Effect of the number of negative lymph nodes on prognosis of patients with muscle-invasive bladder cancer
-
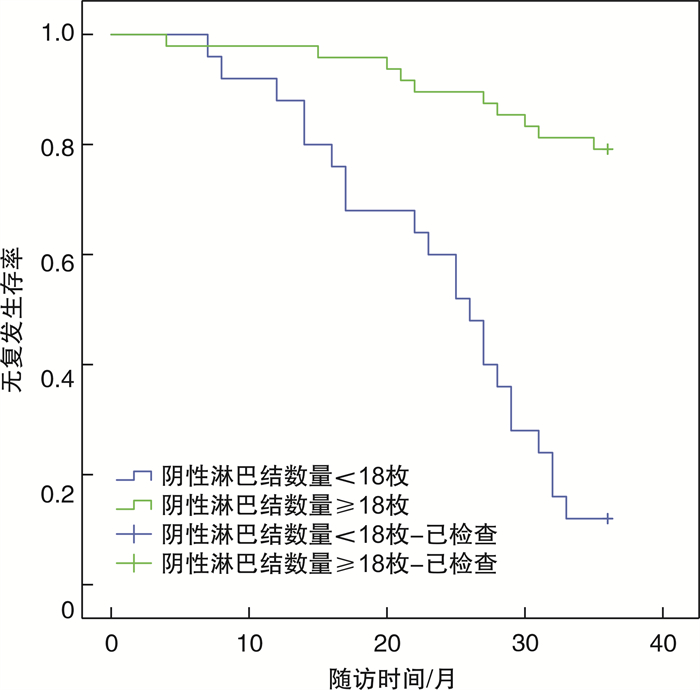
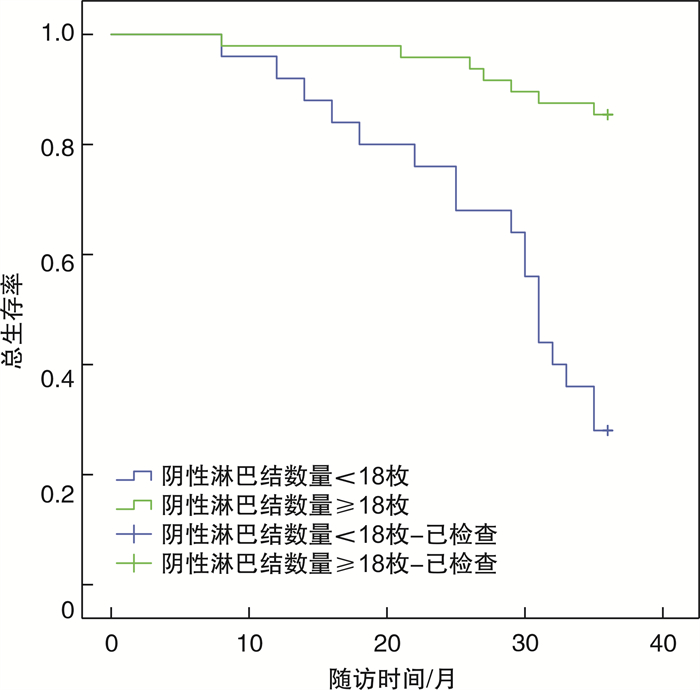
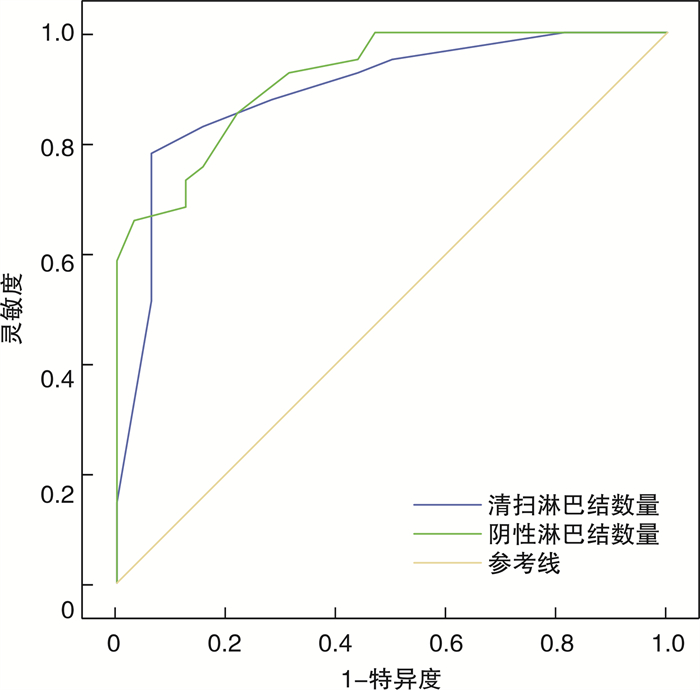
摘要: 目的 探讨肌层浸润性膀胱癌(muscle-invasive bladder cancer, MIBC)患者阴性淋巴结数量对预后的影响。方法 回顾性分析厦门大学附属东南医院2015年1月-2020年6月年收治73例接受膀胱根治性切除术的MIBC患者临床病理资料, 根据术后是否发生肿瘤复发或死亡分为预后不良组(32例)和预后良好组(41例)。根据术后病理结果计算患者阴性淋巴结总数, 绘制受试者工作特征(receiver operating characteristic, ROC)曲线分析阴性淋巴结数对预后的预测作用, 单因素和logistic多因素分析MIBC患者预后影响因素, 采用Kaplan-Meier风险曲线分析阴性淋巴结数对无复发生存期(recurrence free survival, RFS)和总生存期(overall survival, OS)的影响。结果 73例MIBC患者中, 32例肿瘤复发, 复发率43.84%, 复发时间4~35个月, 平均22.72个月; 25例死亡, 死亡率34.25%, 死亡时间8~36个月, 平均25.68个月。单因素分析发现肿瘤最大长径≥3 cm、临床分期Ⅲ~Ⅳ期、淋巴结转移、清扫淋巴结数量 < 23枚、阴性淋巴结数量 < 18枚与MIBC预后不良相关(P < 0.05)。多因素分析发现肿瘤最大长径≥3 cm (OR=9.125, 95%CI: 1.987~14.371)、临床分期Ⅲ~Ⅳ期(OR=8.377, 95%CI: 1.965~12.752)、清扫淋巴结数量 < 23枚(OR=16.346, 95%CI: 5.081~28.646)、阴性淋巴结数量 < 18枚(OR=22.043, 95%CI: 5.625~44.245)是MIBC预后不良的独立危险因素。Kaplan-Meier分析结果显示, 阴性淋巴结数量 < 18枚患者RFS短于阴性淋巴结数量≥18枚患者(χ2=37.610, P < 0.001), 阴性淋巴结数量 < 18枚患者OS短于阴性淋巴结数量≥18枚患者(χ2=26.690, P < 0.001)。结论 阴性淋巴结数量 < 18枚是MIBC患者预后不良的危险因素, 对患者预后具有预测价值, 可以作为临床预后评估指标。Abstract: Objective To investigate the effect of the number of negative lymph nodes on the prognosis of patients with muscle-invasive bladder cancer (MIBC).Methods The clinicopathological data of 73 MIBC patients who were admitted to the Dongnan Hospital of Xiamen University and underwent radical cystectomy from January 2015 to June 2020 were retrospectively analyzed.The patients were divided into poor prognosis group (n=32) and good prognosis group (n=41) according to whether tumor recurrence or death occurred after surgery.The total number of negative lymph nodes was calculated according to postoperative pathological results, then the ROC curve was drawn to analyze the predictive effect of negative lymph nodes on prognosis.Univariate and logistic multivariate analysis were used to analyze prognostic factors in MIBC patients.The effects of the number of negative lymph nodes on recurrence free survival (RFS) and overall survival (OS) were analyzed by Kaplan-Meier risk curve.Results Among the 73 patients with MIBC, 32 cases had tumor recurrence, and the recurrence rate was 43.84%.The recurrence time was 4-35 months, with an average of 22.72 months.Twenty-five cases died, and the mortality rate was 34.25%.The death time was 8-36(mean 25.68) months.Univariate analysis showed that the maximum length of tumor ≥3 cm, clinical stage Ⅲ-Ⅳ, lymph node metastasis, the number of lymph nodes dissected < 23, the number of negative lymph nodes < 18 were associated with poor prognosis of MIBC (P < 0.05).Multivariate analysis showed that the maximum length and diameter of the tumor ≥3 cm (OR=9.125, 95%CI: 1.987-14.371), clinical stage Ⅲ-Ⅳ(OR=8.377, 95%CI: 1.965-12.752), the number of lymph nodes dissected < 23(OR=16.346, 95%CI: 5.081-28.646), the number of negative lymph nodes < 18(OR=22.043, 95%CI: 5.625-44.245) were independent risk factors in poor prognosis of MIBC.Kaplan-Meier analysis showed that RFS of patients with negative lymph nodes < 18 were shorter than that of patients with negative lymph nodes ≥18(χ2=37.610, P < 0.001), and OS of patients with negative lymph nodes < 18 was shorter than that of patients with negative lymph nodes ≥ 18(χ2=26.690, P < 0.001).Conclusion The number of negative lymph nodes less than 18 is a risk factor in poor prognosis in patients with MIBC, which has predictive value for patients'prognosis and can be used as an indicator for clinical prognosis evaluation.
-
Key words:
- number of negative lymph nodes /
- bladder cancer /
- lymph nodes /
- radical cystectomy /
- prognosis /
- recurrence
-

-
表 1 73例MIBC患者预后单因素分析
例,X±S 因素 预后不良组
(32例)预后良好组
(41例)t/χ2 P值 年龄/岁 62.25±5.30 62.21± 4.56 0.026 0.979 性别 0.139 0.723 男 28 37 女 4 4 BMI/(kg/m2) 23.55±0.44 23.71± 0.42 -1.606 0.113 糖尿病 0.603 0.437 是 6 5 否 26 36 高血压 0.692 0.406 是 8 7 否 24 34 吸烟 0.064 0.800 是 17 23 否 15 18 肾积水 2.924 0.087 是 12 8 否 20 33 手术方式 0.088 0.767 开腹 12 14 腹腔镜 20 27 肿瘤最大长径/cm 9.017 0.003 ≥3 17 8 < 3 15 33 肿瘤分化 0.015 0.902 低分化 9 11 中高分化 23 30 病理类型 0.575 0.448 高级别 12 19 低级别 20 22 临床分期 5.059 0.024 Ⅲ~Ⅳ期 15 9 Ⅱ期 17 32 肿瘤个数 0.486 0.486 多发 11 11 单发 21 30 淋巴结转移 7.136 0.008 是 21 14 否 11 27 清扫淋巴结数量/枚 35.718 < 0.001 < 23 28 7 ≥23 4 34 阴性淋巴结数量/枚 30.122 < 0.001 < 18 22 3 ≥18 10 38 表 2 73例MIBC患者预后多因素分析
因素 β SE Wald χ2 OR 95%CI P值 肿瘤最大长径≥3 cm 2.211 1.135 3.796 9.125 1.987~14.371 0.041 临床分期Ⅲ~Ⅳ期 2.126 1.103 3.714 8.377 1.965~12.752 0.044 淋巴结转移 1.907 1.450 1.729 6.733 0.909~12.548 0.189 清扫淋巴结数量 < 23枚 2.794 1.106 6.381 16.346 5.081~28.646 0.001 阴性淋巴结数量 < 18枚 3.093 1.718 3.241 22.043 5.625~44.245 0.003 -
[1] Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries[J]. CA Cancer J Clin, 2021, 71(3): 209-249. doi: 10.3322/caac.21660
[2] 王淼, 章小平. EAU 2024热点速递: 肌层浸润性膀胱癌的临床进展[J]. 临床泌尿外科杂志, 2024, 39(6): 547-550. https://lcmw.whuhzzs.com/article/doi/10.13201/j.issn.1001-1420.2024.06.017
[3] 冯国伟, 宋鸽, 张振庭, 等. 新辅助免疫联合用于治疗肌层浸润性膀胱癌的研究进展[J]. 中华泌尿外科杂志, 2022, 4(4): 309-312. doi: 10.3760/cma.j.cn112330-20210430-00245
[4] Feldman AS, Kulkarni GS, Bivalacqua TJ, et al. Surgical challenges and considerations in Tri-modal therapy for muscle invasive bladder 5 cancer[J]. Urol Oncol, 2022, 40(10): 442-450. doi: 10.1016/j.urolonc.2021.01.013
[5] Zhou Y, Yang H, Liang ZH. Efficiency and safety of laparoscopic radical cystectomy for muscle-invasive bladder cancer, and postoperative recurrence[J]. Arch Esp Urol, 2023, 76(3): 196-202. doi: 10.56434/j.arch.esp.urol.20237603.23
[6] Zhang XX, Zhang AX, Hu LS, et al. An innovative risk index based on neutrophils and macrophages can effectively predict prognosis and immunotherapy response in patients with muscle-invasive bladder cancer[J]. Transl Cancer Res, 2023, 12(3): 536-549. doi: 10.21037/tcr-22-2255
[7] Katims AB, Bochner BH. Extended pelvic lymph node dissection in muscle invasive bladder cancer[J]. Curr Opin Urol, 2023, 33(4): 252-257. doi: 10.1097/MOU.0000000000001096
[8] 蒋铭心, 牛亦农. 根治性膀胱切除术中盆腔淋巴结清扫的研究进展[J]. 临床泌尿外科杂志, 2024, 39(6): 534-538. https://lcmw.whuhzzs.com/article/doi/10.13201/j.issn.1001-1420.2024.06.014
[9] Yu L, Zhang XT, Guan SH, et al. The number of negative lymph nodes is positively associated with survival in esophageal squamous cell carcinoma patients in China[J]. Open Med, 2020, 15: 152-159. doi: 10.1515/med-2020-0023
[10] Cui J, Zhang L, Yang L, et al. The prognostic signifificance of the treatment response of regional lymph nodes and the refifinement of the current TNM staging system in locally advanced rectal cancer after neoadjuvant chemoradiotherapy[J]. Cancer Med, 2020, 9(24): 9373-9384. doi: 10.1002/cam4.3553
[11] Liu LM, Ren JG, Wang G, et al. Negative lymph node is an independent prognostic factor for stage Ⅲ gastric cancer patients after curative gastrectomy: a surveillance, epidemiology, and end results-based study[J]. Am Surg, 2023, 89(11): 4413-4423. doi: 10.1177/00031348221114034
[12] Peña KB, Riu F, Gumà J, et al. Immunohistochemical algorithm for the classification of muscle-invasive urinary bladder carcinoma with lymph node metastasis: an institutional study[J]. J Clin Med, 2022, 11(24): 7430. doi: 10.3390/jcm11247430
[13] 石丰华, 邱建新. 根治性膀胱切除术时淋巴结清扫的研究概况[J]. 国际泌尿系统杂志, 2021, 5(5): 932-935. doi: 10.3760/cma.j.cn431460-20200326-00044
[14] Lenis AT, Lec PM, Michel J, et al. Predictors of adequate lymph node dissection in patients with non-muscle invasive bladder cancer undergoing radical cystectomy and effect on survival[J]. Urol Oncol, Urol Oncol, 2020, 38(10): 796.
[15] Choi SY, You D, Hong B, et al. Impact of lymph node dissection in radical cystectomy for bladder cancer: How many vs how far?[J]. Surg Oncol, 2019, 30: 109-116. doi: 10.1016/j.suronc.2019.06.008
[16] 李金洲, 黄泽平, 穆彦熹, 等. 阴性淋巴结数目在实体肿瘤预后中的价值[J]. 肿瘤防治研究, 2022, 8(8): 843-849. https://www.cnki.com.cn/Article/CJFDTOTAL-ZLFY202208016.htm
[17] Kronstedt S, Doppalapudi SK, Boyle J, et al. Does time to adjuvant chemotherapy after radical cystectomy affect survival in muscle invasive bladder cancer?A systematic review[J]. Cancers, 2022, 14(22): 5644. doi: 10.3390/cancers14225644
[18] Gu PF, Deng JY, Wang W, et al. Impact of the number of examined lymph nodes on stage migration in node-negative gastric cancer patients: a Chinese multi-institutional analysis with propensity score matching[J]. Ann Transl Med, 2020, 8(15): 938. doi: 10.21037/atm-19-4727
[19] Tochigi K, Nagayama J, Bando S, et al. Relationship between the number of lymph nodes dissected and prognosis in muscle-invasive bladder cancer in the era of neoadjuvant chemotherapy[J]. Int J Urol, 2022, 29(11): 1264-1270. doi: 10.1111/iju.14974
[20] Xiong Y, Huang F, Li XZ, et al. CCL21/CCR7 interaction promotes cellular migration and invasion via modulation of the MEK/ERK1/2 signaling pathway and correlates with lymphatic metastatic spread and poor prognosis in urinary bladder cancer[J]. Int J Oncol, 2017, 51(1): 75-90. doi: 10.3892/ijo.2017.4003
[21] Xu ZA, Zeng H, Liu ZP, et al. Poor clinical outcomes and immunoevasive contexture in SIRPα+tumor-associated macrophages enriched muscle-invasive bladder cancer patients[J]. Urol Oncol, 2022, 40(3): 109. e11-109. e20. doi: 10.1016/j.urolonc.2021.08.024
[22] 储永波, 柯昌兴. 膀胱癌淋巴结转移机制的研究进展[J]. 国际泌尿系统杂志, 2020, 40(5): 933-935.
[23] Hwang EC, Sathianathen NJ, Imamura M, et al. Extended versus standard lymph node dissection for urothelial carcinoma of the bladder in patients undergoing radical cystectomy[J]. Cochrane Database Syst Rev, 2019, 5(5): CD013336.
[24] Lee W, Nam W, Lim B, et al. Impact of preoperative chemotherapy on pathologic nodal status in muscle-invasive bladder cancer: optimal lymphadenectomy in the preoperative chemotherapy era[J]. J Cancer Res Clin Oncol, 2022, 148(9): 2507-2515.
[25] Małkiewicz B, Kiełb P, Gurwin A, et al. The usefulness of lymphadenectomy in bladder cancer-current status[J]. Medicina, 2021, 57(5): 415.
-




 下载:
下载: