Experience of delivery resection surgical policies of giant tumor in retroperitoneal adrenal region: a report of 24 cases
-
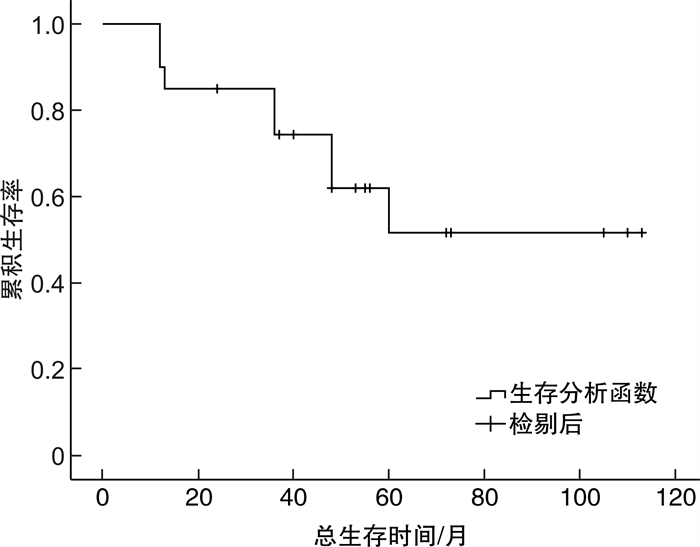
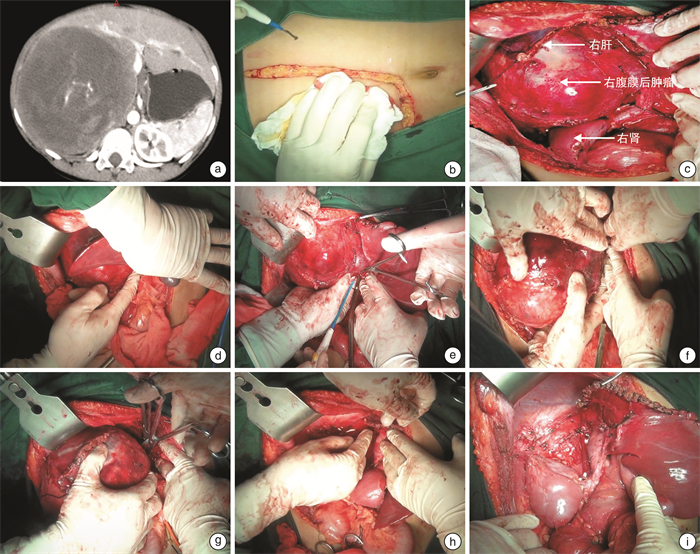
摘要: 目的 探索分娩式三步法手术治疗腹膜后肾上腺区巨大肿瘤的经验方法。方法 回顾性分析2013年7月-2020年12月江西省肿瘤医院收治的24例肿瘤长径≥10 cm的腹膜后肾上腺区肿瘤患者临床资料, 手术治疗策略为分娩式三步法。其中男17例, 女7例, 平均年龄(54±17)岁; 肿瘤平均直径(17.6±6.4) cm, 位于左侧11例, 右侧13例。手术治疗策略: 第一步, 打开侧腹膜, 游离肿瘤四周疏松组织, 扩大间隙, 解剖肿瘤与毗邻脏器关系; 第二步, 托举并向外下方牵引肿瘤, 精准处理肿瘤与重要血管、脏器的关系, "分娩"出肿瘤; 第三步, 创面严格止血, 检查临近脏器有无损伤。分析手术时间、出血量、输血量、病理结果, 并进行生存随访。结果 本研究24例手术均顺利完成, 平均手术时间(300±84) min, 平均术中出血量(1 018±965) mL; 完整肿瘤切除的20例, 分块切除、肿瘤有残留的4例; 联合脏器切除15例, 涉及肾12例, 脾脏6例, 胰腺5例, 肠管2例, 胃1例, 胆囊1例, 肝脏1例。病理: 恶性肿瘤20例, 良性肿瘤4例, 其中脂肪肉瘤11例, 炎性肌纤维母细胞瘤3例, 肾上腺皮质癌2例, 绒癌1例, 精原细胞瘤1例, 肾上腺节细胞神经母细胞瘤1例, 肾上腺神经母细胞瘤1例, 副神经节瘤2例, 孤立性纤维肿瘤1例, 嗜铬细胞瘤1例。患者均恢复良好出院。恶性肿瘤中位随访时间50.5个月, 肿瘤1、3、5年总生存率分别为90.0%、74.4%和51.6%。结论 分娩式三步法手术治疗腹膜后肾上腺区巨大肿瘤简单有效, 并发症少, 值得推广。Abstract: Objective To explore the experience and method of three-step delivery surgery for the treatment of giant tumors in the retroperitoneal adrenal region.Methods A retrospective analysis was conducted on the clinical data of 24 patients with retroperitoneal adrenal tumors with a tumor diameter ≥10 cm admitted to Jiangxi Cancer Hospital from July 2013 to December 2020.The surgical treatment strategy was a three-step delivery method.Among them, there were 17 males and 7 females, with an average age of (54±17) years.The average size of the tumor was (17.6±6.4) cm, located in 11 cases on the left and 13 cases on the right.Surgical treatment strategy: The first step is to open the lateral peritoneum, free the loose tissue around the tumor, expand the gap, and dissect the relationship between the tumor and adjacent organs; The second step is to lift and pull the tumor outwards and downwards, accurately handle the relationship between the tumor and important blood vessels and organs, and "deliver" the tumor; The third step is to strictly stop bleeding on the wound and check for damage to nearby organs.The surgical time, bleeding volume, blood transfusion volume and pathological results were analyzed, and survival follow-up was conducted.Results All 24 surgeries in this study were successfully completed, with surgical time of (300±84) min, intraoperative bleeding of (1 018±965) mL.Tumors were completely resected in 20 cases, and the other four cases experienced block resection and residual tumor.Multiple organs were resected in 15 cases, involving kidney in 12 cases, spleen in 6 cases, pancreas in 5 cases, intestine in 2 cases, stomach in 1 case, gallbladder in 1 case, and liver in 1 case.Pathology results showed that 20 cases were malignant tumors, and 4 cases were benign tumors, including 11 cases of liposarcoma, 3 cases of inflammatory myofibroblastoma, 2 cases of adrenal cortical carcinoma, 1 case of choriocarcinoma, 1 case of seminoma, 1 case of adrenal ganglioneuroblastoma, 1 case of adrenal neuroblastoma, 2 cases of paraganglioma, 1 case of solitary fibroma, and 1 case of pheochromocytoma.All patients recovered well and were discharged.The median follow-up time for malignant tumors was 50.5 months, and the overall survival rates at 1 year, 3 years, and 5 years were 90.0%, 74.4%, and 51.6%, respectively.Conclusion The three-step delivery method for the treatment of giant tumors in the retroperitoneal adrenal region is simple and effective with fewer complications, so is worth promoting.
-
Key words:
- retroperitoneal tumor /
- delivery /
- open surgery
-

-
表 1 手术时间与出血量相关因素分析
例,X±S 项目 肿瘤直径 肿瘤侵犯 >15 cm ≤15 cm 有 无 例数 14 10 13 11 手术时间/min 318±90 288±72 330±961) 258±30 手术出血量/mL 1136±1 032 855±899 1280±9181) 583±829 在肿瘤侵犯的评估中,与无肿瘤侵犯比较,1)P < 0.05。 -
[1] 尤爱军. 旋后肩法在肩难产处理中的应用[J]. 中华护理杂志, 2015, 50(11): 1318-1321. doi: 10.3761/j.issn.0254-1769.2015.11.007
[2] Neville A, Herts BR. CT characteristics of primary retroperitoneal neoplasms[J]. Crit Rev Comput Tomogr, 2004, 45(4): 247-270. doi: 10.3109/10408370490506616
[3] 罗成华. 腹膜后肿瘤[M]. 北京: 人民卫生出版社, 2013.
[4] Porter GA, Baxter NN, Pisters PW. Retroperitoneal sarcoma: a population-based analysis of epidemiology, surgery, and radiotherapy[J]. Cancer, 2006, 106(7): 1610-1616. doi: 10.1002/cncr.21761
[5] Munoz P, Bretcha-Boix P, Artigas V, et al. Surgical principles of primary retroperitoneal sarcoma in the era of personalized treatment: a review of the frontline extended surgery[J]. Cancers, 2022, 14(17): 4091. doi: 10.3390/cancers14174091
[6] Callegaro D, Raut CP, Ng D, et al. Has the outcome for patients who undergo resection of primary retroperitoneal sarcoma changed over time?A study of time trends during the past 15years[J]. Ann Surg Oncol, 2021, 28(3): 1700-1709. doi: 10.1245/s10434-020-09065-6
[7] Gronchi A, Vullo SL, Fiore M, et al. Aggressive surgical policies in a retrospectively reviewed single-institution case series of retroperitoneal soft tissue sarcoma patients[J]. J Clin Oncol, 2009, 27(1): 24-30. doi: 10.1200/JCO.2008.17.8871
[8] 龚宇, 宋波, 李为兵, 等. 腹膜后巨大肿瘤的手术切除[J]. 临床泌尿外科杂志, 2004, 19(10): 580-582, 641. https://www.cnki.com.cn/Article/CJFDTOTAL-LCMW200410001.htm
[9] Callegaro D, Miceli R, Brunelli C, et al. Long-term morbidity after multivisceral resection for retroperitoneal sarcoma[J]. Br J Surg, 2015, 102(9): 1079-1087. doi: 10.1002/bjs.9829
[10] Fiore M, Baia M, Conti L, et al. Residual adrenal function after multivisceral resection with adrenalectomy in adult patients[J]. JAMA Surg, 2022, 157(5): 415-423. doi: 10.1001/jamasurg.2021.7588
[11] Gorji L, Nikahd M, Onuma A, et al. Comparing multivisceral resection with tumor-only resection of liposarcoma using the win ratio[J]. Ann Surg Oncol, 2024, 31(5): 3389-3396. doi: 10.1245/s10434-024-14985-8
[12] Guo Q, Zhao JC, Du XJ, et al. Survival outcomes of surgery for retroperitoneal sarcomas: a systematic review and meta-analysis[J]. PLoS One, 2022, 17(7): e0272044. doi: 10.1371/journal.pone.0272044
[13] Gladdy RA, Gupta A, Catton CN. Retroperitoneal sarcoma: fact, opinion, and controversy[J]. Surg Oncol Clin N Am, 2016, 25(4): 697-711. doi: 10.1016/j.soc.2016.05.003
[14] García-Aceituno L, Villarreal-Garza C, Perfecto M, et al. Retroperitoneal soft tissue sarcomas: experience at a single institution in Mexico[J]. World J Surg, 2010, 34(7): 1511-1516. doi: 10.1007/s00268-010-0473-9
-




 下载:
下载: