Preliminary study on the value and safety of templated lymph node dissection in upper urinary tract urothelial carcinoma
-
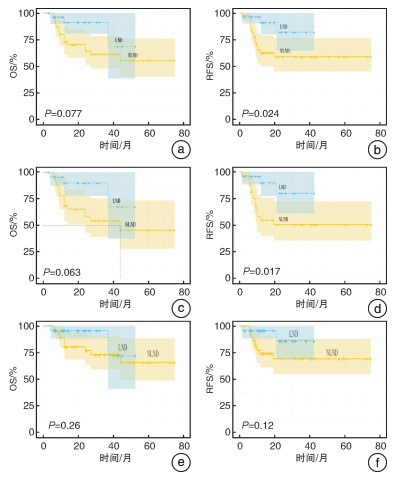
摘要: 目的 初步研究模板化淋巴结清扫术(lymph node dissection,LND)在上尿路尿路上皮癌(upper tract urothelial carcinoma,UTUC)中的价值及安全性。方法 回顾性分析我院2016年9月—2022年6月行腹腔镜下根治性肾输尿管切除术(laparoscopic radical nephroureterectomy,LRNU)且术后病理证实为UTUC患者的临床和随访资料,根据是否行LND,将患者分为LND组和NLND组,检验并比较2组患者的临床特征、总生存率及无复发生存率,分析肿瘤结局的影响因素。结果 2组患者在术中出血量、手术时长、住院费用及术后Ⅱ级并发症方面差异有统计学意义(P < 0.05);LND组的累积生存率(68.5% vs 55.1%,P=0.077)及无复发生存率(82.1% vs 58.9%,P=0.024)均高于NLND组;在≥pT2期患者中2组累积生存率及无复发生存率分别为67.5% vs 45.4%(P=0.063)和79.9% vs 50.4%(P=0.017);在cN0期患者中,2组累积生存率及无复发生存率分别为71.9% vs 65.6%(P=0.26)和86.3% vs 69.2%(P=0.12)。术后挽救性治疗(HR=0.31,95%CI:0.11~0.86,P=0.024)是改善生存结局的独立保护性因素。结论 UTUC患者,尤其是≥pT2期患者,可能从模板化LND中获益,同时,模板化LND的部分手术相关指标也可能稍逊色于NLND,但总体安全。Abstract: Objective To study the value and safety of templated lymph node dissection(LND) in upper urinary tract urothelial carcinoma(UTUC).Methods Clinical and follow-up data of patients who underwent laparoscopic radical nephroureterectomy(LRNU) and were pathologically confirmed as UTUC in our hospital from September 2016 to June 2022 were retrospectively collected. The patients were divided into LND group and NLND group, and the clinical characteristics, overall survival rate and recurrence-free survival rate of the two groups were examined and compared. The influencing factors of tumor outcome were analyzed.Results There were statistical differences in intraoperative blood loss, operation duration, hospitalization costs and postoperative Ⅱ complications between the two groups(P < 0.05). The cumulative and relapse-free survival rates in the LND group were 68.5% vs 55.1%(P=0.077) and 82.1% vs 58.9%(P=0.024) in all patients compared with the NLND group. In patients with ≥pT2, 67.5% vs 45.4%(P=0.063) and 79.9% vs 50.4%(P=0.017) were found, while in cN0 patients, 71.9% vs 65.6%(P=0.26) and 86.3% vs 69.2%(P=0.12) were found respectively. Postoperative salvage therapy(HR=0.31, 95%CI: 0.11-0.86, P=0.024) was an independent protective factor for improved survival outcomes.Conclusion Templated LND is basically safe for patients with UTUC especially those with ≥pT2, so these patients may benefit from it. However, some operation-related indicators of templated LND may be slightly lower than those of NLND.
-

-
表 1 2组患者的临床及随访资料
例,M(Q1,Q3) 项目 LND组(29例) NLND组(45例) χ2/Z P值 性别 0.76 0.383 男 18 22 女 11 23 年龄/岁 64.00(60.00, 67.00) 68.00(62.00, 73.00) 1.40 0.163 ECOG(体力状况评分) — 0.311 0 17 18 1 9 20 2 3 7 侧别 0 1 左 15 22 右 14 23 肿瘤位置 0.10 0.754 肾盂 18 25 输尿管 11 20 危险度分级 0.09 0.758 低危 6 12 高危 23 33 cN分期 <0.001 1 cN0 24 37 cN+ 5 8 术中出血量/mL 150.00(100.00, 200.00) 100.00(50.00, 100.00) -3.36 0.001 手术时间/min 305.00(270.00, 380.00) 235.00(190.00, 286.00) -3.74 < 0.001 术后并发症Clavie分级 — 0.042 0~1 22 42 2 7 3 术后住院时间/d 8.00(7.00, 13.00) 8.00(7.00, 10.00) -1.17 0.242 住院费用/元 35 017.38(31 146.18, 43 445.49) 28 946.73(25 082.60, 36 052.19) -2.97 0.003 病理分级 0 1 低级别 13 19 高级别 16 26 pT分期 0.74 0.388 pTis~pT1 5 13 pT2~pT4 24 32 pN分期 58.89 <0.001 pN0 20 0 pNx 0 39 pN+ 9 6 挽救性治疗 0 1 是 8 12 否 21 33 IVR 0.09 0.758 是 6 12 否 23 33 肿瘤复发 0.63 0.426 是 10 21 否 19 24 肿瘤性死亡 5.41 0.020 是 3 17 否 26 28 随访时间/月 16.00(10.00, 26.00) 24.00(12.00, 42.00) 1.78 0.074 表 2 影响患者术后生存的单因素和多因素Cox回归模型分析结果
因素 单因素分析 多因素分析 HR(95%CI) P值 HR(95%CI) P值 病理分级 低级别a)/高级别 3.88(1.13~13.29) 0.031 4.97(0.98~25.12) 0.053 肿瘤T分期 pTis~pT1a)/pT2~pT4 2.70(0.63~11.67) 0.183 肿瘤N分期 pN0a)/pNx、pN+ 0.29(0.07~1.26) 0.098 0.63(0.05~7.36) 0.712 LND/NLNDa) 0.35(0.10~1.19) 0.091 0.62(0.07~5.23) 0.66 挽救性治疗 有/无a) 0.27(0.11~0.65) 0.004 0.31(0.11~0.86) 0.024 注:a)表示参照组。 表 3 UTUC患者LNM位置分布情况
原发肿瘤位置 LNM部位 左肾盂(3例) 左RH-LN 6/8、IAC-LN 1/11、
PA-LN 0/2右肾盂(4例) 右RH-LN 7/16、PC-LN 5/12、
PA-LN 1/3左输尿管上段(1例) 左RH-LN 2/2 左输尿管下段(1例) 左II-LN及Ob-LN 1/17,
左EI-LN 0/7注:RH为肾门;PC为腔静脉旁;IAC为腔静脉主动脉间;PA为主动脉旁;II为髂内;EI为髂外;Ob为闭孔。 -
[1] 中国医师协会泌尿外科医师分会肿瘤专业委员会, 中国医师协会泌尿外科医师分会上尿路尿路上皮癌(CUDA-UTUC)协作组. 上尿路尿路上皮癌诊断与治疗中国专家共识[J]. 中华泌尿外科杂志, 2018, 39(7): 485-488. doi: 10.3760/cma.j.issn.1000-6702.2018.07.002
[2] Moschini M, Foerster B, Abufaraj M, et al. Trends of lymphadenectomy in upper tract urothelial carcinoma(UTUC)patients treated with radical nephroureterectomy[J]. World J Urol, 2017, 35(10): 1541-1547. doi: 10.1007/s00345-017-2026-4
[3] 白航, 单祖卷, 余闫宏, 等. 上尿路尿路上皮癌腹腔镜下基于模板的淋巴结清扫术的价值初探(附52例报道)[J]. 现代泌尿生殖肿瘤杂志, 2022, 14(4): 213-218.
[4] Kondo T, Takagi T, Tanabe K. Therapeutic role of template-based lymphadenectomy in urothelial carcinoma of the upper urinary tract[J]. World J Clin Oncol, 2015, 6(6): 237-251. doi: 10.5306/wjco.v6.i6.237
[5] Nazzani S, Mazzone E, Preisser F, et al. Rates of lymph node invasion and their impact on cancer specific mortality in upper urinary tract urothelial carcinoma[J]. Eur J Surg Oncol, 2019, 45(7): 1238-1245. doi: 10.1016/j.ejso.2018.12.004
[6] Huang JW, Qian HY, Yuan YC, et al. Prospective clinical trial of the oncologic outcomes and safety of extraperitoneal laparoscopic extended retroperitoneal lymph node dissection at time of nephroureterectomy for upper tract urothelial carcinoma[J]. Front Oncol, 2022, 12: 791140. doi: 10.3389/fonc.2022.791140
[7] Lughezzani G, Jeldres C, Isbarn H, et al. Nephroureterectomy and segmental ureterectomy in the treatment of invasive upper tract urothelial carcinoma: a population-based study of 2299 patients[J]. Eur J Cancer, 2009, 45(18): 3291-3297. doi: 10.1016/j.ejca.2009.06.016
[8] Choo MS, Yoo S, Yuk HD, et al. Survival benefits based on the number of lymph nodes removed during radical nephroureterectomy for upper tract urothelial carcinoma: systematic review and meta-analysis[J]. J Clin Med, 2020, 9(6): 1933. doi: 10.3390/jcm9061933
[9] Pallauf M, D'Andrea D, Knig F, et al. Diagnostic accuracy of clinical lymph node staging for upper tract urothelial cancer patients: a multicenter, retrospective, observational study[J]. J Urol, 2023, 209(3): 515-524. doi: 10.1097/JU.0000000000003085
[10] Kondo T, Hara I, Takagi T, et al. Template-based lymphadenectomy in urothelial carcinoma of the renal pelvis: a prospective study[J]. Int J Urol, 2014, 21(5): 453-459. doi: 10.1111/iju.12338
[11] Ikeda M, Matsumoto K, Sakaguchi K, et al. Effect of lymphadenectomy during radical nephroureterectomy in locally advanced upper tract urothelial carcinoma[J]. Clin Genitourin Cancer, 2017, 15(5): 556-562. doi: 10.1016/j.clgc.2017.04.004
[12] Dong F, Xu TY, Wang XJ, et al. Lymph node dissection could bring survival benefits to patients diagnosed with clinically node-negative upper urinary tract urothelial cancer: a population-based, propensity score-matched study[J]. Int J Clin Oncol, 2019, 24(3): 296-305. doi: 10.1007/s10147-018-1356-6
[13] Zareba P, Rosenzweig B, Winer AG, et al. Association between lymph node yield and survival among patients undergoing radical nephroureterectomy for urothelial carcinoma of the upper tract[J]. Cancer, 2017, 123(10): 1741-1750. doi: 10.1002/cncr.30516
[14] Xylinas E, Kluth L, Rieken M, et al. External validation of the pathological nodal staging score in upper tract urothelial carcinoma: a population-based study[J]. Urol Oncol, 2017, 35(1): 33. e21-33. e26.
[15] Kondo T, Hashimoto Y, Kobayashi H, et al. Template-based lymphadenectomy in urothelial carcinoma of the upper urinary tract: impact on patient survival[J]. Int J Urol, 2010, 17(10): 848-854. doi: 10.1111/j.1442-2042.2010.02610.x
[16] Kondo T, Tanabe K. Role of lymphadenectomy in the management of urothelial carcinoma of the bladder and the upper urinary tract[J]. Int J Urol, 2012, 19(8): 710-721. doi: 10.1111/j.1442-2042.2012.03009.x
[17] Kondo T, Hara I, Takagi T, et al. Template-based lymphadenectomy reduces the risk of regional lymph node recurrence among patients with upper/middle ureteral cancer [J]. Int J Clin Oncol, 2017, 22(1): 145-152. doi: 10.1007/s10147-016-1024-7
[18] Abe T, Takada N, Matsumoto R, et al. Outcome of regional lymphadenectomy in accordance with primary tumor location on laparoscopic nephroureterectomy for urothelial carcinoma of the upper urinary tract: a prospective study[J]. J Endourol, 2015, 29(3): 304-309. doi: 10.1089/end.2014.0369
[19] Rao SR, Correa JJ, Sexton WJ, et al. Prospective clinical trial of the feasibility and safety of modified retroperitoneal lymph node dissection at time of nephroureterectomy for upper tract urothelial carcinoma[J]. BJU Int, 2012, 110(11 Pt B): E475-E480. doi: 10.1111/j.1464-410X.2012.11170.x
[20] Chan VW, Wong CHM, Yuan YH, et al. Lymph node dissection for upper tract urothelial carcinoma: a systematic review[J]. Arab J Urol, 2020, 19(1): 37-45.
[21] Li CC, Chang CH, Huang CP, et al. Comparing oncological outcomes and surgical complications of hand-assisted, laparoscopic and robotic nephroureterectomy for upper tract urothelial carcinoma[J]. Front Oncol, 2021, 11: 731460. doi: 10.3389/fonc.2021.731460
[22] Kenigsberg AP, Smith W, Meng XS, et al. Robotic nephroureterectomy vs laparoscopic nephroureterectomy: increased utilization, rates of lymphadenectomy, decreased morbidity robotically[J]. J Endourol, 2021, 35(3): 312-318. doi: 10.1089/end.2020.0496
[23] Veccia A, Carbonara U, Djaladat H, et al. Robotic vs laparoscopic nephroureterectomy for upper tract urothelial carcinoma: a multicenter propensity-score matched pair tetrafecta analysis(ROBUUST collaborative group)[J]. J Endourol, 2022, 36(6): 752-759. doi: 10.1089/end.2021.0587
[24] Veccia A, Antonelli A, Francavilla S, et al. Robotic versus other nephroureterectomy techniques: a systematic review and meta-analysis of over 87, 000 cases[J]. World J Urol, 2020, 38(4): 845-852. doi: 10.1007/s00345-019-03020-1
[25] Zargar H, Krishnan J, Autorino R, et al. Robotic nephroureterectomy: a simplified approach requiring no patient repositioning or robot redocking[J]. Eur Urol, 2014, 66(4): 769-777. doi: 10.1016/j.eururo.2014.02.060
-




 下载:
下载: