-
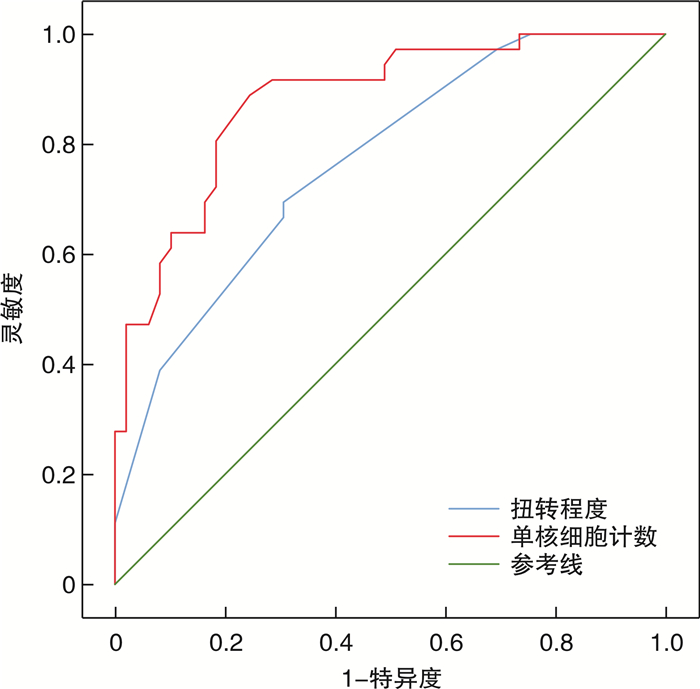
摘要: 目的 探讨单核细胞计数在预测儿童睾丸扭转睾丸存活的价值,并分析其他血液学标志物如平均血小板体积(mean platelet volume,MPV)、中性粒细胞与淋巴细胞比值(neutrophil-to-lymphocyte ratio,NLR)和血小板与淋巴细胞比值(platelet-to-lymphocyte ratio,PLR)的预测能力。方法 回顾性分析2016年12月—2024年3月在江南大学附属儿童医院接受紧急睾丸扭转手术的85例患儿的临床资料。采用独立样本t检验、多因素logistic回归分析和受试者工作特征(receiver operating characteristic,ROC)曲线及其曲线下面积(area under the curve,AUC)分析评估包括单核细胞计数、MPV、NLR和PLR在内的血液学参数的预测准确性。结果 患儿根据手术方式分为睾丸切除组(36例)和睾丸固定组(49例),平均年龄分别为(120.27 ± 59.60)个月和(139.06 ± 38.60)个月。2组的症状持续时间和睾丸的扭转程度比较差异均有统计学意义(P<0.05)。单核细胞计数与睾丸切除显著相关(OR=350.18,P=0.018),最佳截断值为0.59×109/L(AUC=0.880)。扭转程度也是关键预测因素(OR=1.006,P=0.029),最佳截断值为420°(AUC=0.767)。相比之下,MPV、NLR和PLR的预测可靠性不足。结论 单核细胞计数是预测儿童睾丸扭转患者是否需要睾丸切除的可靠生物标志物,尤其在结合扭转程度时。MPV、NLR和PLR在此方面的实用性有限,建议重新评估这些指标在预测睾丸存活方面的作用。
-
关键词:
- 睾丸扭转 /
- 单核细胞计数 /
- 平均血小板体积 /
- 中性粒细胞与淋巴细胞比值 /
- 血小板与淋巴细胞比值 /
- 儿童
Abstract: Objective To investigate the predictive value of monocyte counts for testicular survival outcomes in pediatric patients with testicular torsion, alongside other hematological markers such as mean platelet volume(MPV), neutrophil-to-lymphocyte ratio(NLR), and platelet-to-lymphocyte ratio(PLR).Methods Data from 85 pediatric patients undergoing emergency testicular torsion surgery at Affiliated Children's Hospital of Jiangnan University from December 2016 to March 2024 were retrospectively analyzed.The study utilized multivariate logistic regression and receiver operating characteristic(ROC) curve and area under the curve(AUC) analyses to assess the predictive accuracy of hematological parameters including monocyte counts, MPV, NLR, and PLR.Results The study divided patients into orchiectomy(n=36, mean age 120.27±59.60 months) and orchiopexy(n=49, mean age 139.06±38.60 months) groups. Symptom duration significantly differed, correlating with the severity of torsion. Monocyte counts showed a significant association with orchiectomy, with an OR of 350.18(P=0.018) and an optimal threshold of 0.59×109/L(AUC=0.880). The degree of torsion was also a critical predictor, with an OR of 1.006 per degree increase(P=0.029), and an optimal threshold of 420 degrees yielding an AUC of 0.77. Conversely, MPV, NLR, and PLR demonstrated inadequate predictive reliability with insufficient AUC values.Conclusion Monocyte count is a reliable biomarker for predicting the need for orchiectomy in pediatric testicular torsion, particularly when combined with the degree of torsion. The findings underscore the limited utility of MPV, NLR, and PLR in this clinical context, recommending their reevaluation in predicting testicular survival. -

-
表 1 睾丸切除组与睾丸固定组患儿临床资料比较
X±S 项目 合计(85例) 睾丸固定组(49例) 睾丸切除组(36例) t P值 年龄/月 131.10±49.18 139.06±38.60 120.27±59.60 1.654 0.104 症状持续时间/h 28.42±37.73 11.43±16.41 51.56±45.75 -5.030 < 0.001 扭转程度/° 465.18±207.31 380.20±162.53 580.83±207.49 -4.999 < 0.001 WBC/(×109/L) 11.45±2.83 10.58±2.71 12.63±2.56 -3.519 0.001 NEUT/(×109/L) 8.13±2.63 8.02±2.76 8.28±2.47 -0.445 0.657 单核细胞计数/(×109/L) 0.64±0.30 0.47±0.21 0.86±0.26 -7.612 < 0.001 LYM/(×109/L) 2.55±1.94 1.98±1.37 3.33±2.31 -3.135 0.003 PLT/(×109/L) 264.86±70.4 263.53±60.27 266.67±83.11 -0.202 0.841 PCT/% 0.27±0.07 0.26±0.06 0.28±0.08 -0.912 0.365 MPV/fL 10.22±1.23 9.98±1.09 10.54±1.35 -2.044 0.045 PDW/fL 15.13±1.97 15.31±1.70 14.88±2.30 0.932 0.355 NLR 5.14±4.07 6.29±4.76 3.57±2.08 3.569 0.001 PLR 150.03±99.37 184.77±111.16 102.75±52.59 4.521 < 0.001 CRP/(mg/L) 7.99±13.86 2.02±5.10 16.10±17.55 -4.670 < 0.001 表 2 睾丸扭转患儿睾丸切除的多因素logistic回归分析结果
变量 β SE Wals OR 95%CI P值 发病时间 0.026 7 0.017 2.460 1.027 0.993~1.060 0.117 扭转程度 0.005 9 0.003 4.784 1.006 1.001~1.011 0.029 WBC 0.057 8 0.291 0.039 1.060 0.599~1.866 0.842 单核细胞计数 5.858 5 2.470 5.624 350.185 2.760~49 012.231 0.018 LYM -0.073 1 0.362 0.041 0.930 0.457~1.891 0.840 MPV 0.392 3 0.338 1.346 1.480 0.763~2.868 0.246 NLR -0.168 4 0.479 0.124 0.845 0.332~2.162 0.725 PLR -0.001 5 0.017 0.008 0.999 0.966~1.032 0.930 CRP 0.042 0 0.052 0.657 1.043 0.941~1.153 0.418 表 3 各危险因素预测睾丸坏死的ROC曲线分析结果
变量 最佳截断值 AUC 敏感度/% 特异度/% 95%置信区间 发病时间 11.5 h 0.842 83.3 75.5 0.751~0.932 扭转程度 420° 0.767 69.4 69.4 0.668~0.866 WBC 11.16×109/L 0.707 77.8 61.2 0.595~0.819 单核细胞计数 0.59×109/L 0.880 88.9 75.5 0.808~0.952 LYM 1.89×109/L 0.732 72.2 67.3 0.628~0.837 MPV 10.95 fL 0.613 41.7 85.7 0.488~0.738 NLR 6.55 0.668 94.4 38.8 0.555~0.781 PLR 88.9 0.765 58.3 85.7 0.664~0.866 CRP 5.45 mg/L 0.806 66.7 91.8 0.701~0.910 -
[1] Minas A, Mahmoudabadi S, Gamchi NS, et al. Testicular torsion in vivo models: mechanisms and treatments[J]. Andrology, 2023, 11(7): 1267-1285. doi: 10.1111/andr.13418
[2] Delgado-Miguel C, García A, Muñoz-Serrano AJ, et al. The role of neutrophil-to-lymphocyte ratio as a predictor of testicular torsion in children[J]. J Pediatr Urol, 2022, 18(5): 697. e1-697. e6. doi: 10.1016/j.jpurol.2022.09.010
[3] Zhu J, Song YX, Chen GY, et al. Predictive value of haematologic parameters in diagnosis of testicular torsion: evidence from a systematic review and meta-analysis[J]. Andrologia, 2020, 52(2): e13490.
[4] Austermann J, Roth J, Barczyk-Kahlert K. The good and the bad: monocytes' and macrophages' diverse functions in inflammation[J]. Cells, 2022, 11(12): 1979. doi: 10.3390/cells11121979
[5] Yucel C, Ozlem Ilbey Y. Predictive value of hematological parameters in testicular torsion: retrospective investigation of data from a high-volume tertiary care center[J]. J Int Med Res, 2019, 47(2): 730-737. doi: 10.1177/0300060518809778
[6] Merder E, Bozkurt M, Ariman A, et al. Comprehensive examination of haematological parameters of patients operated due to testicular torsion[J]. Andrologia, 2020, 52(9): e13674.
[7] Chen PY, Huang WP, Liu L, et al. Predictive value of hematological parameters in testicular salvage: a 12-year retrospective review[J]. Front Pediatr, 2022, 10: 989112. doi: 10.3389/fped.2022.989112
[8] Bedel C, Korkut M. Evaluation of the neutrophil-lymphocyte ratio, platelet-lymphocyte ratio and monocyte lymphocyte ratio for diagnosis of testicular torsion[J]. J Acute Dis, 2020, 9(5): 213-217. doi: 10.4103/2221-6189.291286
[9] Dziedzic EA, Gąsior JS, Tuzimek A, et al. Blood count-derived inflammatory markers and acute complications of ischemic heart disease in elderly women[J]. J Clin Med, 2023, 12(4): 1369. doi: 10.3390/jcm12041369
[10] Lee HY, Lim DG, Chung HS, et al. Mean platelet volume is the most valuable hematologic parameter in differentiating testicular torsion from epididymitis within the golden time[J]. Transl Androl Urol, 2022, 11(9): 1282-1291. doi: 10.21037/tau-21-1112
[11] Barkai E, Dekalo S, Yossepowitch O, et al. Complete blood count markers and C-reactive protein as predictors of testicular viability in the event of testicular torsion in adults[J]. Urol Int, 2023, 107(8): 801-806. doi: 10.1159/000531145
[12] Adawi EA, Ghanem MA, Ghanem AM, et al. High platelet distribution width can independently predict testicular survival in testicular torsion among patients with steady-state sickle cell anemia[J]. World J Pediatr Surg, 2022, 5(1): e000358. doi: 10.1136/wjps-2021-000358
[13] He M, Zhang WP, Sun N. Can haematologic parameters be used to predict testicular viability in testicular torsion?[J]. Andrologia, 2019, 51(9): e13357.
[14] Jang JB, Ko YH, Choi JY, et al. Neutrophil-lymphocyte ratio predicts organ salvage in testicular torsion with marginal diagnostic delay[J]. World J Mens Health, 2019, 37(1): 99-104. doi: 10.5534/wjmh.180049
[15] Greear GM, Romano MF, Katz MH, et al. Testicular torsion: epidemiological risk factors for orchiectomy in pediatric and adult patients[J]. Int J Impot Res, 2021, 33(2): 184-190. doi: 10.1038/s41443-020-0331-8
[16] Seizilles de Mazancourt E, Khene Z, Sbizerra M, et al. Cut-off time for surgery and prediction of orchiectomy in spermatic cord torsion: a retrospective multicentric study over 15 years[J]. World J Urol, 2023, 41(12): 3789-3794. doi: 10.1007/s00345-023-04671-x
[17] Steeman A, Ngatchou W, Ramadan AS, et al. Impact of treatment delays on outcome of acute testicular torsion: a 15-year retrospective study[J]. Acta Chir Belg, 2022, 122(2): 116-122. doi: 10.1080/00015458.2021.1883391
-

| 引用本文: | 吴航, 杨越, 李国根, 等. 儿童睾丸扭转中单核细胞计数的睾丸活性预测价值[J]. 临床泌尿外科杂志, 2024, 39(10): 904-908. doi: 10.13201/j.issn.1001-1420.2024.10.012 |
| Citation: | WU Hang, YANG Yue, LI Guogen, et al. Predictive value of monocyte counts in pediatric testicular torsion outcomes[J]. J Clin Urol, 2024, 39(10): 904-908. doi: 10.13201/j.issn.1001-1420.2024.10.012 |
- Figure 1.



 下载:
下载: