Analysis of urodynamic characteristics of IC/BPS women with or without Hunner's lesion
-
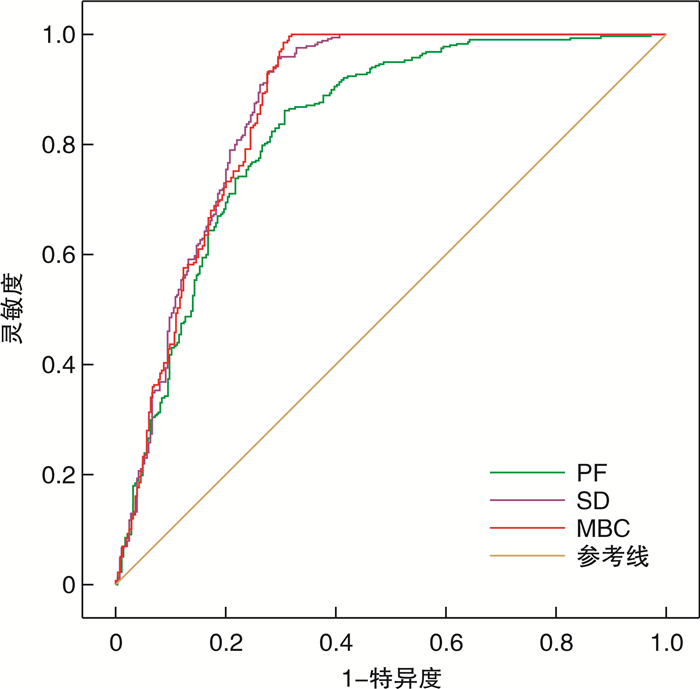
摘要: 目的 根据间质性膀胱炎伴或不伴Hunner病变的分型,探讨间质性膀胱炎/膀胱疼痛综合征(interstitial cystitis/bladder pain syndrome,IC/BPS)女性患者客观尿动力学参数差异。方法 回顾性分析2013年1月—2020年12月南京医科大学第二附属医院接受膀胱水扩张和尿动力学检查的604例IC/BPS的女性患者临床资料。IC/BPS患者根据美国泌尿外科指南标准行膀胱水扩张,根据膀胱镜检查中Hunner病变是否存在,将患者分为Hunner病变组和非Hunner病变组。比较2组患者平均排尿次数、平均排尿量、疼痛视觉模拟量表评分(VAS)、O'Leary-Saint症状评分和尿动力学检查客观指标,对患者的临床症状进行评估。比较2组患者的基线参数和尿动力学检查参数。结果 604例IC/BPS女性患者中,286例(47.35%)IC/BPS患者在麻醉状态下行膀胱水扩张检查中出现Hunner病变。排尿日记提示,Hunner组IC/BPS患者平均排尿次数较非Hunner组患者更频繁,且平均排尿量明显减少,差异有统计学意义(P < 0.05)。尿动力学检查客观指标提示,Hunner组的初始排尿感、正常排尿感、出现不适膀胱容量、强烈排尿感和最大膀胱容量均显著低于非Hunner组(P < 0.05)。ROC曲线结果提示,尿动力学结果中出现不适膀胱容量≤141 mL[曲线下面积(AUC)=0.827,P < 0.001]、强烈尿意≤200 mL(AUC=0.867,P < 0.001)和最大膀胱容量≤215 mL(AUC=0.867,P < 0.001)对诊断存在Hunner病变的IC/BPS患者更有意义。结论 伴或不伴Hunner病变的IC/BPS患者,其主观症状的差异和尿动力学客观指标的差异相一致。Abstract: Objective To investigate the differences of objective urodynamic parameters in female patients with interstitial cystitis/bladder pain syndrome (IC/BPS) according to the classification of interstitial cystitis with or without Hunner's disease.Methods The clinical data of 604 female patients with IC/BPS who received treatment from January 2013 to December 2020 in the Second Affiliated Hospital of Nanjing Medical University were retrospectively analyzed. The patients with IC/BPS underwent bladder hydrodistention according to the American urological guidelines. According to the presence of Hunner's lesions in cystoscopy, the patients were divided into Hunner's lesion group and non-Hunner's lesion group. The average urination frequency, average urination volume, visual analogue scale (VAS), O'Leary-Sant symptom score and objective indicators of urodynamic examination were compared between the two groups to evaluate the clinical symptoms of the patients. Baseline parameters and urodynamic parameters were compared between the two groups.Results Among the 604 IC/BPS female patients, 286 (47.35%) IC/BPS patients had Hunner lesions during the examination of bladder hydrodistention under anesthesia. In terms of urination diary response, the average urination frequency of IC/BPS patients in Hunner lesion group was more frequent than that of non-Hunner lesion group IC/BPS patients, and the average urination volume was significantly decreased. The difference was statistically significant (P < 0.05). The objective indicators of urodynamic examination indicated that the initial urge to urinate, normal urge to urinate, strong urge to urinate, maximum bladder capacity and pain with filling in the Hunner lesion group were significantly lower than those in the non-Hunner lesion group (P < 0.05). The results of the ROC curve indicated that pain with filling ≤141 mL (area under the curve [AUC]=0.827, P < 0.001), strong urge to urinate ≤200 mL (AUC=0.867, P < 0.001) and maximum bladder capacity ≤215 mL (AUC=0.867, P < 0.001) were significantly important for the diagnosis of IC/BPS patients with Hunner lesion.Conclusion The differences in subjective symptoms and objective urodynamic parameters are consistent in IC/BPS patients with or without Hunner's lesions.
-
Key words:
- interstitial cystitis /
- urodynamic test /
- Hunner's disease /
- bladder hydrodistention
-

-
表 1 2组患者基线资料比较
M(P25,P75) 项目 Hunner病变组(286例) 非Hunner病变组(318例) 平均排尿量/mL 50(39,80)1) 90(70,120) 平均排尿次数/次 32(24,42)1) 23(18,29) VAS评分/分 8(7,10) 8(6,9) O'Leary-Sant评分/分 30(27,32) 29(26,31) 与非Hunner病变组比较,1) P < 0.05。 表 2 2组患者尿动力学指标比较
M(P25,P75) 指标 Hunner病变组(286例) 非Hunner病变组(318例) 尿流率指标 Qmax/(mL/s) 11.25
(7.03,17.08)12.2
(7.2,18.5)VV/mL 127.25
(88,168.83)1)130
(88.03,178.75)PVR/mL 21(8,34) 23(14,27) 充盈期膀胱压力容积测定 FD/mL 55.15
(32.85,78.32)1)79.10
(63.20,94.80)ND/mL 92.45
(62.72,123.9)1)133.30
(109.40,162.45)SD/mL 151.4
(109.13,213.78)1)263.2
(229.08,301.85)PF/mL 113.25
(81.9,152.65)1)181.60
(154.40,208.08)MBC/mL 167.40
(116.53,243.43)1)292.05
(253.03,329.5)DO/例(%) 186(65.03) 158(49.69) 排尿期压力-流率测定 Pdet Qmax/cmH2O 30.5(20,45) 31.0(19,46) 注:1 cmH2O=0.098 kPa;与非Hunner病变组比较,1) P < 0.05。 表 3 PF、SD、MBC的ROC曲线参数分析
参数 PF SD MBC AUC 0.827 0.867 0.867 P值 < 0.001 < 0.001 < 0.001 95% CI 0.793~0.861 0.837~0.898 0.836~0.898 截断值/mL 141 200 215 灵敏度/% 86.2 95.6 99.7 特异度/% 69.2 70.6 68.5 PPV/% 81.9 93.5 98.5 NPV/% 75.1 77.9 77.8 -
[1] Homma Y, Akiyama Y, Tomoe H, et al. Clinical guidelines for interstitial cystitis/bladder pain syndrome[J]. Int J Urol, 2020, 27(7): 578-589. doi: 10.1111/iju.14234
[2] Lai HH, Pickersgill NA, Vetter JM. Hunner lesion phenotype in interstitial cystitis/bladder pain syndrome: a systematic review and meta-analysis[J]. J Urol, 2020, 204(3): 518-523. doi: 10.1097/JU.0000000000001031
[3] Kim A, Hoe KO, Shin JH, et al. Evaluation of the incidence and risk factors associated with persistent frequency in interstitial cystitis/bladder pain syndrome and the efficacy of antimuscarinic treatment[J]. Investig Clin Urol, 2017, 58(5): 353-358. doi: 10.4111/icu.2017.58.5.353
[4] Lai HH, Thu J, Moh FV, et al. Clustering of patients with interstitial cystitis/bladder pain syndrome and chronic prostatitis/chronic pelvic pain syndrome[J]. J Urol, 2019, 202(3): 546-551. doi: 10.1097/JU.0000000000000250
[5] Yeh HL, Jhang JF, Kuo YC, et al. Long-term outcome and symptom improvement in patients with interstitial cystitis/bladder pain syndrome with or without regular follow-up and treatment[J]. Neurourol Urodyn, 2019, 38(7): 1985-1993. doi: 10.1002/nau.24104
[6] Schäfer W, Abrams P, Liao L, et al. Good urodynamic practices: uroflowmetry, filling cystometry, and pressure-flow studies[J]. Neurourol Urodyn, 2002, 21(3): 261-274. doi: 10.1002/nau.10066
[7] Hsu CC, Liang CC, Chang SD, et al. Comparison of urodynamic results and quality of life between women with interstitial cystitis and overactive bladder[J]. Taiwan J Obstet Gynecol, 2020, 59(1): 39-42. doi: 10.1016/j.tjog.2019.11.005
[8] Kuo YC, Kuo HC. Videourodynamic characteristics of interstitial cystitis/bladder pain syndrome-The role of bladder outlet dysfunction in the pathophysiology[J]. Neurourol Urodyn, 2018, 37(6): 1971-1977. doi: 10.1002/nau.23542
[9] Hanno PM, Burks DA, Clemens JQ, et al. AUA guideline for the diagnosis and treatment of interstitial cystitis/bladder pain syndrome[J]. J Urol, 2011, 185(6): 2162-2170. doi: 10.1016/j.juro.2011.03.064
[10] van de Merwe JP, Nordling J, Bouchelouche P, et al. Diagnostic criteria, classification, and nomenclature for painful bladder syndrome/interstitial cystitis: an ESSIC proposal[J]. Eur Urol, 2008, 53(1): 60-67. doi: 10.1016/j.eururo.2007.09.019
[11] Hogan S, Gammie A, Abrams P. Urodynamic features and artefacts[J]. NeurourolUrodyn, 2012, 31(7): 1104-1117.
[12] Nickel JC, Doiron RC. Hunner lesion interstitial cystitis: the bad, the good, and the unknown[J]. Eur Urol, 2020, 78(3): e122-e124. doi: 10.1016/j.eururo.2020.04.067
[13] Houbiers J, van Till J, Kaper M, et al. An adaptive randomized clinical trial in interstitial cystitis/bladder pain syndrome evaluating efficacy of ASP3652 and the relationship between disease characteristics and Hunner's lesions[J]. World J Urol, 2021, 39(6): 2065-2071. doi: 10.1007/s00345-020-03372-z
[14] Ko KJ, Cho WJ, Lee YS, et al. Comparison of the efficacy between transurethral coagulation and transurethral resection of Hunner lesion in interstitial cystitis/bladder pain syndrome patients: a prospective randomized controlled trial[J]. Eur Urol, 2020, 77(5): 644-651. doi: 10.1016/j.eururo.2020.01.002
[15] Mazeaud C, Rigaud J, Levesque A, et al. Stratification of patients with interstitial cystitis/bladder pain syndrome according to the anatomical bladder capacity[J]. Urology, 2019, 123: 87-92. doi: 10.1016/j.urology.2018.07.046
[16] Shin JH, Kang B, Choo MS. Features of various bladder lesions and their impact on clinical symptoms and recurrence in interstitial cystitis[J]. J Urol, 2021, 206(3): 669-678. doi: 10.1097/JU.0000000000001811
[17] Hanno PM, Erickson D, Moldwin R, et al. Diagnosis and treatment of interstitial cystitis/bladder pain syndrome: AUA guideline amendment[J]. J Urol, 2015, 193(5): 1545-1553. doi: 10.1016/j.juro.2015.01.086
[18] Sastry DN, Hunter KM, Whitmore KE. Urodynamic testing and interstitial cystitis/painful bladder syndrome[J]. Int Urogynecol J, 2010, 21(2): 157-161. doi: 10.1007/s00192-009-1015-6
[19] Cheng WM, Fan YH, Lin A. Urodynamic characteristics might be variable in bladder pain syndrome/interstitial cystitis patients with different non-bladder co-morbid conditions[J]. J Chin Med Assoc, 2018, 81(3): 248-254. doi: 10.1016/j.jcma.2017.06.022
-




 下载:
下载: