Study on the relationship between urinary tract infection and ureteral stent after laparoscopic radical cystectomy
-
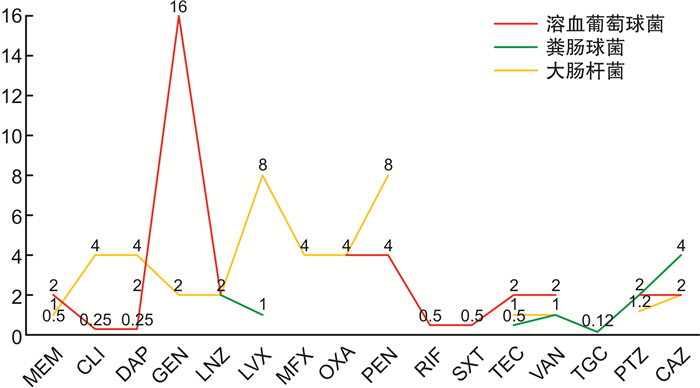
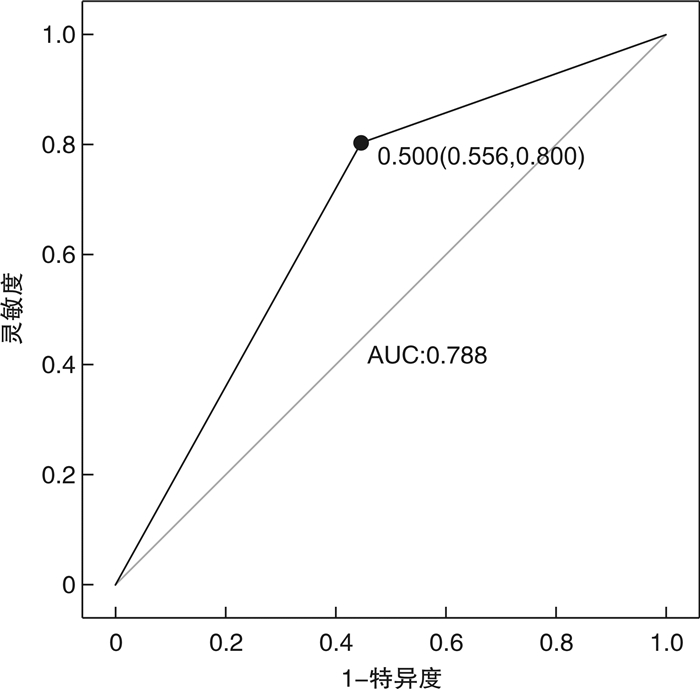
摘要: 目的 初步探讨输尿管支架管拔除后泌尿系感染的危险因素,并总结病原菌谱及其敏感药物。方法 采用前瞻性随机队列研究方法,将2019年8月—2022年10月在北京协和医院进行腹腔镜根治性膀胱切除术及肠道尿流改道术的60例患者分为试验组和对照组,每组30例。试验组拔管时预防性使用抗生素,对照组未使用。通过logistic回归分析拔管后泌尿系感染的危险因素,观察并描述药敏实验结果的差异,总结术后感染的发生规律。结果 在试验组中,导管尖端培养呈阳性的患者17例(56.67%),最终发生感染的患者8例(26.67%);而在对照组中,导管尖端培养呈阳性的患者19例(63.33%),实际发生感染的患者14例(46.67%)。在拔管后6 h内应用碳青霉烯类抗生素可以显著降低拔管后尿路感染的风险(P=0.038,OR=2.414)。体重指数增大、糖尿病史、术前白蛋白水平降低以及术后返回ICU被确定为拔管后尿路感染的独立危险因素。拔管后尿路感染的主要病原菌为大肠埃希菌和肠球菌。拔管后进行血培养以寻找致病菌存在一定的假阳性率和滞后性。结论 拔管时应用碳青霉烯抗生素可以有效降低尿路感染的发生风险。对于进行根治性膀胱切除并进行肠道尿流改道的患者,建议在拔管同时进行导管尖端培养和药敏检测,以指导后续治疗。
-
关键词:
- 腹腔镜根治性膀胱切除术 /
- 输尿管支架管 /
- 泌尿系感染 /
- 菌血症
Abstract: Objective To preliminarily investigate the risk factors in urinary tract infection(UTI) following the removal of ureteral stent, and to summarize the spectrum of pathogens and their sensitive drugs.Methods A prospective randomized grouping method was employed to conduct a case series study on 60 patients who underwent laparoscopic radical cystectomy in Peking Union Medical College Hospital from Aug. 2019 to Oct. 2022. Logistic regression analysis was used to identify the risk factors in UTI after stent removal. Differences in antimicrobial sensitivity test results were observed and described, and the patterns of postoperative infections were summarized.Results In the experimental group, 17 patients(56.67%) had positive cultures at the tip of the catheter, and 8 patients(26.67%) eventually developed infections. In the control group, 19 patients(63.33%) had positive cultures, and 14 patients(46.67%) developed infections. The application of carbapenem antibiotics within 6 hours after stent removal significantly reduced the risk of post-removal UTI(P=0.038, OR=2.414). Increased body mass index, a history of diabetes, decreased preoperative albumin levels, and postoperative return to the ICU were identified as independent risk factors in UTI after stent removal. The most common pathogens causing UTI after stent removal were Escherichia coli and Enterococcus. Blood cultures conducted after stent removal to identify pathogens had a certain false-positive rate and delayed detection.Conclusion The use of carbapenem antibiotics during stent removal effectively reduces the risk of post-removal UTI. For patients undergoing radical bladder resection with diversion of intestinal urine flow, it is recommended to conduct catheter tip cultures and antimicrobial sensitivity tests simultaneously with stent removal to guide subsequent treatment.-
Key words:
- laparoscopic radical cystectomy /
- ureteral stent /
- urinary tract infection /
- bacteremia
-

-
表 1 入组患者的基本病例、临床、病理资料
例(%),X±S 变量 对照组(30例) 试验组(30例) 培养阳性 19(63.33) 17(56.67) 实际感染发生 14(46.67) 8(26.67) 性别 男 22(73.33) 25(83.33) 女 8(26.67) 5(16.67) 年龄/岁 64.17±10.92 63.27±7.50 BMI/(kg/m2) 24.73±2.91 24.50±3.23 术后住院时间/d 23.14±8.01 23.66±10.42 高血压 13(43.33) 15(50.00) 糖尿病 10(33.33) 5(16.67) 吸烟 12(40.00) 12(40.00) 酗酒 4(13.33) 5(16.67) 多次电切 7(23.33) 13(43.33) 新辅助化疗 11(36.67) 7(23.33) 术前血红蛋白/(g/L) 128.40±21.24 135.43±17.77 术前血浆白蛋白/(g/L) 39.93±3.79 40.57±2.85 术前血肌酐/(μmol/L) 86.47±20.04 85.30±23.22 既往腹盆腔手术史 10(33.33) 9(30.00) 手术时长/min 390.67±73.27 401.50±87.60 术中出血量/mL 636.67±631.00 468.33±358.35 术中输血/单位红细胞 1.40±2.12 1.07±1.77 尿流改道方式 原位新膀胱 9(30.00) 12(40.00) 回肠膀胱 21(70.00) 18(60.00) 术后抗生素应用天数/d 6.30±2.65 6.70±3.00 淋巴结清扫数目/枚 14.97±5.87 16.57±7.97 肿瘤直径/cm 2.89±1.29 2.42±1.57 返重症监护病房 13(43.33) 6(20.00) 表 2 单因素logistic回归结果显示拔管后UTI潜在风险因素
变量 回归系数 标准误 Z P值 性别 -0.618 39 0.622 71 -0.732 0.439 年龄 0.523 26 0.712 47 0.639 0.233 BMI 1.232 44 0.022 27 1.763 0.127 术式选择 -0.434 63 0.891 41 -2.259 0.431 慢性便秘史 1.133 79 0.678 43 1.913 0.267 肠道准备药物量 1.141 55 0.304 51 1.030 0.216 腹部手术史 0.859 28 0.459 65 1.226 0.095 糖尿病史 2.168 49 0.750 12 1.321 0.031 高血压史 -0.027 92 0.521 12 -0.019 0.985 吸烟史 -2.921 01 0.648 12 -0.323 0.717 酗酒史 -1.241 49 0.895 11 -1.722 0.278 多次电切史 -2.321 05 0.626 21 -1.612 0.551 新辅助化疗 1.210 29 0.671 84 1.218 0.101 术前白蛋白 -1.413 16 0.568 21 -1.341 0.131 术前肌酐 -1.010 81 0.122 31 -0.891 0.221 术前血红蛋白 -0.069 19 0.165 11 -0.411 0.219 ASA分级 -0.918 81 0.951 29 -0.974 0.271 术中出血量 2.113 23 0.424 21 0.281 0.078 手术时长 -0.982 11 0.319 05 -0.291 0.633 输血量 1.104 05 0.312 89 0.218 0.217 初次排气时间 0.313 15 0.512 06 1.001 0.803 初次下地时间 -0.871 25 0.392 91 -0.671 0.512 抗生素应用天数 0.594 01 0.549 18 0.981 0.215 淋巴结清扫数目 0.119 18 0.292 15 0.391 0.675 肿瘤直径 -0.059 18 0.521 09 -0.141 0.681 T分期 0.981 71 0.018 94 0.665 0.517 N分期 -0.581 21 0.917 64 -0.871 0.319 是否返ICU 2.129 21 0.312 52 0.819 0.027 表 3 多因素logistic回归分析显示拔管后UTI发生的危险因素
变量 回归系数 标准误 Z P值 BMI 2.418 17 0.371 81 1.323 0.041 腹部手术史 1.891 01 0.881 53 1.457 0.295 糖尿病史 1.625 71 0.891 12 2.091 0.027 新辅助化疗 0.471 96 0.279 71 1.098 0.122 术前白蛋白 -1.290 85 0.980 91 -2.211 0.033 术中出血量 1.971 89 0.198 17 0.521 0.053 是否返ICU 2.109 83 0.412 91 0.232 0.018 表 4 LRC术后感染患者的导管尖和血液细菌培养情况
例(%) 菌种 导管尖端培养
(36例次)血液培养
(22例次)肠杆菌科 14(38.89) 9(40.91) 肠球菌 8(22.2) 6(27.27) 铜绿假单胞菌 1(2.78) 1(4.55) 金黄色葡萄球菌 3(8.33) 3(13.64) 脆弱类杆菌 2(5.56) 1(4.55) 溶血葡糖球菌 5(13.89) 1(4.55) 其他杂菌 3(8.33) 1(4.55) -
[1] van Hemelrijck M, Thorstenson A, Smith P, et al. Risk of in-hospital complications after radical cystectomy for urinary bladder carcinoma: population-based follow-up study of 7608 patients[J]. BJU Int, 2013, 112(8): 1113-1120. doi: 10.1111/bju.12239
[2] Çek M, Tandoǧdu Z, Naber K, et al. Antibiotic prophylaxis in urology departments, 2005—2010[J]. Eur Urol, 2013, 63(2): 386-394. doi: 10.1016/j.eururo.2012.09.038
[3] Shabsigh A, Korets R, Vora KC, et al. Defining early morbidity of radical cystectomy for patients with bladder cancer using a standardized reporting methodology[J]. Eur Urol, 2009, 55(1): 164-174. doi: 10.1016/j.eururo.2008.07.031
[4] Pariser JJ, Anderson BB, Pearce SM, et al. The effect of broader, directed antimicrobial prophylaxis including fungal coverage on perioperative infectious complications after radical cystectomy[J]. Urol Oncol, 2016, 34(3): 121. e9-121. e14.
[5] Haider M, Ladurner C, Mayr R, et al. Use and duration of antibiotic prophylaxis and the rate of urinary tract infection after radical cystectomy for bladder cancer: Results of a multicentric series[J]. Urol Oncol, 2019, 37(5): 300. e9-300. e15.
[6] Symeonidis EN, Falagas ME, Dimitriadis F. Urinary tract infections in patients undergoing radical cystectomy and urinary diversion: challenges and considerations in antibiotic prophylaxis[J]. Transl Androl Urol, 2019, 8(4): 286-289. doi: 10.21037/tau.2019.07.12
[7] Kolwijck E, Seegers AEM, Tops SCM, et al. Incidence and microbiology of post-operative infections after radical cystectomy and ureteral stent removal; a retrospective cohort study[J]. BMC Infect Dis, 2019, 19(1): 303. doi: 10.1186/s12879-019-3932-4
[8] Antonelli L, Sebro K, Lahmar A, et al. Association between antibiotic prophylaxis before cystectomy or stent removal and infection complications: a systematic review[J]. Eur Urol Focus, 2023, 9(4): 631-636. doi: 10.1016/j.euf.2023.01.012
[9] Hashimoto J, Takahashi S, Kurimura Y, et al. Clinical relevance of single administration of prophylactic antimicrobial agents against febrile events after removal of ureteral stents for patients with urinary diversion or reconstruction[J]. Int J Urol, 2010, 17(2): 163-166. doi: 10.1111/j.1442-2042.2009.02432.x
[10] Beano H, He JX, Hensel C, et al. Lasix renal scintigraphy results correlate with ureteroenteric stricture rates and total readmission rates following radical cystectomy[J]. J Urol, 2019, 201(Supplement 4): e355.
[11] Numao N, Fujiwara R, Uehara S, et al. Intraoperative only versus extended duration use of antimicrobial prophylaxis for infectious complications in radical cystectomy with intestinal urinary diversion[J]. Urol Int, 2020, 104(11-12): 954-959. doi: 10.1159/000509881
[12] 陈瑞廷, 赵俊峰, 董建设, 等. 泌尿外科术后尿道感染危险因素[J]. 中华医院感染学杂志, 2021, 31(7): 1047-1050. https://www.cnki.com.cn/Article/CJFDTOTAL-ZHYY202107021.htm
[13] Alemu M, Belete MA, Gebreselassie S, et al. Bacterial profiles and their associated factors of urinary tract infection and detection of extended spectrum beta-lactamase producing gram-negative uropathogens among patients with diabetes mellitus at dessie referral hospital, northeastern Ethiopia[J]. Diabetes Metab Syndr Obes, 2020, 13: 2935-2948. doi: 10.2147/DMSO.S262760
[14] Martin ET, Kaye KS, Knott C, et al. Diabetes and risk of surgical site infection: a systematic review and meta-analysis[J]. Infect Control Hosp Epidemiol, 2016, 37(1): 88-99. doi: 10.1017/ice.2015.249
[15] Zhang F, Liu XN, Tan ZW, et al. Effect of postoperative hypoalbuminemia and supplement of human serum albumin on the development of surgical site infection following spinal fusion surgery: a retrospective study[J]. Eur Spine J, 2020, 29(7): 1483-1489. doi: 10.1007/s00586-020-06306-w
[16] Parker WP, Toussi A, Tollefson MK, et al. Risk factors and microbial distribution of urinary tract infections following radical cystectomy[J]. Urology, 2016, 94: 96-101. doi: 10.1016/j.urology.2016.03.049
[17] Janifer J, Geethalakshmi S, Satyavani K, et al. Prevalence of lower urinary tract infection in South Indian type 2 diabetic subjects[J]. Indian J Nephrol, 2009, 19(3): 107-111. doi: 10.4103/0971-4065.57107
[18] Fünfstück R, Nicolle LE, Hanefeld M, et al. Urinary tract infection in patients with diabetes mellitus[J]. Clin Nephrol, 2012, 77(1): 40-48. doi: 10.5414/CN107216
[19] Chen SL, Jackson SL, Boyko EJ. Diabetes mellitus and urinary tract infection: epidemiology, pathogenesis and proposed studies in animal models[J]. J Urol, 2009, 182(6 Suppl): S51-S56.
[20] Wilke T, Boettger B, Berg B, et al. Epidemiology of urinary tract infections in type 2 diabetes mellitus patients: an analysis based on a large sample of 456, 586 German T2DM patients[J]. J Diabetes Complications, 2015, 29(8): 1015-1023. doi: 10.1016/j.jdiacomp.2015.08.021
[21] Mahdi H, Goodrich S, Lockhart D, et al. Predictors of surgical site infection in women undergoing hysterectomy for benign gynecologic disease: a multicenter analysis using the national surgical quality improvement program data[J]. J Minim Invasive Gynecol, 2014, 21(5): 901-909. doi: 10.1016/j.jmig.2014.04.003
[22] Sampathkumar P. Reducing catheter-associated urinary tract infections in the ICU[J]. Curr Opin Crit Care, 2017, 23(5): 372-377. doi: 10.1097/MCC.0000000000000441
[23] Yu SS, Fu AZ, Qiu Y, et al. Disease burden of urinary tract infections among type 2 diabetes mellitus patients in the U.S[J]. J Diabetes Complications, 2014, 28(5): 621-626. doi: 10.1016/j.jdiacomp.2014.03.012
[24] Magistro G, Zimmermann L, Bischoff R, et al. The natural course of urinalysis after urinary diversion[J]. World J Urol, 2021, 39(5): 1559-1567. doi: 10.1007/s00345-020-03355-0
-

计量
- 文章访问数: 171
- 施引文献: 0



 下载:
下载: