Clinical effect analysis and experience summary of laparoscopic resection of largetumors in adrenal and adrenal areas via abdominal route
-
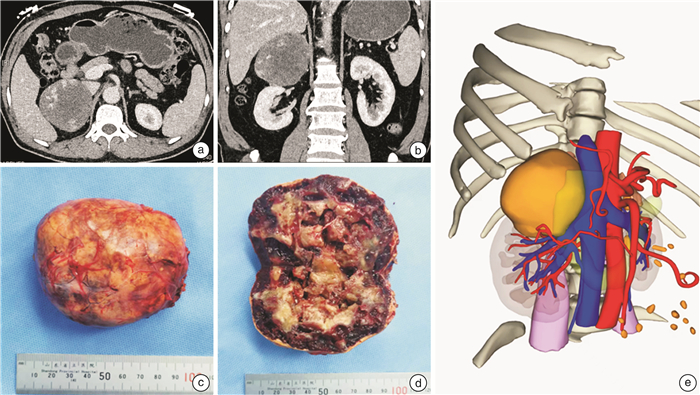
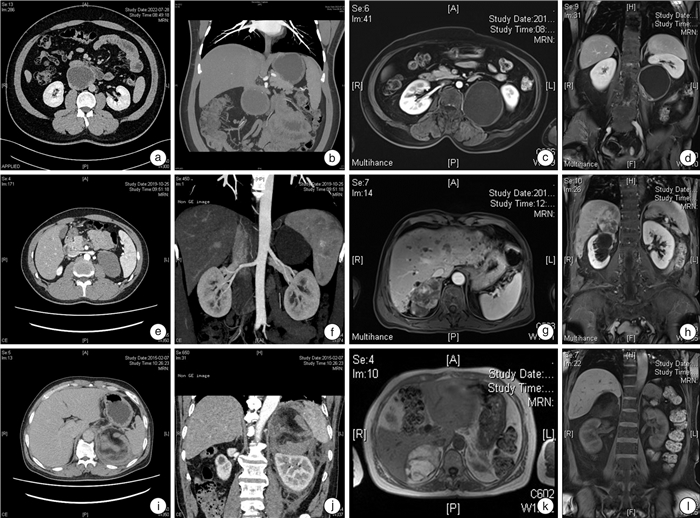
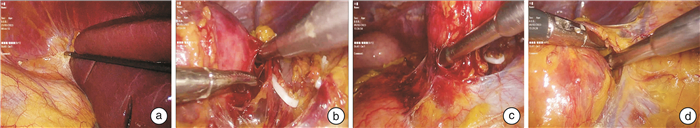
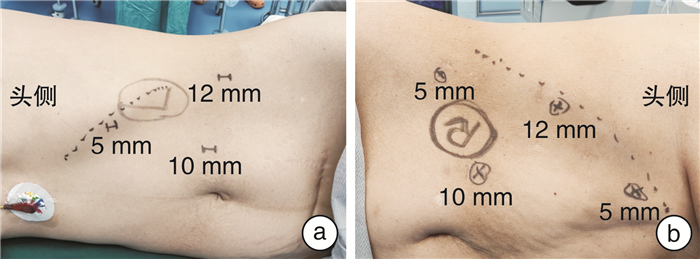
摘要: 目的 探讨经腹腔路径腹腔镜手术切除肾上腺及肾上腺区巨大肿瘤的手术经验、技巧及安全性。方法 回顾性分析2012年3月—2022年8月山东第一医科大学附属省立医院收治的行腹腔镜手术治疗的82例肾上腺及肾上腺区巨大肿瘤患者的临床资料,统计手术成功率、手术时间、术中出血量、输血量、术后引流量、术后拔管时间、术后住院时间、围手术期并发症等情况。结果 82例患者手术入路均为经腹腔,其中左侧52例、右侧30例;肾上腺病变66例,肾上腺区病变16例。82例患者中,81例手术成功,无中转开放手术,1例因肿瘤粘连严重,转为腹腔镜肿瘤活检+减瘤术。手术时间30~360 min,平均(95.68±57.51) min;术中出血量10~1 500 mL,平均(119.37±224.90) mL;输血6例,输去白悬浮红细胞2.00~5.75 U,平均(3.96±1.19) U。术后前3 d引流量0~594 mL,平均(101.35±115.00) mL;术后拔管时间3~20 d,平均(5.84±2.64) d;术后住院时间4~23 d,平均(8.04±2.94) d;术后患者均未发生严重的围手术期并发症。结论 对于经验丰富的外科医生,经腹腔路径腹腔镜手术切除肾上腺及肾上腺区巨大肿瘤是安全可行的。Abstract: Objective To explore the surgical experience, operation technique and safety of laparoscopic resection of large tumors in adrenal and adrenal areas via abdominal approach.Methods A retrospective analysis was made of the clinical data of 82 patients with large adrenal or adrenal areas tumors who underwent laparoscopic surgery and were treated in Shandong Provincial Hospital Affiliated to Shandong First Medical University from March 2012 to August 2022. The achievement ratio of operation, operation time, intraoperative blood loss, blood transfusion volume, postoperative drainage volume, postoperative drainage tube extraction time, postoperative hospital stay, perioperative complications were counted.Results The surgical approach of 82 patients was via abdominal approach, including 52 cases on the left side, 30 cases on the right side, 66 cases of adrenal lesions, 16 cases of adrenal areas lesions. Among the 82 patients, 81 were successfully operated without conversion to open surgery. One patient underwent laparoscopic surgery and was converted to laparoscopic tumor biopsy plus tumor reduction due to severe tumor adhesion. The operation time was 30-360 min, and the average time was (95.68±57.51) min. Intraoperative blood loss ranged from 10 to 1 500 mL with an average of (119.37±224.90) mL. Six patients were transfused with red blood cells from 2.00 to 5.75 U, with an average of (3.96±1.19) U. In the first 3 days after surgery, the drainage volume was 0-594 mL, with an average of (101.35±115.00) mL. The postoperative extubation time was 3-20 days, with an average of (5.84±2.64) days. The postoperative hospital stay was 4-23 days, with an average of (8.04±2.94) days. No serious perioperative complications occurred in the patients.Conclusion For experienced surgeons, laparoscopic resection of large adrenal or adrenal areas tumors via abdominal approach is safe and feasible.
-

-
[1] Bittner JG 4th, Gershuni VM, Matthews BD, et al. Risk factors affecting operative approach, conversion, and morbidity for adrenalectomy: a single-institution series of 402 patients[J]. Surg Endosc, 2013, 27(7): 2342-2350. doi: 10.1007/s00464-013-2789-7
[2] Gagner M, Lacroix A, Bolté E. Laparoscopic adrenalectomy in Cushing's syndrome and pheochromocytoma[J]. N Engl J Med, 1992, 327(14): 1033. doi: 10.1056/NEJM199210013271417
[3] Rosoff JS, Raman JD, Del Pizzo JJ. Laparoscopic adrenalectomy for large adrenal masses[J]. Curr Urol Rep, 2008, 9(1): 73-79. doi: 10.1007/s11934-008-0014-3
[4] Autorino R, Bove P, De Sio M, et al. Open Versus Laparoscopic Adrenalectomy for Adrenocortical Carcinoma: A Meta-analysis of Surgical and Oncological Outcomes[J]. Ann Surg Oncol, 2016, 23(4): 1195-1202. doi: 10.1245/s10434-015-4900-x
[5] Hobart MG, Gill IS, Schweizer D, et al. Laparoscopic adrenalectomy for large-volume(>or=5 cm)adrenal masses[J]. J Endourol, 2000, 14(2): 149-154. doi: 10.1089/end.2000.14.149
[6] Shonkwiler RJ, Lee JA. Laparoscopic retroperitoneal adrenalectomy[J]. Surg Laparosc Endosc Percutan Tech, 2011, 21(4): 243-247. doi: 10.1097/SLE.0b013e3182266a86
[7] Raffaelli M, De Crea C, Bellantone R. Laparoscopic adrenalectomy[J]. Gland Surg, 2019, 8(Suppl 1): S41-S52.
[8] Yip L, Duh QY, Wachtel H, et al. American Association of Endocrine Surgeons Guidelines for Adrenalectomy: Executive Summary[J]. JAMA surgery, 2022, 157(10): 870-877. doi: 10.1001/jamasurg.2022.3544
[9] Dalvi AN, Thapar PM, Thapar VB, et al. Laparoscopic adrenalectomy for large tumours: Single team experience[J]. J Minim Access Surg, 2012, 8(4): 125-128. doi: 10.4103/0972-9941.103110
[10] Elfenbein DM, Scarborough JE, Speicher PJ, et al. Comparison of laparoscopic versus open adrenalectomy: results from American College of Surgeons-National Surgery Quality Improvement Project[J]. J Surg Res, 2013, 184(1): 216-220. doi: 10.1016/j.jss.2013.04.014
[11] Hemal AK, Singh A, Gupta NP. Whether adrenal mass more than 5 cm can pose problem in laparoscopic adrenalectomy? An evaluation of 22 patients[J]. World J Urol, 2008, 26(5): 505-508. doi: 10.1007/s00345-008-0270-3
[12] Bozkurt IH, Arslan M, Yonguc T, et al. Laparoscopic adrenalectomy for large adrenal masses: Is it really more complicated?[J]. Kaohsiung J Med Sci, 2015, 31(12): 644-648. doi: 10.1016/j.kjms.2015.09.005
[13] Gan L, Peng L, Li J, et al. Comparison of the effectiveness and safety of robotic-assisted and laparoscopic in adrenalectomy: A systematic review and meta-analysis[J]. Int J Surg, 2022, 105: 106853. doi: 10.1016/j.ijsu.2022.106853
[14] Virseda Rodríguez JA, Donate Moreno MJ, Pastor Navarro H, et al. Primary retroperitoneal tumors: review of our 10-year case series[J]. Arch Esp Urol, 2010, 63(1): 13-22.
[15] Jain A, Baracco R, Kapur G. Pheochromocytoma and paraganglioma-an update on diagnosis, evaluation, and management[J]. Pediatr Nephrol, 2020, 35(4): 581-594. doi: 10.1007/s00467-018-4181-2
[16] Wang X, Zhao Y, Liao Z, et al. Surgical strategies of complicated pheochromocytomas/paragangliomas and literature review[J]. Front Endocrinol(Lausanne), 2023, 14: 1129622. doi: 10.3389/fendo.2023.1129622
[17] Ji XK, Zheng XW, Wu XL, et al. Diagnosis and surgical treatment of retroperitoneal paraganglioma: A single-institution experience of 34 cases[J]. Oncol Lett, 2017, 14(2): 2268-2280. doi: 10.3892/ol.2017.6468
[18] Menegaux F, Chéreau N, Peix JL, et al. Management of adrenal incidentaloma[J]. J Visc Surg, 2014, 151(5): 355-364. doi: 10.1016/j.jviscsurg.2014.07.002
[19] Hallin Thompson L, Makay Ö, Brunaud L, et al. Adrenalectomy for incidental and symptomatic phaeochromocytoma: retrospective multicentre study based on the Eurocrine® database[J]. Br J Surg, 2021, 108(10): 1199-1206. doi: 10.1093/bjs/znab199
[20] Fernandes-Rosa FL, Boulkroun S, Fedlaoui B, et al. New advances in endocrine hypertension: from genes to biomarkers[J]. Kidney Int, 2023, 103(3): 485-500. doi: 10.1016/j.kint.2022.12.021
[21] Chai YJ, Kwon H, Yu HW, et al. Systematic Review of Surgical Approaches for Adrenal Tumors: Lateral Transperitoneal versus Posterior Retroperitoneal and Laparoscopic versus Robotic Adrenalectomy[J]. Int J Endocrinol, 2014, 2014: 918346.
[22] 李磊, 唐世英, 刘茁, 等. 全肝游离技术在肾癌伴下腔静脉癌栓手术中的应用价值[J]. 中华泌尿外科杂志, 2021, 42(8): 566-570.
[23] 张大宏, 刘锋, 毛祖杰. 巨大肾上腺肿瘤腹腔镜手术(附光盘)[J]. 现代泌尿外科杂志, 2014, 19(10): 633-635. https://www.cnki.com.cn/Article/CJFDTOTAL-MNWK201410004.htm
[24] Zhang X, Lang B, Ouyang JZ, et al. Retroperitoneoscopic adrenalectomy without previous control of adrenal vein is feasible and safe for pheochromocytoma[J]. Urology, 2007, 69(5): 849-853. doi: 10.1016/j.urology.2007.01.078
[25] Perry KA, El Youssef R, Pham TH, et al. Laparoscopic adrenalectomy for large unilateral pheochromocytoma: experience in a large academic medical center[J]. Surg Endosc, 2010, 24(6): 1462-1467. doi: 10.1007/s00464-009-0801-z
-




 下载:
下载: