Analysis of diagnosis and treatment of primary pigmented nodular adrenocortical disease
-
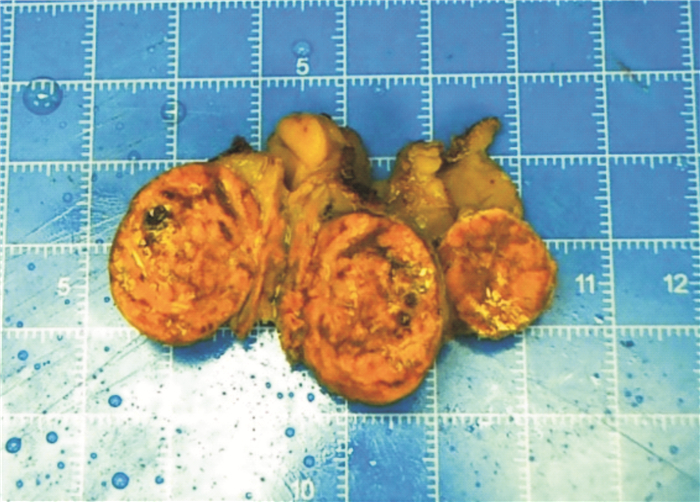
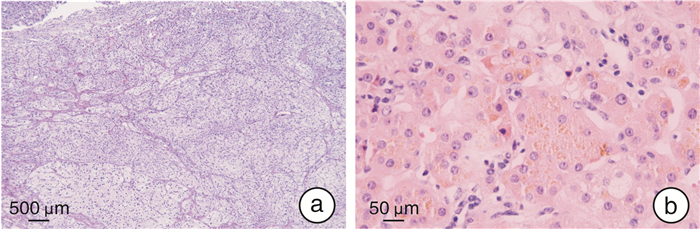
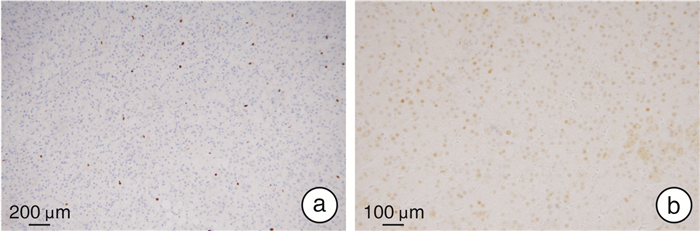
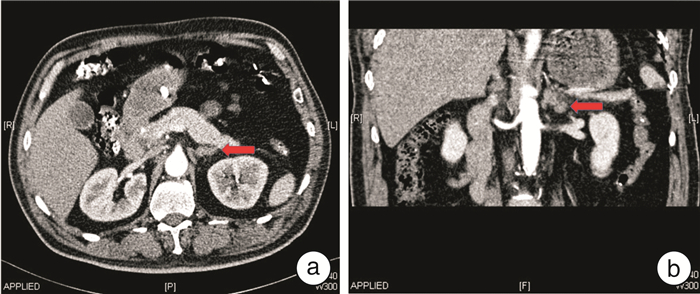
摘要: 目的 探讨原发性色素性结节状肾上腺皮质病(primary pigmented nodular adrenocortical disease,PPNAD)的临床特点和腹腔镜肾上腺切除术的疗效。方法 回顾性分析2011年12月—2021年4月福建省立医院收治的5例病理确诊为PPNAD的患者资料,包括临床表现、体征、实验室结果、影像学检查、手术及随访数据等。5例PPNAD的患者中,女2例,男3例,表现为经典库欣综合征(Cushing's syndrome,CS)2例,其余3例患者仅有高血压。2例有口唇皮肤色素沉着,符合卡尼综合征(Carney complex,CNC)表现。3例患者促肾上腺皮质激素(ACTH)偏低,2例正常。1例血浆皮质醇正常;4例血浆皮质醇升高,昼夜节律消失,其中1例小剂量地塞米松抑制试验(LDDST)后血浆皮质醇被抑制,另外3例大、小剂量地塞米松抑制试验均未被抑制。患者影像学表现为单侧肾上腺大结节增生、双侧肾上腺轻度增生或肾上腺未见明显占位性病变。1例患者入院后行腹腔镜下右侧肾上腺次全切术+左侧肾上腺全切术,4例入院后行腹腔镜下单侧肾上腺切除术。结果 5例患者术后送检病理均确诊为PPNAD,镜下均可观察到脂褐素沉积于胞质,免疫学组化提示该肿瘤的良性生物学行为。5例患者术后1周内血压明显下降,2例术后1周CS症状开始减退,随访1年后症状消失。1例术后随访第12年后再发CS,行腹腔镜下对侧肾上腺切除术后随访至今症状无复发。1例行腹腔镜下右侧肾上腺次全切术+左侧肾上腺全切术,术后2次因自行停用激素导致肾上腺皮质功能减退,出现低血压、头晕、四肢乏力等表现。其余患者术后恢复良好。结论 PPNAD可合并CNC。腹腔镜肾上腺切除术是PPNAD患者的有效治疗方法,可以实现CS的长期缓解。
-
关键词:
- 原发性色素性结节状肾上腺皮质病 /
- 腹腔镜肾上腺切除 /
- 库欣综合征 /
- 卡尼综合征
Abstract: Objective To investigate the clinical characteristics of the primary pigmented nodular adrenocortical disease(PPNAD) and the therapeutic effect of laparoscopic adrenalectomy.Methods Clinical data of five patients diagnosed with PPNAD in our center from December 2011 to April 2021 were collected for retrospective analysis, including clinical manifestations, signs, laboratory tests, imaging examinations, operation and follow-up data, etc.. There were two female and three male patients. Two cases showed classic Cushing's syndrome (CS), but only hypertension was established in the remaining three patients. Two cases had pigmentation of the skin on the face and lip, consistent with Carney complex (CNC). ACTH assay results were low in three patients and typical in two patients. Plasma cortisol was normal in one case, elevated in four cases, and disappeared in circadian rhythm. Plasma cortisol was suppressed in one case after LDDST, and the other three cases had the opposite results after DDST. Imaging studies showed unilateral adrenal hyperplasia, mild bilateral adrenal hyperplasia, or no obvious adrenal space-occupying lesions. One case underwent laparoscopic right subtotal adrenalectomy+left adrenalectomy. The other 4 cases underwent laparoscopic unilateral adrenalectomy after admission.Results Postoperative pathological diagnoses of all 5 patients were PPNAD, and lipofuscin deposition in the cytoplasm could be observed under the microscope. Immunohistochemistry suggested the benign biological behavior of the tumor. The blood pressure of 5 patients decreased significantly within 1 week after operation. The symptoms of CS in 2 cases began to subside in 1 week after operation, then the symptoms disappeared after 1 year of follow-up. One case developed CS after 12 years of postoperative follow-up. Laparoscopic contralateral adrenalectomy was performed and no symptoms have recurred so far. One case underwent laparoscopic right subtotal adrenalectomy+left adrenalectomy. Self-discontinuation of hormones twice after surgery resulted in adrenal hypofunction, hypotension, dizziness, and limb weakness. The remaining patients recovered well after the procedure.Conclusion PPNAD can be concurrent with CNC. Laparoscopic adrenalectomy is an effective treatment for patients with PPNAD. It can achieve long-term remission of CS. -

-
[1] Ammini AC, Tandon N, Gupta N, et al. Etiology and clinical profile of patients with Cushing's syndrome: A single center experience[J]. Indian J Endocrinol Metab, 2014, 18(1): 99-105. doi: 10.4103/2230-8210.126586
[2] Zhou J, Zhang M, Bai X, et al. Demographic Characteristics, Etiology, and Comorbidities of Patients with Cushing's Syndrome: A 10-Year Retrospective Study at a Large General Hospital in China[J]. Int J Endocrinol, 2019, 2019: 7159696.
[3] Groussin L, Kirschner LS, Vincent-Dejean C, et al. Molecular analysis of the cyclic AMP-dependent protein kinase A(PKA)regulatory subunit 1A(PRKAR1A)gene in patients with Carney complex and primary pigmented nodular adrenocortical disease(PPNAD)reveals novel mutations and clues for pathophysiology: augmented PKA signaling is associated with adrenal tumorigenesis in PPNAD[J]. Am J Hum Genet, 2002, 71(6): 1433-1442. doi: 10.1086/344579
[4] Stratakis CA, Carney JA, Lin JP, et al. Carney complex, a familial multiple neoplasia and lentiginosis syndrome. Analysis of 11 kindreds and linkage to the short arm of chromosome 2[J]. J Clin Invest, 1996, 97(3): 699-705. doi: 10.1172/JCI118467
[5] Stratakis CA, Kirschner LS, Carney JA. Clinical and molecular features of the Carney complex: diagnostic criteria and recommendations for patient evaluation[J]. J Clin Endocrinol Metab, 2001, 86(9): 4041-4046. doi: 10.1210/jcem.86.9.7903
[6] Dumontet T, Sahut-Barnola I, Septier A, et al. PKA signaling drives reticularis differentiation and sexually dimorphic adrenal cortex renewal[J]. JCI Insight, 2018, 3(2): e98394. doi: 10.1172/jci.insight.98394
[7] Young WF Jr, du Plessis H, Thompson GB, et al. The clinical conundrum of corticotropin-independent autonomous cortisol secretion in patients with bilateral adrenal masses[J]. World J Surg, 2008, 32(5): 856-862. doi: 10.1007/s00268-007-9332-8
[8] Maillet M, Bourdeau I, Lacroix A. Update on primary micronodular bilateral adrenocortical diseases[J]. Curr Opin Endocrinol Diabetes Obes, 2020, 27(3): 132-139. doi: 10.1097/MED.0000000000000538
[9] Powell AC, Stratakis CA, Patronas NJ, et al. Operative management of Cushing syndrome secondary to micronodular adrenal hyperplasia[J]. Surgery, 2008, 143(6): 750-758. doi: 10.1016/j.surg.2008.03.022
[10] Hahner S, Loeffler M, Bleicken B, et al. Epidemiology of adrenal crisis in chronic adrenal insufficiency: the need for new prevention strategies[J]. Eur J Endocrinol, 2010, 162(3): 597-602. doi: 10.1530/EJE-09-0884
[11] Ritzel K, Beuschlein F, Mickisch A, et al. Clinical review: Outcome of bilateral adrenalectomy in Cushing's syndrome: a systematic review[J]. J Clin Endocrinol Metab, 2013, 98(10): 3939-3948. doi: 10.1210/jc.2013-1470
[12] Xu Y, Rui W, Qi Y, et al. The role of unilateral adrenalectomy in corticotropin-independent bilateral adrenocortical hyperplasias[J]. World J Surg, 2013, 37(7): 1626-1632. doi: 10.1007/s00268-013-2059-9
[13] 冒永鑫, 马文明, 戴军, 等. 单侧肾上腺切除作为促肾上腺皮质激素非依赖性肾上腺大结节增生首选治疗方法的可行性分析[J]. 临床泌尿外科杂志, 2021, 36(3): 167-172. doi: 10.13201/j.issn.1001-1420.2021.03.001 http://lcmw.cbpt.cnki.net/WKC/WebPublication/paperDigest.aspx?paperID=809418aa-5495-41a8-b8c2-a15eac5244ea
[14] Cristante J, Chabre O. Unilateral adrenalectomy in primary bilateral macronodular hyperplasia-Science Direct[J]. Curr Opin Endocr Metab Res, 2019, 8(C): 88-95.
[15] Guanà R, Gesmundo R, Morino M, et al. Laparoscopic unilateral adrenalectomy in children for isolated primary pigmented nodular adrenocortical disease(PPNAD): case report and literature review[J]. Eur J Pediatr Surg, 2010, 20(4): 273-275. doi: 10.1055/s-0029-1243203
[16] Vezzosi D, Tenenbaum F, Cazabat L, et al. Hormonal, Radiological, NP-59 Scintigraphy, and Pathological Correlations in Patients With Cushing's Syndrome Due to Primary Pigmented Nodular Adrenocortical Disease(PPNAD)[J]. J Clin Endocrinol Metab, 2015, 100(11): 4332-4338. doi: 10.1210/jc.2015-2174
-




 下载:
下载: