Analysis of the distribution of pathogenic bacteria and risk factors of infection caused by indwelling urinary catheter after radical prostatectomy for prostate cancer
-
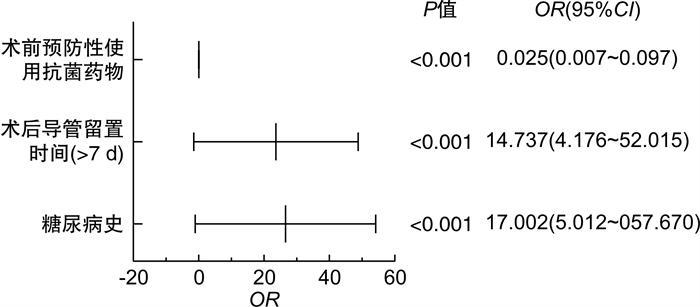
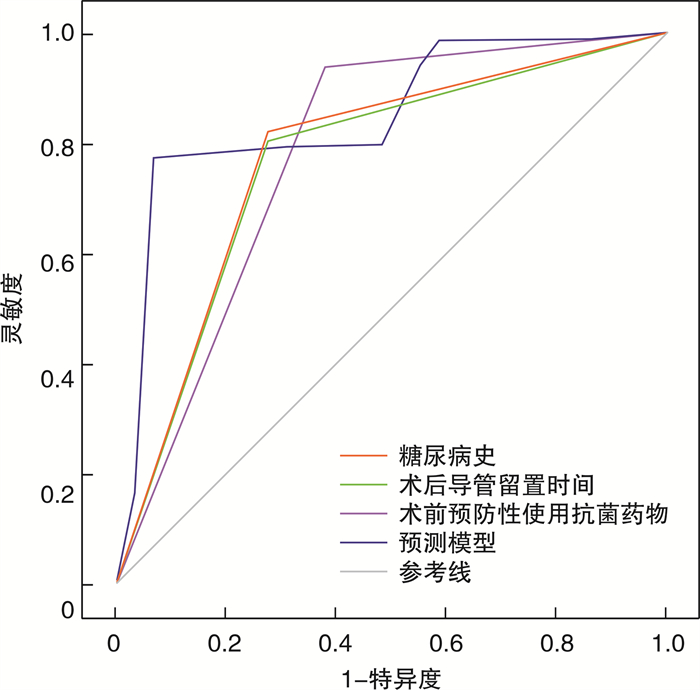
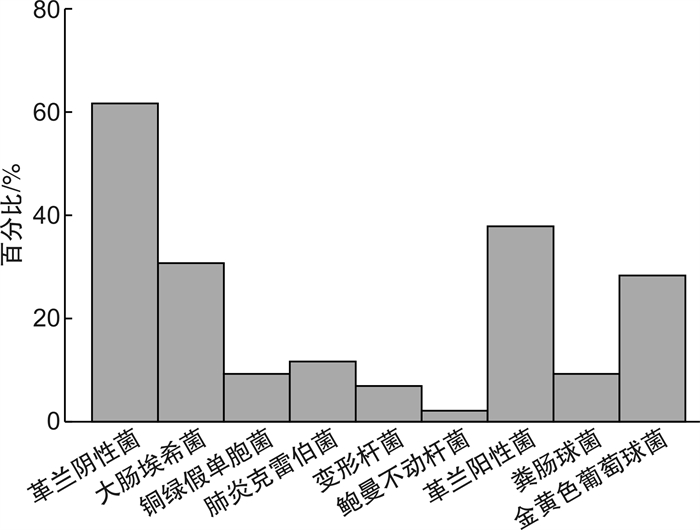
摘要: 目的 探究前列腺癌根治术后留置尿管所致感染的病原菌分布及危险因素分析。方法 回顾性分析2019年10月-2023年10月在荣县人民医院和自贡市第一人民医院收治的符合纳入排除标准的320例行前列腺癌根治术患者的临床资料。分析患者留置尿管所致感染发生率与病原菌分布状况, 主要革兰阴性菌、主要革兰阳性菌耐药情况。分析感染组与未感染组的临床资料差异, 通过二元logistic回归模型分析前列腺癌根治术后留置尿管所致感染的影响因素。结果 320例患者中发生尿路感染29例(9.06%), 29例患者中检出病原菌42株, 其中革兰阴性菌26株, 占比61.9%, 最主要菌株为大肠埃希菌; 革兰阳性菌16株, 占比38.1%, 最主要菌株为金黄色葡萄球菌。主要革兰阴性菌(大肠埃希菌)主要耐药药物为哌拉西林、氨苄西林, 主要革兰阳性菌(金黄色葡萄球菌)主要耐药药物为红霉素、青霉素、苯唑西林。二元logistic回归模型显示, 年龄不是前列腺癌根治术后留置尿管所致感染发生的影响因素(P>0.05), 糖尿病史、术后导管留置时间(>7 d)、术前预防性使用抗菌药物均为前列腺癌根治术后留置尿管所致感染发生的影响因素(P < 0.05)。受试者工作特征(receiver operating characteristic, ROC)曲线分析显示, 糖尿病史、术后导管留置时间、术前预防性使用抗菌药物预测前列腺癌根治术后留置尿管所致感染发生的曲线下面积(AUC)分别为0.773、0.764、0.781。预测模型(预测模型=2.833×糖尿病史+2.69×术后导管留置时间-3.67×术前预防性使用抗菌药物)预测前列腺癌根治术后留置尿管所致感染发生的AUC为0.850, 灵敏度、特异度分别为77.7%、93.1%。结论 前列腺癌根治术后留置尿管所致感染菌株主要为革兰阴性菌, 糖尿病史、术后导管留置时间(>7 d)、术前预防性使用抗菌药物均为前列腺癌根治术后留置尿管所致感染发生的影响因素, 临床需加强重视。Abstract: Objective To investigate the distribution of pathogenic bacteria and risk factors in infection caused by indwelling urinary catheter after radical prostatectomy for prostate cancer.Methods The clinical data of 320 radical prostatectomy patients who were admitted to Rong County People's Hospital and First People's Hospital of Zigong from October 2019 to October 2023 and meet the inclusion and exclusion criteria were collected and analyzed retrospectively.We analyzed the incidence of infection caused by indwelling urinary catheter and the distribution of pathogenic bacteria, the antibiotic resistance rates of the major gram-negative and gram-positive bacteria.The difference between the clinical data of the infected group and the uninfected group was compared, and the factors affecting the infection caused by indwelling urinary catheter after radical prostatectomy were analyzed through the binary logistic regression model.Results Urinary tract infection occurred in 29 of 320 patients, accounting for 9.06%, and 42 strains of pathogenic bacteria were detected in the 29 patients.Twenty-six strains of gram-negative bacteria accounted for 61.9%, and the most predominant strain was Escherichia coli, while 16 strains of gram-positive bacteria accounted for 38.1%, and the most predominant strain was Staphylococcus aureus.The main resistant drugs for the major gram-negative bacteria (Escherichia coli) were piperacillin and ampicillin, while the main resistant drugs for the major gram-positive bacteria (Staphylococcus aureus) were erythromycin, penicillin, and oxacillin.Binary logistic regression model showed that age was not an influential factor in the occurrence of infection due to indwelling urinary catheter after radical prostate cancer surgery (P>0.05), but history of diabetes mellitus, duration of postoperative catheter tube retention (>7 d), and preoperative prophylactic antimicrobial drugs were influential factors in the occurrence of infection due to indwelling urinary catheter after radical prostate cancer surgery (P < 0.05).ROC curve analysis showed that the AUCs of history of diabetes mellitus, postoperative catheter tube retention time, and preoperative prophylactic use of antimicrobial drugs to predict the occurrence of infection due to indwelling urinary catheter after radical prostatectomy for prostate cancer were 0.773, 0.764, 0.781, respectively.The AUC for the occurrence of infection due to indwelling urinary catheter after radical prostate cancer surgery was 0.850, calculated by the prediction model (Prediction model=2.833×History of diabetes mellitus+2.69×Postoperative catheter tube retention time-3.67×Preoperative prophylactic use of antimicrobial drugs) with a sensitivity and specificity of 77.7% and 93.1%, respectively.Conclusion The strains of infection due to indwelling urinary catheter after radical prostate cancer surgery are mainly gram-negative bacteria.The history of diabetes, postoperative catheter tube retention time (>7 d), and preoperative prophylactic use of antimicrobials are all influencing factors in the occurrence of infection due to indwelling urinary catheter after radical prostate cancer surgery, which needs much attention.
-

-
表 1 尿路感染病原菌分布
病原菌 株数 构成比/% 革兰阴性菌 26 61.90 大肠埃希菌 13 30.95 铜绿假单胞菌 4 9.52 肺炎克雷伯菌 5 11.90 变形杆菌 3 7.14 鲍曼不动杆菌 1 2.38 革兰阳性菌 16 38.10 粪肠球菌 4 9.52 金黄色葡萄球菌 12 28.57 表 2 主要革兰阴性菌耐药情况
抗菌药物 大肠埃希菌(13株) 株数 耐药率/% 氨曲南 3 23.08 阿莫西林 3 23.08 头孢哌酮/舒巴坦 3 23.08 头孢吡肟 3 23.08 头孢克洛 4 30.77 庆大霉素 4 30.77 头孢呋辛 5 38.46 头孢噻肟 6 46.15 苯唑西林 6 46.15 氨苄西林/舒巴坦 7 53.85 亚胺培南 8 61.54 环丙沙星 9 69.23 氨苄西林 11 84.62 哌拉西林 12 92.31 表 3 主要革兰阳性菌耐药情况
抗菌药物 金黄色葡萄球菌(12株) 株数 耐药率/% 万古霉素 0 0 喹诺酮 3 25.00 克林霉素 3 25.00 头孢呋辛 3 25.00 头孢唑林 4 33.33 环丙沙星 4 33.33 氧氟沙星 5 41.67 苯唑西林 9 75.00 青霉素 10 83.33 红霉素 12 100.00 表 4 2组患者临床资料比较
例(%) 指标 感染组
(29例)未感染组
(291例)χ2 P值 年龄/岁 7.068 0.008 < 60 6(20.69) 135(46.39) ≥60 23(79.31) 156(53.61) BMI/(kg/m2) 0.054 0.817 < 24 13(44.83) 137(47.08) ≥24 16(55.17) 154(52.92) 高血压史 0.010 0.919 有 9(31.03) 93(31.96) 无 20(68.97) 198(68.04) 糖尿病史 44.558 < 0.001 有 21(72.41) 52(17.87) 无 8(27.59) 239(82.13) 病理分期 3.155 0.076 T1~T2 15(51.72) 198(68.04) T3~T4 14(48.28) 93(31.96) 手术时长/min 1.501 0.220 ≤60 8(27.59) 114(39.18) >60 21(72.41) 177(60.82) 导尿管置入方法 2.608 0.106 严格无菌操作 21(72.41) 245(84.19) 相对无菌操作 8(27.59) 46(15.81) 术后导管留置时间/d 39.924 < 0.001 ≤7 8(27.59) 234(80.41) >7 21(72.41) 57(19.59) 术前预防性使用抗菌药物 85.589 < 0.001 是 11(37.93) 274(94.16) 否 18(62.07) 17(5.84) 表 5 自变量赋值
变量 赋值 年龄 1= < 60岁;2=≥60岁 糖尿病史 1=有;2=无 术后导管留置时间 1=≤7 d;2=>7 d 术前预防性使用抗菌药物 1=是;2=否 表 6 前列腺癌根治术后留置尿管所致感染的影响因素logistic回归分析
变量 B SE Wald P值 OR 95%CI 年龄(≥60岁) 1.099 0.670 2.69 0.101 3.001 0.807~11.156 糖尿病史 2.833 0.623 20.671 < 0.001 17.002 5.012~57.670 术后导管留置时间(>7 d) 2.690 0.643 17.482 < 0.001 14.737 4.176~52.015 术前预防性使用抗菌药物 -3.670 0.683 28.843 < 0.001 0.025 0.007~0.097 常量 -2.861 0.733 15.241 < 0.001 0.057 表 7 预测模型预测前列腺癌根治术后留置尿管所致感染的价值效能
项目 AUC 标准误 渐近显著性水平 95%置信区间 cut-off值 灵敏度 特异度 约登指数 下限值 上限值 糖尿病史 0.773 0.050 < 0.001 0.675 0.871 1.500 0.821 0.276 0.097 术后导管留置时间 0.764 0.050 < 0.001 0.666 0.862 1.500 0.804 0.276 0.080 术前预防性使用抗菌药物 0.781 0.056 < 0.001 0.672 0.890 1.500 0.942 0.379 0.321 预测模型 0.850 0.038 < 0.001 0.776 0.924 4.612 0.777 0.931 0.708 -
[1] Bergengren O, Pekala KR, Matsoukas K, et al. 2022 update on prostate cancer epidemiology and risk factors-a systematic review[J]. Eur Urol, 2023, 84(2): 191-206. doi: 10.1016/j.eururo.2023.04.021
[2] Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020. GLOBOCAN estimates of inc idence and mortality worldwide for 36 cancers in 1 85 countries[J]. CA Cancer J Clin, 2021, 71(3): 209-249. doi: 10.3322/caac.21660
[3] 杨云开, 胡毓祺, 王晶运, 等. 前列腺根治术前肥胖相关的生化指标对前列腺癌患者预后的意义[J]. 临床泌尿外科杂志, 2022, 37(1): 42-46. https://lcmw.whuhzzs.com/article/doi/10.13201/j.issn.1001-1420.2022.01.010
[4] 张小林, 曾燕, 丁雪飞, 等. 机器人辅助腹腔镜前列腺癌根治术后三腔导尿管最佳引流方式的研究[J]. 实用临床医药杂志, 2022, 26(15): 1-4. https://www.cnki.com.cn/Article/CJFDTOTAL-XYZL202215001.htm
[5] Toro A, Magazu' S, Fiorino L, et al. Port catheter tip positioning is essential[J]. Langenbecks Arch Surg, 2022, 407(3): 1311-1312. doi: 10.1007/s00423-022-02506-8
[6] 陈磊, 王琦, 谢栋栋, 等. 腹腔镜前列腺癌根治术中采用膀胱颈口荷包缝合联合尿道周围组织重建的早期尿控效果[J]. 中国微创外科杂志, 2022, 22(9): 752-756. doi: 10.3969/j.issn.1009-6604.2022.09.013
[7] Ellahi A, Stewart F, Kidd EA, et al. Strategies for the removal of short-term indwelling urethral catheters in adults[J]. Cochrane Database Syst Rev, 2021, 6(6): CD004011.
[8] 傅阳阳, 王雪静, 史又文, 等. 经腹腔镜下前列腺癌根治术后老年患者并发尿路感染的危险因素分析[J]. 老年医学与保健, 2022, 28(2): 349-352, 365. https://www.cnki.com.cn/Article/CJFDTOTAL-LYBJ202202027.htm
[9] 尚红, 王毓三, 申子瑜. 全国临床检验操作规程[M]. 4版. 北京: 人民卫生出版社, 2015.
[10] Copeland MM. American Joint Committee on Cancer Staging and end results reporting. Objectives and progress[J]. Cancer, 1965, 18(12): 1637-1640. doi: 10.1002/1097-0142(196512)18:12<1637::AID-CNCR2820181218>3.0.CO;2-C
[11] 赵卫红, 王增利, 王明, 等. 肾盂及输尿管结石患者术后泌尿系统感染的病原菌、药敏实验及影响因素分析[J]. 贵州医药, 2022, 46(1): 117-118. https://www.cnki.com.cn/Article/CJFDTOTAL-GZYI202201063.htm
[12] Mangal S, Pho A, Arcia A, et al. Patient and family engagement in catheter-associated urinary tract infection(CAUTI)prevention: a systematic review[J]. Jt Comm J Qual Patient Saf, 2021, 47(9): 591-603.
[13] 高可, 马莉, 陈艳霞, 等. 宫颈癌术后导尿管相关尿路感染病原菌及其影响因素分析[J]. 中国病原生物学杂志, 2023, 18(9): 1074-1078. https://www.cnki.com.cn/Article/CJFDTOTAL-ZISC202309015.htm
[14] 徐小娟, 叶铁君, 余金涣. 高龄剖宫产产妇导尿管相关尿路感染的影响因素与病原菌分布[J]. 中国消毒学杂志, 2021, 38(9): 660-662, 666. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGXD202109007.htm
[15] 陈景强, 赵沨. 经尿道前列腺切除术后尿路感染的危险因素及病原菌分布[J]. 中国感染控制杂志, 2020, 19(8): 752-757. https://www.cnki.com.cn/Article/CJFDTOTAL-GRKZ202008017.htm
[16] Rubi H, Mudey G, Kunjalwar R. Catheter-associated urinary tract infection(CAUTI)[J]. Cureus, 2022, 14(10): e30385.
[17] 张伟, 张娟娟, 任艳利, 等. 导尿管相关尿路感染的病原菌分布及危险因素分析[J]. 中国消毒学杂志, 2019, 36(7): 532-534. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGXD201907018.htm
-




 下载:
下载: