Value of preoperative 18F-FDG PET/CT combined with neutrophil to lymphocyte ratio in predicting lymph node metastasis in patients undergoing radical cystectomy
-
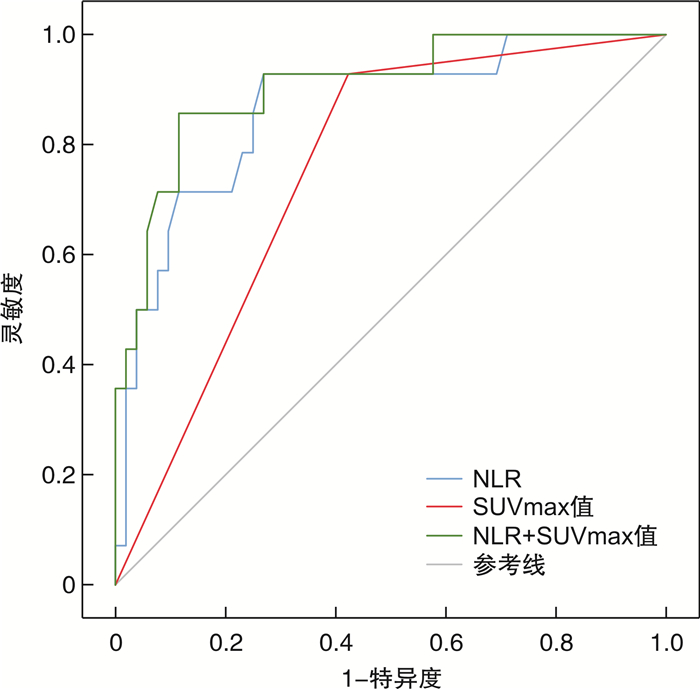
摘要: 目的 分析术前18F-氟代脱氧葡萄糖正电子发射/计算机断层显像(18F-fluorodeoxyglucose positron emission/computed tomography,18F-FDG PET/CT)中盆腔淋巴结最大标准化摄取值(maximal standardized uptake value,SUVmax)联合中性粒细胞与淋巴细胞比值(neutrophil to lymphocyte ratio,NLR)对根治性膀胱切除术(radical cystectomy,RC)患者淋巴结转移的预测价值。方法 回顾性分析2017年1月—2023年12月于首都医科大学附属北京友谊医院接受RC且术前1个月内行18F-FDG PET/CT检查的85例患者的临床资料和病理资料,最终纳入66例患者,根据术后病理结果,分为淋巴结转移组(14例)和淋巴结非转移组(52例)。收集患者18F-FDG PET/CT淋巴结SUVmax及术前1周内血常规结果,计算NLR及血小板与淋巴细胞比值(platelet to lymphocyte ratio,PLR),以淋巴结SUVmax≥2作为影像学转移截断值。应用受试者工作特征(ROC)曲线分析淋巴结SUVmax、NLR及两者联合曲线下面积(AUC)。结果 淋巴结转移组患者病理T分期、SUVmax、NLR、PLR明显高于非转移组患者(P < 0.01)。多因素logistic回归分析结果显示患者病理T分期、淋巴结SUVmax及NLR是预测病理淋巴结转移的独立危险因素(均P < 0.05)。ROC曲线显示以SUVmax≥2预测患者病理淋巴结转移的AUC为0.753(95%CI:0.626~0.879),灵敏度和特异度分别为92.9%和57.7%,阳性预测值和阴性预测值分别为37.1%和96.8%;NLR预测患者病理淋巴结转移的AUC为0.867(95%CI:0.759~0.975),根据约登指数,计算NLR最佳截断值为2.5,此时灵敏度和特异度分别为92.9%和73.1%,阳性预测值和阴性预测值分别为40.9%和97.4%;联合SUVmax和NLR后,预测病理淋巴结转移AUC为0.906(95%CI:0.816~0.995),灵敏度和特异度分别为85.7%和90.4%,阳性预测值和阴性预测值分别为70.6%和95.9%。结论 18F-FDG PET/CT淋巴结SUVmax及NLR可预测RC患者病理淋巴结转移的发生,两者联合诊断对淋巴结转移的预测价值更高。Abstract: Objective To evaluate the predictive value of 18F-fluorodeoxyglucose positron emission/computed tomography(18F-FDG PET/CT) combined with neutrophil to lymphocyte ratio(NLR) for lymph node metastasis in patients undergoing radical cystectomy.Methods A retrospective analysis was conducted on 85 patients who underwent radical cystectomy and 18F-FDG PET/CT examination one month before surgery at Beijing Friendship Hospital from January 2017 to December 2023. Based on inclusion and exclusion criteria, 66 patients were included. They were divided into lymph node metastasis group(n=14) and lymph node non-metastasis group(n=52). The 18F-FDG PET/CT lymph node SUVmax and NLR were collected. Lymph node SUVmax≥2 was considered as imaging metastasis. ROC curve was performed to analyze the area under curve of lymph node SUVmax, NLR and the combination of both.Results Pathological T stage, SUVmax, NLR and platelet to lymphocyte ratio in lymph node metastasis group were significantly higher than those in non-metastatic group(P < 0.01). Multivariate logistic regression analysis showed that pathological T stage, lymph node SUVmax and NLR were independent risk factors in predicting pathological lymph node metastasis(P < 0.05). ROC curve revealed that the AUC of SUVmax≥2 to predict pathological lymph node metastasis was 0.753(95%CI: 0.626-0.879). The sensitivity and specificity were 92.9% and 57.7%, respectively, and the positive predictive value(PPV) and negative predictive value(NPV) were 37.1% and 96.8%, respectively. NLR predicted that the AUC of patients with pathological lymph node metastasis was 0.867(95%CI: 0.759-0.975). According to the Youden index, the optimal cut-off value of NLR was 2.5. The sensitivity and specificity were 92.9% and 73.1%, respectively, and the PPV and NPV were 40.9% and 97.4%, respectively. Combined SUVmax and NLR, the AUC for predicting pathological lymph node metastasis was 0.906(95%CI: 0.816-0.995). The sensitivity and specificity were 85.7% and 90.4%, and the PPV and NPV were 70.6% and 95.9%, respectively.Conclusion Both 18F-FDG PET/CT and NLR can predict the occurrence of pathological lymph node metastasis in patients undergoing radical cystectomy, and the combined method is more valuable in diagnosis.
-
Key words:
- bladder cancer /
- pelvic lymph node metastasis /
- PET/CT /
- neutrophil /
- lymphocyte
-

-
表 1 淋巴结转移组和非转移组患者基本资料比较
例(%),X±S,M(Q1,Q3) 变量 淋巴结转移组
(14例)淋巴结非转移组
(52例)P值 年龄/岁 67.1±6.6 69.6±10.2 0.397 性别 0.178 男 10(71.4) 45(86.5) 女 4(28.6) 7(13.5) BMI/(kg/m2) 23.9±2.7 24.3±3.4 0.669 高血压 0.410 有 9(64.3) 27(51.9) 无 5(35.7) 25(48.1) 糖尿病 0.670 有 4(28.6) 12(23.1) 无 10(71.4) 40(76.9) 灌注史 0.448 有 4(28.6) 10(19.2) 无 10(71.4) 42(80.8) 手术方式 0.519 开放 5(26.3) 14(19.1) 腹腔镜 9(73.7) 38(80.9) pT分期 0.006 pT0~T2 4(28.6) 36(69.2) pT3~T4 10(71.4) 16(30.8) 淋巴结SUVmax 0.001 < 2 1(7.1) 30(57.7) ≥2 13(92.9) 22(42.3) NLR 3.12
(2.56,4.12)2.25
(1.99,2.53)< 0.001 PLR 174.4
(134.6,199.5)125.3
(96.6,158.1)0.004 表 2 病理淋巴结转移影响因素的多因素logistic回归分析
变量 OR 95%CI P值 pT分期 9.228 1.444~58.967 0.019 淋巴结SUVmax 25.042 2.133~294.029 0.010 NLR 7.864 1.082~57.182 0.042 PLR 0.989 0.961~1.018 0.455 表 3 淋巴结SUVmax、NLR及两者联合对病理淋巴结转移的预测效能
变量 AUC(95%CI) P值 灵敏度/% 特异度/% 阳性预测值/% 阴性预测值/% SUVmax 0.753(0.626~0.879) 0.004 92.9 57.7 37.1 96.8 NLR 0.867(0.759~0.975) < 0.001 92.9 73.1 40.9 97.4 SUVmax+NLR 0.906(0.816~0.995) < 0.001 85.7 90.4 70.6 95.9 -
[1] Jubber I, Ong S, Bukavina L, et al. Epidemiology of bladder cancer in 2023: a systematic review of risk factors[J]. Eur Urol, 2023, 84(2): 176-190. doi: 10.1016/j.eururo.2023.03.029
[2] Salama A, Abdelmaksoud AM, Shawki A, et al. Outcome of muscle-invasive urothelial bladder cancer after radical cystectomy[J]. Clin Genitourin Cancer, 2016, 14(1): e43-e47. doi: 10.1016/j.clgc.2015.07.007
[3] 林天歆. 膀胱癌的淋巴结清扫范围[J]. 北京大学学报(医学版), 2017, 49(4): 565-568. https://www.cnki.com.cn/Article/CJFDTOTAL-BYDB201704002.htm
[4] Ploussard G, Briganti A, de la Taille A, et al. Pelvic lymph node dissection during robot-assisted radical prostatectomy: efficacy, limitations, and complications-a systematic review of the literature[J]. Eur Urol, 2014, 65(1): 7-16. doi: 10.1016/j.eururo.2013.03.057
[5] Gloger S, Ubrig B, Boy A, et al. Bilateral peritoneal flaps reduce incidence and complications of lymphoceles after robotic radical prostatectomy with pelvic lymph node dissection-results of the prospective randomized multicenter trial ProLy[J]. J Urol, 2022, 208(2): 333-340. doi: 10.1097/JU.0000000000002693
[6] Vind-Kezunovic S, Bouchelouche K, Ipsen P, et al. Detection of lymph node metastasis in patients with bladder cancer using maximum standardised uptake value and 18F-fluorodeoxyglucose positron emission Tomography/Computed tomography: results from a high-volume centre including long-term follow-up[J]. Eur Urol Focus, 2019, 5(1): 90-96. doi: 10.1016/j.euf.2017.06.005
[7] Girard A, Rouanne M, Taconet S, et al. Integrated analysis of 18F-FDG PET/CT improves preoperative lymph node staging for patients with invasive bladder cancer[J]. Eur Radiol, 2019, 29(8): 4286-4293. doi: 10.1007/s00330-018-5959-0
[8] Voskuilen CS, van Gennep EJ, Einerhand SMH, et al. Staging 18F-fluorodeoxyglucose positron emission tomography/computed tomography changes treatment recommendation in invasive bladder cancer[J]. Eur Urol Oncol, 2022, 5(3): 366-369. doi: 10.1016/j.euo.2021.01.005
[9] Faria AVS, Andrade SS, Peppelenbosch MP, , et al. Platelets in aging and cancer-"double-edged sword"[J]. Cancer Metastasis Rev, 2020, 39(4): 1205-1221. doi: 10.1007/s10555-020-09926-2
[10] Kaushik D, Shah PK, Mukherjee N, et al. Effects of yoga in men with prostate cancer on quality of life and immune response: a pilot randomized controlled trial[J]. Prostate Cancer Prostatic Dis, 2022, 25(3): 531-538. doi: 10.1038/s41391-021-00470-w
[11] Nabavizadeh R, Bobrek K, Master VA. Risk stratification for bladder cancer: Biomarkers of inflammation and immune activation[J]. Urol Oncol, 2020, 38(9): 706-712. doi: 10.1016/j.urolonc.2020.04.006
[12] Witjes JA, Bruins HM, Carrión A, et al. European association of urology guidelines on muscle-invasive and metastatic bladder cancer: summary of the 2023 guidelines[J]. Eur Urol, 2024, 85(1): 17-31. doi: 10.1016/j.eururo.2023.08.016
[13] Leissner J, Hohenfellner R, Thüroff JW, et al. Lymphadenectomy in patients with transitional cell carcinoma of the urinary bladder; significance for staging and prognosis[J]. BJU Int, 2000, 85(7): 817-823. doi: 10.1046/j.1464-410x.2000.00614.x
[14] Steven K, Poulsen AL. Radical cystectomy and extended pelvic lymphadenectomy: survival of patients with lymph node metastasis above the bifurcation of the common iliac vessels treated with surgery only[J]. J Urol, 2007, 178(4 Pt 1): 1218-1234.
[15] Simone G, Papalia R, Ferriero M, et al. Stage-specific impact of extended versus standard pelvic lymph node dissection in radical cystectomy[J]. Int J Urol, 2013, 20(4): 390-397. doi: 10.1111/j.1442-2042.2012.03148.x
[16] Nathanson SD. Insights into the mechanisms of lymph node metastasis[J]. Cancer, 2003, 98(2): 413-423. doi: 10.1002/cncr.11464
[17] Li Y, Diao FY, Shi SY, et al. Computed tomography and magnetic resonance imaging evaluation of pelvic lymph node metastasis in bladder cancer[J]. Chin J Cancer, 2018, 37(1): 3. doi: 10.1186/s40880-018-0269-0
[18] Jeong IG, Hong S, You D, et al. FDG PET-CT for lymph node staging of bladder cancer: a prospective study of patients with extended pelvic lymphadenectomy[J]. Ann Surg Oncol, 2015, 22(9): 3150-3156. doi: 10.1245/s10434-015-4369-7
[19] Caglic I, Panebianco V, Vargas HA, et al. MRI of bladder cancer: local and nodal staging[J]. J Magn Reson Imaging, 2020, 52(3): 649-667. doi: 10.1002/jmri.27090
[20] Vartolomei MD, Porav-Hodade D, Ferro M, et al. Prognostic role of pretreatment neutrophil-to-lymphocyte ratio(NLR)in patients with non-muscle-invasive bladder cancer(NMIBC): a systematic review and meta-analysis[J]. Urol Oncol, 2018, 36(9): 389-399. doi: 10.1016/j.urolonc.2018.05.014
[21] 刘帅, 周晓洲, 段光杰, 等. 术前高中性粒细胞与淋巴细胞比值预示膀胱非尿路上皮癌患者根治术后预后不良[J]. 现代泌尿外科杂志, 2023, 28(11): 964-969. doi: 10.3969/j.issn.1009-8291.2023.11.010
[22] 薛震, 陆俊, 林嘉, 等. Ⅱ~Ⅲ期胃癌患者淋巴结转移的人工神经网络预测模型构建[J]. 中华胃肠外科杂志, 2022, 25(4): 327-335. doi: 10.3760/cma.j.cn441530-20220105-00010
[23] Hedrick CC, Malanchi I. Neutrophils in cancer: heterogeneous and multifaceted[J]. Nat Rev Immunol, 2022, 22(3): 173-187. doi: 10.1038/s41577-021-00571-6
[24] Bamias A, Merseburger A, Loriot Y, et al. New prognostic model in patients with advanced urothelial carcinoma treated with second-line immune checkpoint inhibitors[J]. J Immunother Cancer, 2023, 11(1): e005977. doi: 10.1136/jitc-2022-005977
[25] Ke ZB, Lin XD, Chen YH, et al. Role of 18F-FDG-PET/CT in combination with neutrophil-lymphocyte ratio in the diagnosis of upper urinary tract lesion: can we accurately predict malignant tumor?[J]. Front Oncol, 2021, 11: 615881. doi: 10.3389/fonc.2021.615881
-

计量
- 文章访问数: 239
- 施引文献: 0



 下载:
下载: