Construction of a bladder cancer muscle invading prediction model based on MRI imaging radiomics
-
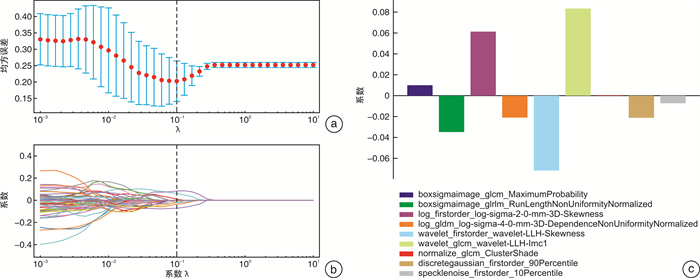
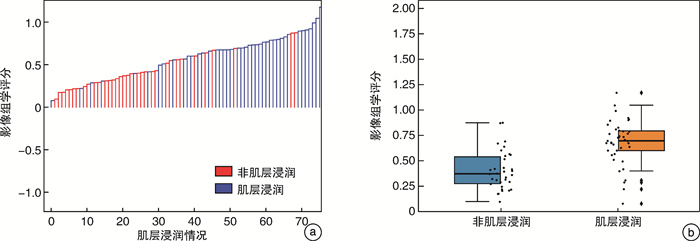
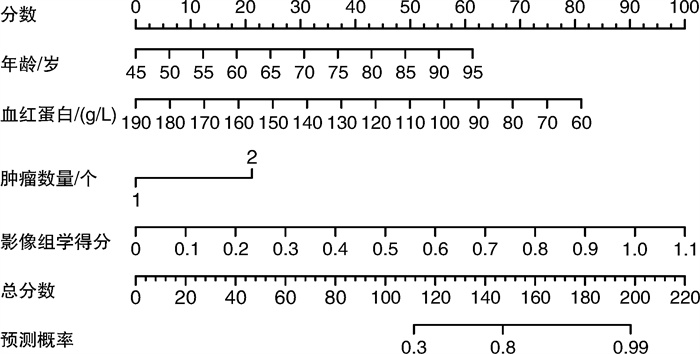
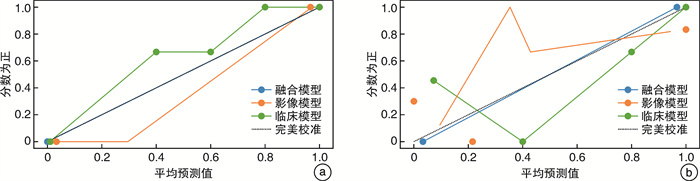
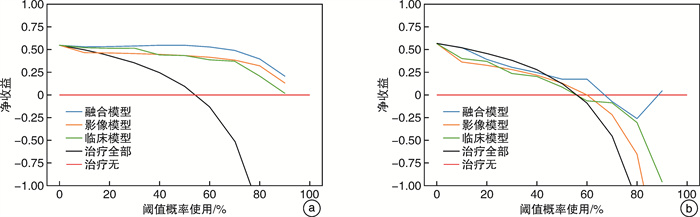
摘要: 目的 构建基于磁共振成像(magnetic resonance imaging,MRI)技术的影像组学特征及临床风险因素为基础的膀胱癌(bladder cancer,BCa)肌层浸润预测模型,用以术前准确且无创评估肿瘤肌层浸润情况。方法 本研究采用回顾性方法,汇集了76例接受根治性膀胱切除术(radical cystectomy,RC)的病例,所有患者术前30 d内均行3.0T MRI扫描,入院检查至手术日的等待期间不存在外来干预措施,且术后病理均证实为BC。在MRI诊断过程中,采取了T2加权成像(T2-weighted imaging,T2WI)和弥散加权成像(diffusion-weighted imaging,DWI)2种序列,研究者于每例患者的T2WI和相应的表观扩散系数图(apparent diffusion coefficient,ADC)上勾画出肿瘤最大占位区域,提取影像组学特征,并运用最小绝对收缩和选择算子(least absolute shrinkage and selection operator,LASSO)对特征进行筛选以达到降维目的。通过单因素与多因素分析同步进行,筛选出与肿瘤肌层侵袭有关的临床独立风险因素,进而共同创建影像组学与临床相关的列线图。结果 本次研究提取出影像组学特征属性共计2 286个。最终建立起的影像组学-临床融合模型指标包括影像组学特征10个和临床独立危险因子2个。曲线下面积(area under the curve,AUC)分别为0.97(训练集)和0.88(验证集),表现出良好的校准和鉴别能力。相比于单纯的影像组学模型和临床模型,影像组学-临床融合模型在校正曲线中更加贴合理想的预测情况(即贴合对角虚线代表的模型预测概率等同实际发生概率)。训练集和验证集在决策曲线中净收益值均高于全干预线和无干预线,具有更高的临床净效益和使用价值。结论 相较于单纯的影像组学或临床因素模型,将两者结合的融合模型在膀胱癌肌层浸润情况上表现出更好的预测效能,有助于术前对患者进行准确、无创的评估。Abstract: Objective Constructing a muscle invading prediction model for bladder cancer(BCa) based on radiomics attributes derived from magnetic resonance imaging(MRI) technology and clinical risk factors, aimed at preoperative, accurate, and non-invasive assessment of tumor muscle infiltration.Methods This retrospective study finally included 76 bladder cancer patients who underwent radical cystectomy(RC). All patients underwent 3.0T MRI scans within 30 days prior to surgery, with no external interventions between imaging and surgery, and postoperative pathology confirmed bladder cancer. MRI examinations included T2-weighted imaging(T2WI) and diffusion-weighted imaging(DWI) sequences. The researchers delineated the maximum tumor occupancy area on T2WI and the corresponding apparent diffusion coefficient(ADC) maps for each patient, from which radiomic features were extracted. Feature selection and dimensionality reduction were achieved using the least absolute shrinkage and selection operator(LASSO) method. Additionally, clinical risk factors associated with tumor muscle invasion were identified through univariate and multivariate analyses, and an integrated radiomic-clinical nomogram was constructed.Results In this study, a total of 2 286 radiomic features were extracted. Following selection, the radiomics-clinical model constructed with 10 radiomic features and 2 clinical risk factors exhibited excellent calibration and discrimination abilities, with area under the curve(AUC) of 0.97 and 0.88 in the training and validation sets, respectively. Compared to either the standalone radiomics or clinical models, the radiomics-clinical fusion model demonstrated a closer fit to the ideal prediction scenario on the calibration curve(i. e. alignment with the diagonal dashed line representing model prediction probability equivalent to actual occurrence probability). Both the training and validation sets showed higher net benefit values on the decision curve compared to either all or none intervention lines, indicating superior clinical net benefit and utility.Conclusion The predictive model that combines radiomics attributes with clinical risk factors further enhances predictive efficacy compared to models that rely solely on radiomics or clinical factors. It demonstrates good predictive utility for the muscle invading of bladder tumors, aiding in the preoperative, accurate, and non-invasive assessment of bladder cancer.
-
Key words:
- bladder cancer /
- magnetic resonance imaging /
- radiomics /
- muscle-invasive status /
- nomogram
-

-
表 1 2组患者临床基线资料比较
例(%),X±S 项目 训练集(53例) 验证集(23例) P值 性别 0.365 男 44(83.0) 17(73.9) 女 9(17.0) 6(26.1) 年龄/岁 69.7±10.3 67.6±12.6 0.484 BMI/(kg/m2) 22.7±3.3 23.1±2.4 0.536 血糖/(mmol/L) 5.7±1.4 5.5±1.3 0.545 甘油三酯/(mmol/L) 1.4±0.8 1.2±0.5 0.199 总胆固醇/(mmol/L) 4.3±1.0 4.1±0.9 0.426 HDL/(mmol/L) 1.1±0.3 1.2±0.3 0.051 LDL/(mmol/L) 2.6±0.8 2.4±0.7 0.243 血红蛋白/(g/L) 117.2±22.1 117.8±26.0 0.914 白蛋白/(g/L) 39.9±3.6 40.0±5.9 0.922 NLR 4.0±3.4 4.7±3.9 0.470 PLR 180.0±92.2 172.5±77.5 0.715 HDL:高密度脂蛋白;LDL:低密度脂蛋白;NLR:中性粒细胞与淋巴细胞计数比值;PLR:血小板与淋巴细胞计数比值。 表 2 临床风险因素单因素及多因素分析
因素 单因素分析 多因素分析 OR 95%置信区间 P值 OR 95%置信区间 P值 下限 上限 下限 上限 性别 1.92 0.49 7.57 0.349 年龄 1.08 1.02 1.14 0.010 0.0100 0.0038 0.0223 0.008 BMI 0.97 0.81 1.16 0.761 血糖 0.96 0.67 1.40 0.847 甘油三酯 0.70 0.31 1.56 0.380 总胆固醇 0.61 0.33 1.12 0.109 HDL 0.25 0.04 1.62 0.145 LDL 0.64 0.31 1.34 0.235 血红蛋白 0.95 0.91 0.98 0.004 -0.0100 -0.0133 -0.0024 0.007 白蛋白 0.83 0.71 0.96 0.013 0.0004 -0.0825 0.0248 0.892 NLR 1.03 0.90 1.19 0.645 PLR 1.00 1.00 1.01 0.167 肿瘤最大截面 1.02 0.99 1.05 0.226 肿瘤是否多发 1.56 0.52 4.68 0.012 0.2000 -0.0097 0.4068 0.048 表 3 融合模型与VI-RADS评分预测结果比较
例 组别 VI-RADS评分 融合模型 高风险 低风险 高风险 低风险 肌层浸润(41例) 37 4 40 1 非肌层浸润(35例) 23 12 24 9 P值 0.001 -
[1] Antoni S, Ferlay J, Soerjomataram I, et al. Bladder cancer incidence and mortality: a global overview and recent trends[J]. Eur Urol, 2017, 71(1): 96-108. doi: 10.1016/j.eururo.2016.06.010
[2] Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries[J]. CA Cancer J Clin, 2021, 71(3): 209-249. doi: 10.3322/caac.21660
[3] Powles T, Bellmunt J, Comperat E, et al. Bladder cancer: ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up[J]. Ann Oncol, 2022, 33(3): 244-258. doi: 10.1016/j.annonc.2021.11.012
[4] Funt SA, Rosenberg JE. Systemic, perioperative management of muscle-invasive bladder cancer and future horizons[J]. Nat Rev Clin Oncol, 2017, 14(4): 221-234. doi: 10.1038/nrclinonc.2016.188
[5] Panebianco V, Narumi Y, Altun E, et al. Multiparametric magnetic resonance imaging for bladder cancer: development of VI-RADS(vesical imaging-reporting and data system)[J]. Eur Urol, 2018, 74(3): 294-306. doi: 10.1016/j.eururo.2018.04.029
[6] Babjuk M, Böhle A, Burger M, et al. EAU guidelines on non-muscle-invasive urothelial carcinoma of the bladder: update 2016[J]. Eur Urol, 2017, 71(3): 447-461. doi: 10.1016/j.eururo.2016.05.041
[7] Karakiewicz PI, Shariat SF, Palapattu GS, et al. Precystectomy nomogram for prediction of advanced bladder cancer stage[J]. Eur Urol, 2006, 50(6): 1254-1260;discussion 1261-1262.
[8] Shariat SF, Palapattu GS, Karakiewicz PI, et al. Discrepancy between clinical and pathologic stage: impact on prognosis after radical cystectomy[J]. Eur Urol, 2007, 51(1): 137-149;discussion 149-151.
[9] Svatek RS, Shariat SF, Novara G, et al. Discrepancy between clinical and pathological stage: external validation of the impact on prognosis in an international radical cystectomy cohort[J]. BJU Int, 2011, 107(6): 898-904. doi: 10.1111/j.1464-410X.2010.09628.x
[10] Huang L, Kong QC, Liu ZZ, et al. The diagnostic value of MR imaging in differentiating T staging of bladder cancer: a meta-analysis[J]. Radiology, 2018, 286(2): 502-511. doi: 10.1148/radiol.2017171028
[11] van der Pol CB, Chung A, Lim C, et al. Update on multiparametric MRI of urinary bladder cancer[J]. J Magn Reson Imaging, 2018, 48(4): 882-896. doi: 10.1002/jmri.26294
[12] Wang HJ, Pui MH, Guan J, et al. Comparison of early submucosal enhancement and tumor stalk in staging bladder urothelial carcinoma[J]. AJR Am J Roentgenol, 2016, 207(4): 797-803. doi: 10.2214/AJR.16.16283
[13] Daneshmand S, Ahmadi H, Huynh LN, et al. Preoperative staging of invasive bladder cancer with dynamic gadolinium-enhanced magnetic resonance imaging: results from a prospective study[J]. Urology, 2012, 80(6): 1313-1318. doi: 10.1016/j.urology.2012.07.056
[14] Rosenkrantz AB, Haghighi M, Horn J, et al. Utility of quantitative MRI metrics for assessment of stage and grade of urothelial carcinoma of the bladder: preliminary results[J]. AJR Am J Roentgenol, 2013, 201(6): 1254-1259. doi: 10.2214/AJR.12.10348
[15] Wang HJ, Xu XP, Zhang X, et al. Elaboration of a multisequence MRI-based radiomics signature for the preoperative prediction of the muscle-invasive status of bladder cancer: a double-center study[J]. Eur Radiol, 2020, 30(9): 4816-4827. doi: 10.1007/s00330-020-06796-8
[16] Li LC, Zhang J, Zhe X, et al. An MRI-based radiomics nomogram in predicting histologic grade of non-muscle-invasive bladder cancer[J]. Front Oncol, 2023, 13: 1025972. doi: 10.3389/fonc.2023.1025972
[17] Zhang XX, Wang YC, Zhang J, et al. Development of a MRI-based radiomics nomogram for prediction of response of patients with muscle-invasive bladder cancer to neoadjuvant chemotherapy[J]. Front Oncol, 2022, 12: 878499. doi: 10.3389/fonc.2022.878499
[18] Zheng ZT, Xu FJ, Gu ZR, et al. Combining multiparametric MRI radiomics signature with the vesical imaging-reporting and data system(VI-RADS)score to preoperatively differentiate muscle invasion of bladder cancer[J]. Front Oncol, 2021, 11: 619893. doi: 10.3389/fonc.2021.619893
[19] Ueno Y, Takeuchi M, Tamada T, et al. Diagnostic accuracy and interobserver agreement for the vesical imaging-reporting and data system for muscle-invasive bladder cancer: a multireader validation study[J]. Eur Urol, 2019, 76(1): 54-56. doi: 10.1016/j.eururo.2019.03.012
[20] Lambin P, Leijenaar RTH, Deist TM, et al. Radiomics: the bridge between medical imaging and personalized medicine[J]. Nat Rev Clin Oncol, 2017, 14(12): 749-762. doi: 10.1038/nrclinonc.2017.141
[21] Wu SX, Zheng JJ, Li Y, et al. A radiomics nomogram for the preoperative prediction of lymph node metastasis in bladder cancer[J]. Clin Cancer Res, 2017, 23(22): 6904-6911. doi: 10.1158/1078-0432.CCR-17-1510
[22] Wu SX, Zheng JJ, Li Y, et al. Development and validation of an MRI-based radiomics signature for the preoperative prediction of lymph node metastasis in bladder cancer[J]. EBioMedicine, 2018, 34: 76-84. doi: 10.1016/j.ebiom.2018.07.029
[23] Cha KH, Hadjiiski L, Chan HP, et al. Bladder cancer treatment response assessment in CT using radiomics with deep-learning[J]. Sci Rep, 2017, 7(1): 8738. doi: 10.1038/s41598-017-09315-w
[24] Witjes JA, Bruins HM, Cathomas R, et al. European association of urology guidelines on muscle-invasive and metastatic bladder cancer: summary of the 2020 guidelines[J]. Eur Urol, 2021, 79(1): 82-104. doi: 10.1016/j.eururo.2020.03.055
[25] Kim TY, Cho NH, Jeong GB, et al. 3D texture analysis in renal cell carcinoma tissue image grading[J]. Comput Math MethodsMed, 2014, 2014: 536217.
[26] Zhou Y, Zhou GF, Zhang JL, et al. Radiomics signature on dynamic contrast-enhanced MR images: a potential imaging biomarker for prediction of microvascular invasion in mass-forming intrahepatic cholangiocarcinoma[J]. Eur Radiol, 2021, 31(9): 6846-6855. doi: 10.1007/s00330-021-07793-1
[27] Bhattacharjee S, Kim CH, Park HG, et al. Multi-features classification of prostate carcinoma observed in histological sections: analysis of wavelet-based texture and colour features[J]. Cancers, 2019, 11(12): 1937. doi: 10.3390/cancers11121937
[28] Xu XP, Liu Y, Zhang X, et al. Preoperative prediction of muscular invasiveness of bladder cancer with radiomic features on conventional MRI and its high-order derivative maps[J]. Abdom Radiol, 2017, 42(7): 1896-1905. doi: 10.1007/s00261-017-1079-6
[29] Tong YB, Udupa JK, Wang C, et al. Radiomics-guided therapy for bladder cancer: Using an optimal biomarker approach to determine extent of bladder cancer invasion from t2-weighted magnetic resonance images[J]. Adv Radiat Oncol, 2018, 3(3): 331-338. doi: 10.1016/j.adro.2018.04.011
[30] Xu XP, Zhang X, Tian Q, et al. Quantitative identification of nonmuscle-invasive and muscle-invasive bladder carcinomas: a multiparametric MRI radiomics analysis[J]. J Magn Reson Imaging, 2019, 49(5): 1489-1498. doi: 10.1002/jmri.26327
[31] Zheng JJ, Kong JQ, Wu SX, et al. Development of a noninvasive tool to preoperatively evaluate the muscular invasiveness of bladder cancer using a radiomics approach[J]. Cancer, 2019, 125(24): 4388-4398. doi: 10.1002/cncr.32490
[32] Xu SS, Yao QY, Liu GQ, et al. Combining DWI radiomics features with transurethral resection promotes the differentiation between muscle-invasive bladder cancer and non-muscle-invasive bladder cancer[J]. Eur Radiol, 2020, 30(3): 1804-1812. doi: 10.1007/s00330-019-06484-2
[33] Hammouda K, Khalifa F, Soliman A, et al. A multiparametric MRI-based CAD system for accurate diagnosis of bladder cancer staging[J]. Comput Med Imaging Graph, 2021, 90: 101911. doi: 10.1016/j.compmedimag.2021.101911
[34] Teleka S, Häggström C, Nagel G, et al. Risk of bladder cancer by disease severity in relation to metabolic factors and smoking: a prospective pooled cohort study of 800, 000 men and women[J]. Int J Cancer, 2018, 143(12): 3071-3082. doi: 10.1002/ijc.31597
[35] Huang XX, Pan T, Yan LL, et al. The inflammatory microenvironment and the urinary microbiome in the initiation and progression of bladder cancer[J]. Genes Dis, 2021, 8(6): 781-797. doi: 10.1016/j.gendis.2020.10.002
[36] Zhou Q, Zhang ZY, Ang XJ, et al. A nomogram combined with radiomics features, albuminuria, and metabolic syndrome to predict the risk of myometrial invasion of bladder cancer[J]. Transl Cancer Res, 2021, 10(7): 3177-3191. doi: 10.21037/tcr-21-426
-





 下载:
下载: