-
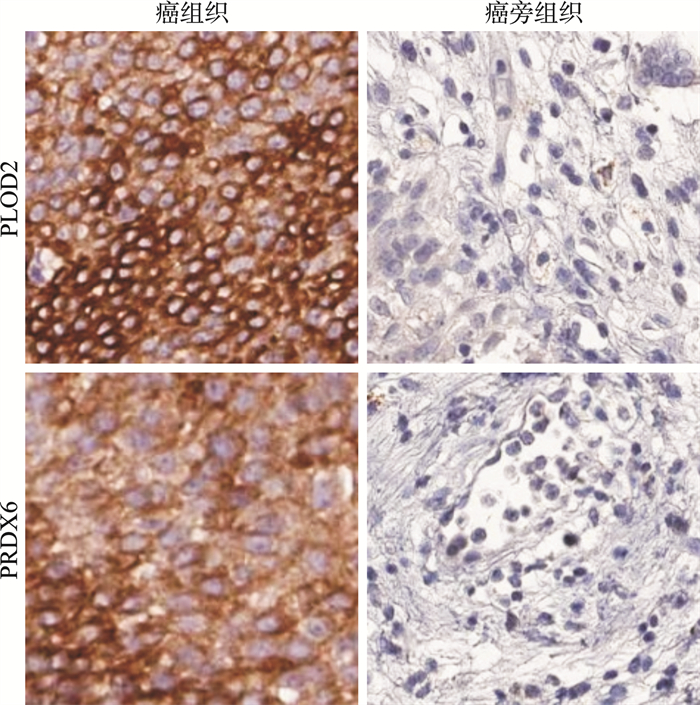
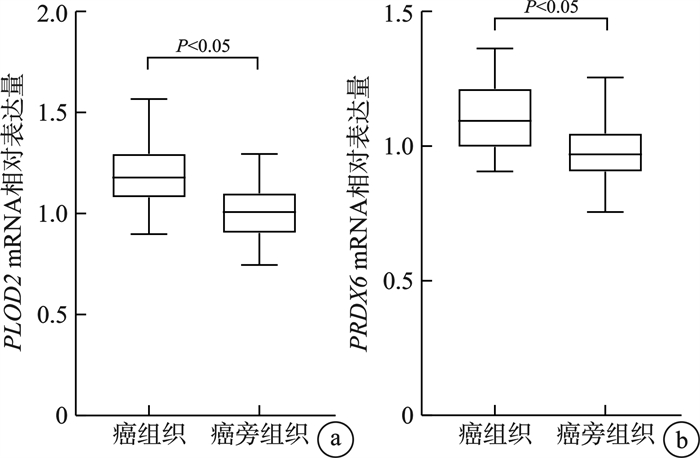
摘要: 目的 探讨膀胱癌组织中赖氨酸羟化酶2(procollagen-lysine 2-oxoglutarate 5-dioxygenase 2,PLOD2)、过氧化物氧化还原蛋白6(peroxiredoxin-6,PRDX6)的表达水平及其临床意义。方法 选择2017年9月—2020年8月邯郸市第一医院收治的113例膀胱癌患者作为研究对象;采用实时荧光定量PCR(qRT-PCR)法检测PLOD 2、PRDX6mRNA的相对表达量;采用免疫组织化学染色法测定PLOD2、PRDX6蛋白表达;膀胱癌组织中PLOD2、PRDX6表达与膀胱癌患者预后的关系采用Kaplan-Meier生存曲线分析;膀胱癌患者预后的影响因素采用Cox回归分析。结果 膀胱癌组织中PLOD2 mRNA、PRDX6 mRNA表达水平以及PLOD2、PRDX6阳性表达率均显著高于癌旁组织(P < 0.05)。膀胱癌患者TNM分期为Ⅲ~Ⅳ期、肿瘤分化程度为低分化、浸润深度为肌层浸润的PLOD2、PRDX6蛋白阳性表达率显著高于TNM分期为Ⅰ~Ⅱ期、肿瘤分化程度为高、中分化、浸润深度为非肌层浸润(P < 0.05)。PLOD2阳性表达患者3年无病生存率显著低于PLOD2阴性表达患者(63.64% vs 85.11%,χ2=7.093,P=0.008);PRDX6阳性表达患者3年无病生存率显著低于PRDX6阴性表达患者(65.08% vs 82.00%,χ2=4.756,P=0.029)。TNM分期为Ⅲ~Ⅳ期、肌层浸润、肿瘤低分化以及PLOD2和PRDX6阳性表达是影响膀胱癌患者预后的危险因素(P < 0.05)。结论 膀胱癌组织中PLOD2、PRDX6表达异常上升,二者与TNM分期、浸润深度、肿瘤分化程度有关,可作为膀胱癌预后相关的肿瘤标志物。
-
关键词:
- 膀胱癌 /
- 赖氨酸羟化酶2 /
- 过氧化物氧化还原蛋白6 /
- 预后
Abstract: Objective To investigate the expressions of procollagen-lysine 2-oxoglutarate 5-dioxygenase 2(PLOD2) and peroxiredoxin-6(PRDX6) in bladder cancer and their clinical significance.Methods From September 2017 to August 2020, 113 patients with bladder cancer admitted to our hospital were collected as the study subjects. The relative expressions of PLOD 2 and PRDX 6 mRNA were assayed by real-time fluorescence quantitative PCR (qRT-PCR), and immunohistochemical staining was applied to determine the expressions of PLOD2 and PRDX6 proteins. The relationship between PLOD2, PRDX6 expressions in bladder cancer tissues and the prognosis of bladder cancer patients was analyzed by Kaplan-Meier survival curve, and the prognostic factors of bladder cancer patients were analyzed by Cox regression.Results The expression levels of PLOD 2 mRNA and PRDX 6 mRNA and the positive expression rates of PLOD2 and PRDX6 in bladder cancer tissues were significantly higher than those in paracancer tissues(P < 0.05). The positive expression rates of PLOD2 and PRDX6 in bladder cancer patients with TNM stage Ⅲ-Ⅳ, low differentiation and invasion depth of muscle invasion were significantly higher than those with TNM stage Ⅰ-Ⅱ, high/moderate differentiation and invasion depth of non-muscle invasion(P < 0.05). The 3-year disease-free survival rate of PLOD2 positive expression patients was obviously lower than that of PLOD2 negative expression patients(63.64% vs 85.11%, χ2=7.093, P=0.008), and the 3-year disease-free survival rate of PRDX6 positive expression patients was obviously lower than that of PRDX6 negative expression patients(65.08% vs 82.00%, χ2=4.756, P=0.029). Cox regression analysis showed that TNM stage Ⅲ-Ⅳ, muscular invasion, tumor low differentiation, and the positive expressions of PLOD2 and PRDX6 were the risk factors affecting the prognosis of bladder cancer patients(P < 0.05).Conclusion The abnormal increased expressions of PLOD2 and PRDX6 in bladder cancer and their relationship with TNM stage, depth of invasion and tumor differentiation can be used as tumor markers related to the prognosis of bladder cancer. -

-
表 1 PLOD2、PRDX6蛋白表达与临床病理特征的关系
例(%) 项目 例数 PLOD2阳性表达(66例) χ2 P值 PRDX6阳性表达(63例) χ2 P值 性别 0.513 0.474 0.599 0.439 男 81 49(74.24) 47(74.60) 女 32 17(25.76) 16(25.40) 年龄/岁 0.184 0.668 1.927 0.165 ≤60 55 31(46.97) 27(42.86) >60 58 35(53.03) 36(57.14) BMI/(kg/m2) 0.160 0.689 2.638 0.104 ≤23 65 39(59.09) 32(50.79) >23 48 27(40.91) 31(49.21) 吸烟 3.575 0.059 0.062 0.803 无 46 22(33.33) 25(39.68) 有 67 44(66.67) 38(60.32) 肿瘤最大直径/cm 0.020 0.887 0.142 0.706 ≤3 52 30(45.45) 28(44.44) >3 61 36(54.55) 35(55.56) TNM分期 20.566 < 0.001 15.341 < 0.001 Ⅰ~Ⅱ期 58 22(33.33) 22(34.92) Ⅲ~Ⅳ期 55 44(66.67) 41(65.08) 肿瘤分化程度 11.193 0.004 10.316 0.006 高分化 32 13(19.70) 13(20.63) 中分化 43 23(34.85) 21(33.33) 低分化 38 30(45.45)1)2) 29(46.03)1)2) 浸润深度 5.344 0.021 15.734 < 0.001 非肌层浸润 60 29(43.94) 23(36.51) 肌层浸润 53 37(56.06) 40(63.49) 淋巴结转移 2.846 0.092 3.201 0.074 无 64 33(50.00) 31(49.21) 有 49 33(50.00) 32(50.79) 与高分化比较,1)P < 0.05;与中分化比较,2)P < 0.05。 表 2 Cox回归分析赋值表
变量 赋值 性别 男=1,女=0 年龄 >60岁=1,≤60岁=0 BMI >23 kg/m2=1,≤23 kg/m2=0 吸烟 有=1,无=0 肿瘤最大直径 >3 cm=1,≤3 cm=0 TNM分期 Ⅲ~Ⅳ期=1,Ⅰ~Ⅱ期=0 肿瘤分化程度 低分化=1,高、中分化=0 浸润深度 肌层浸润=1,非肌层浸润=0 淋巴结转移 有=1,无=0 PLOD2 阳性表达=1,阴性表达=0 PRDX6 阳性表达=1,阴性表达=0 表 3 单因素Cox回归分析影响膀胱癌患者预后的因素
影响因素 β SE Wald χ2 P值 HR 95%CI 性别 1.242 0.735 2.853 0.091 3.461 0.820~14.617 年龄 0.960 0.674 2.029 0.154 2.612 0.697~9.788 BMI 1.140 0.841 1.839 0.175 3.128 0.602~16.261 吸烟 1.160 0.598 3.763 0.052 3.190 0.988~10.300 肿瘤最大直径 0.841 0.762 1.218 0.270 2.319 0.521~10.326 TNM分期 1.801 0.455 15.674 < 0.001 6.058 2.483~14.779 肿瘤分化程度 1.739 0.523 11.061 0.001 5.694 2.043~15.871 浸润深度 0.988 0.439 5.066 0.024 2.686 1.136~6.350 淋巴结转移 1.106 0.570 3.767 0.052 3.023 0.989~9.239 PLOD2 1.827 0.387 22.286 < 0.001 6.215 2.911~13.270 PRDX6 1.702 0.416 16.747 < 0.001 5.487 2.428~12.401 表 4 多因素Cox回归分析影响膀胱癌患者预后的因素
影响因素 β SE Wald χ2 P值 HR 95%CI TNM分期 1.243 0.468 7.058 0.008 3.467 1.385~8.676 肿瘤分化程度 1.515 0.503 9.071 0.003 4.549 1.697~12.192 浸润深度 1.380 0.422 10.698 0.001 3.976 1.739~9.092 PLOD2 1.752 0.561 9.749 0.002 5.764 1.920~17.308 PRDX6 1.924 0.385 24.962 < 0.001 6.845 3.219~14.558 -
[1] Jubber I, Ong S, Bukavina L, et al. Epidemiology of bladder cancer in 2023: a systematic review of risk factors[J]. Eur Urol, 2023, 84(2): 176-190. doi: 10.1016/j.eururo.2023.03.029
[2] 邢金春, 赵仲杰, 刘正升. ADC药物联合免疫治疗在膀胱癌的应用[J]. 临床泌尿外科杂志, 2024, 39(9): 755-759.
[3] Witjes JA, Bruins HM, Cathomas R, et al. European association of urology guidelines on muscle-invasive and metastatic bladder cancer: summary of the 2020 guidelines[J]. Eur Urol, 2021, 79(1): 82-104. doi: 10.1016/j.eururo.2020.03.055
[4] Necula L, Matei L, Dragu D, et al. Collagen family as promising biomarkers and therapeutic targets in cancer[J]. Int J Mol Sci, 2022, 23(20): 12415. doi: 10.3390/ijms232012415
[5] Kreße N, Schröder H, Stein KP, et al. PLOD2 is a prognostic marker in glioblastoma that modulates the immune microenvironment and tumor progression[J]. Int J Mol Sci, 2022, 23(11): 6037. doi: 10.3390/ijms23116037
[6] Chang WH, Forde D, Lai AG. Dual prognostic role of 2-oxoglutarate-dependent oxygenases in ten cancer types: implications for cell cycle regulation and cell adhesion maintenance[J]. Cancer Commun, 2019, 39(1): 23. http://www.ncbi.nlm.nih.gov/pubmed/31036064
[7] Li KR, Niu Y, Li K, et al. Dysregulation of PLOD2 promotes tumor metastasis and invasion in hepatocellular carcinoma[J]. J Clin Transl Hepatol, 2023, 11(5): 1094-1105. http://www.semanticscholar.org/paper/274c8ec207842f0f16f7683d6c163df6e6d69c1c
[8] Kim JE, Park H, Kang TC. Peroxiredoxin 6 regulates glutathione peroxidase 1-medited glutamine synthase preservation in the hippocampus of chronic epilepsy rats[J]. Antioxidants(Basel), 2023, 12(1): 156.
[9] Sun JL, Yue WC, You JW, et al. Identification of a novel ferroptosis-related gene prognostic signature in bladder cancer[J]. Front Oncol, 2021, 11: 730716. doi: 10.3389/fonc.2021.730716
[10] Chen ZB, Chen DM, Song ZF, et al. Mapping the tumor microenvironment in bladder cancer and exploring the prognostic genes by single-cell RNA sequencing[J]. Front Oncol, 2022, 12: 1105026.
[11] Yang L, Fan XX, Zhou C, et al. Construction and validation of a novel ferroptosis-related prognostic signature for lung adenocarcinoma[J]. Transl Lung Cancer Res, 2023, 12(8): 1766-1781. doi: 10.21037/tlcr-23-351
[12] Ying YD, Wang ZW, Tan YX, et al. Identification and validation of immunohistochemical marker panels to predict the prognosis of muscle invasive bladder cancer[J]. Transl Androl Urol, 2023, 12(2): 176-186. doi: 10.21037/tau-22-538
[13] 周海鹏, 林天海, 张孟尼, 等. HER2在膀胱尿路上皮癌中的表达情况及临床意义[J]. 临床泌尿外科杂志, 2024, 39(9): 769-776. https://lcmw.whuhzzs.com/article/doi/10.13201/j.issn.1001-1420.2024.09.004
[14] Xu N, Yao ZM, Shang GG, et al. Integrated proteogenomic characterization of urothelial carcinoma of the bladder[J]. J Hematol Oncol, 2022, 15(1): 76. doi: 10.1186/s13045-022-01291-7
[15] Murakami K, Furuya H, Hokutan K, et al. Association of SNPs in the PAI1 gene with disease recurrence and clinical outcome in bladder cancer[J]. Int J Mol Sci, 2023, 24(5): 4943. doi: 10.3390/ijms24054943
[16] Maghsoud Y, Vázquez-Montelongo EA, Yang XD, et al. Computational investigation of a series of small molecules as potential compounds for lysyl hydroxylase-2(LH2) inhibition[J]. J Chem Inf Model, 2023, 63(3): 986-1001. doi: 10.1021/acs.jcim.2c01448
[17] Gong XM, Wang AL, Song WQ. Clinicopathological significances of PLOD2, epithelial-mesenchymal transition markers, and cancer stem cells in patients with esophageal squamous cell carcinoma[J]. Medicine(Baltimore), 2022, 101(34): e30112.
[18] Shao YK, Xu KL, Zheng X, et al. Proteomics profiling of colorectal cancer progression identifies PLOD2 as a potential therapeutic target[J]. Cancer Commun, 2022, 42(2): 164-169. doi: 10.1002/cac2.12240
[19] Lan JW, Zhang SJ, Zheng L, et al. PLOD2 promotes colorectal cancer progression by stabilizing USP15 to activate the AKT/mTOR signaling pathway[J]. Cancer Sci, 2023, 114(8): 3190-3202. doi: 10.1111/cas.15851
[20] Wang Z, Fan GT, Zhu H, et al. PLOD2 high expression associates with immune infiltration and facilitates cancer progression in osteosarcoma[J]. Front Oncol, 2022, 12: 980390. doi: 10.3389/fonc.2022.980390
[21] Sato K, Parag-Sharma K, Terajima M, et al. Lysyl hydroxylase 2-induced collagen cross-link switching promotes metastasis in head and neck squamous cell carcinomas[J]. Neoplasia, 2021, 23(6): 594-606. doi: 10.1016/j.neo.2021.05.014
[22] Chae U, Kim B, Kim H, et al. Peroxiredoxin-6 regulates p38-mediated epithelial-mesenchymal transition in HCT116 colon cancer cells[J]. J Biol Res, 2021, 28(1): 22. http://www.socolar.com/Article/Index?aid=100091654231&jid=100000005000
[23] Di Sanzo M, Cozzolino F, Battaglia AM, et al. Ferritin heavy chain binds peroxiredoxin 6 and inhibits cell proliferation and migration[J]. Int J Mol Sci, 2022, 23(21): 12987. doi: 10.3390/ijms232112987
[24] Mu RH, Li YP, Xing JY, et al. Effect of lentivirus-mediated peroxiredoxins 6 gene silencing on the phenotype of human gastric cancer BGC-823 cells[J]. J Cancer Res Ther, 2022, 18(2): 411-417. doi: 10.4103/jcrt.jcrt_1083_21
-

计量
- 文章访问数: 77
- 施引文献: 0



 下载:
下载: