J]. Eur Urol, 2015, 68(6): 996-1003. doi: 10.1016/j.eururo.2015.04.043
[4] Wu JT, Suk-Ouichai C, Dong W, et al. Analysis of survival for patients with chronic kidney disease primarily related to renal cancer surgery[J]. BJU Int, 2018, 121(1): 93-100. doi: 10.1111/bju.13994
[5] Ljungberg B, Albiges L, Abu-Ghanem Y, et al. European association of urology guidelines on renal cell carcinoma: the 2019 update[J]. Eur Urol, 2019, 75(5): 799-810. doi: 10.1016/j.eururo.2019.02.011
[6] Campbell S, Uzzo RG, Allaf ME, et al. Renal mass and localized renal cancer: AUA guideline[J]. J Urol, 2017, 198(3): 520-529. doi: 10.1016/j.juro.2017.04.100
[7] Sorbellini M, Kattan MW, Snyder ME, et al. Prognostic nomogram for renal insufficiency after radical or partial nephrectomy[J]. J Urol, 2006, 176(2): 472-476. doi: 10.1016/j.juro.2006.03.090
[8] Kim HL, Shah SK, Tan W, et al. Estimation and prediction of renal function in patients with renal tumor[J]. J Urol, 2009, 181(6): 2451-2461. doi: 10.1016/j.juro.2009.01.112
[9] Liss MA, DeConde R, Caovan D, et al. Parenchymal volumetric assessment as a predictive tool to determine renal function benefit of nephron-sparing surgery compared with radical nephrectomy[J]. J Endourol, 2016, 30(1): 114-121. doi: 10.1089/end.2015.0411
[10] Shum CF, Bahler CD, Cary C, et al. Preoperative nomograms for predicting renal function at 1 year after partial nephrectomy[J]. J Endourol, 2017, 31(7): 711-718. doi: 10.1089/end.2017.0184
[11] Martini A, Cumarasamy S, Beksac AT, et al. A nomogram to predict significant estimated glomerular filtration rate reduction after robotic partial nephrectomy[J]. Eur Urol, 2018, 74(6): 833-839. doi: 10.1016/j.eururo.2018.08.037
[12] Bertolo R, Garisto J, Li JB, et al. Development and internal validation of a nomogram for predicting renal function after partial nephrectomy[J]. Eur Urol Oncol, 2019, 2(1): 106-109. doi: 10.1016/j.euo.2018.06.015
[13] Bhindi B, Lohse CM, Schulte PJ, et al. Predicting renal function outcomes after partial and radical nephrectomy[J]. Eur Urol, 2019, 75(5): 766-772. doi: 10.1016/j.eururo.2018.11.021
[14] McIntosh AG, Parker DC, Egleston BL, et al. Prediction of significant estimated glomerular filtration rate decline after renal unit removal to aid in the clinical choice between radical and partial nephrectomy in patients with a renal mass and normal renal function[J]. BJU Int, 2019, 124(6): 999-1005. doi: 10.1111/bju.14839
[15] Aguilar Palacios D, Caraballo ER, Tanaka H, et al. Compensatory changes in parenchymal mass and function after radical nephrectomy[J]. J Urol, 2020, 204(1): 42-49. doi: 10.1097/JU.0000000000000797
[16] Mir MC, Ercole C, Takagi T, et al. Decline in renal function after partial nephrectomy: etiology and prevention[J]. J Urol, 2015, 193(6): 1889-1898. doi: 10.1016/j.juro.2015.01.093
[17] Simmons MN, Hillyer SP, Lee BH, et al. Functional recovery after partial nephrectomy: effects of volume loss and ischemic injury[J]. J Urol, 2012, 187(5): 1667-1673. doi: 10.1016/j.juro.2011.12.068
[18] Tanaka H, Wang YB, Suk-Ouichai C, et al. Can we predict functional outcomes after partial nephrectomy?[J]. J Urol, 2019, 201(4): 693-701. doi: 10.1016/j.juro.2018.09.055
[19] Funahashi Y, Hattori R, Yamamoto T, et al. Relationship between renal parenchymal volume and single kidney glomerular filtration rate before and after unilateral nephrectomy[J]. Urology, 2011, 77(6): 1404-1408. doi: 10.1016/j.urology.2010.03.063
[20] Aguilar Palacios D, Wilson B, Ascha M, et al. New baseline renal function after radical or partial nephrectomy: a simple and accurate predictive model[J]. J Urol, 2021, 205(5): 1310-1320. doi: 10.1097/JU.0000000000001549
[21] 全国eGFR课题协作组. MDRD方程在我国慢性肾脏病患者中的改良和评估[J]. 中华肾脏病杂志, 2006(10): 589-595. doi: 10.3760/j.issn:1001-7097.2006.10.002
[22] Tachibana H, Omae K, Ishihara H, et al. Validation of a predictive model for new baseline renal function after radical nephrectomy or robot-assisted partial nephrectomy in Japanese patients[J]. J Endourol, 2022, 36(6): 745-751. doi: 10.1089/end.2021.0655
-




 下载:
下载: