-
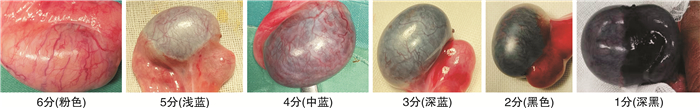
摘要: 目的 研究儿童睾丸扭转复位固定术后睾丸萎缩的危险因素,探讨预测睾丸萎缩的指标。方法 回顾性分析2018年1月—2022年12月河北省儿童医院收治的72例行睾丸扭转复位固定术患儿的临床资料,患儿年龄1~13岁,平均(7.31±0.32)岁;均为单侧,其中左侧43例,右侧29例。记录患儿的临床表现、术中睾丸颜色变化情况、实验室和超声检查结果,术后均随访6个月,依据术后超声结果将患儿分为睾丸萎缩组和非睾丸萎缩组,将2组患儿的资料进行单因素分析,并将其中差异有统计学意义的因素纳入多因素logistic回归模型,分析睾丸扭转复位后睾丸萎缩的危险因素。结果 72例患儿均行睾丸扭转复位固定术,其中术后睾丸萎缩39例,未发生睾丸萎缩33例,单因素分析结果显示术前疼痛持续时间、术前超声不均质表现、睾丸扭转复位10 min后颜色评分与睾丸扭转复位术后发生睾丸萎缩密切相关(P < 0.05)。年龄、阴囊红肿、术前血常规白细胞数值等因素与睾丸扭转复位术后发生睾丸萎缩无相关性(P>0.05)。多因素logistic回归分析结果显示,患儿术前疼痛持续时间>12 h、睾丸扭转复位后10 min颜色评分1~2分、术前超声睾丸实质不均质回声是儿童睾丸扭转复位固定术后发生睾丸萎缩的独立危险因素(P < 0.05)。结论 睾丸扭转复位10 min后颜色评分1~2分,睾丸已产生不可逆损伤,睾丸切除概率大,即使术中保留睾丸,术后发生睾丸萎缩概率高。术前疼痛持续时间>12 h、术前超声不均质表现是睾丸扭转复位术后发生睾丸萎缩的危险因素。当怀疑睾丸扭转时,应积极手术探查,减少睾丸缺血时间从而最大可能的保留睾丸。Abstract: Objective To study the risk factors of testicular atrophy after torsion reduction and fixation in children, and to explore the index of predicting testicular atrophy.Methods The clinical data of 72 children who underwent testicular torsion reduction and fixation in our hospital from January 2018 to December 2022 were retrospectively analyzed. The age ranged from 1 to 13 years, with an average age of (7.31±0.32) years. The patients were followed up for 6 months. According to the results of postoperative ultrasound, the patients were divided into testicular atrophy group and non-testicular atrophy group. The data of the two groups were analyzed by univariate analysis, and the factors with statistically significant differences were included in the multivariate logistic regression model. The risk factors of testicular atrophy after reduction of testicular torsion were analyzed.Results All the 72 children underwent testicular torsion reduction and fixation, among whom 39 cases had testicular atrophy after surgery, and 33 cases did not have testicular atrophy. Univariate analysis showed that there were no significant differences in age, scrotal redness and swelling, or preoperative white blood cell count between the two groups(P>0.05). There were significant differences in the duration of preoperative pain, the appearance of preoperative ultrasound heterogeneity, and the color score after 10 minutes of testicular torsion between the two groups(P < 0.05). Multivariate logistic regression analysis showed that the duration of preoperative pain >12 hours, color score of 1-2 at 10 minutes after reduction of testicular torsion, and the heterogeneous echo of testicular parenchyma on preoperative ultrasound were independent risk factors for testicular atrophy after reduction and fixation of testicular torsion in children(P < 0.05).Conclusion The color score of 1-2 at 10 minutes after reduction of testicular torsion indicates that the testis has been irreversibly damaged, and the probability of orchiectomy is high. Even if the testes are preserved during the operation, the rate of testicular atrophy is high. Preoperative pain duration >12 hours and preoperative ultrasound heterogeneity are risk factors for testicular atrophy after testicular torsion reduction. When testicular torsion is suspected, active surgical exploration should be performed to reduce the testicular ischemia time and thus maximize the possible preservation of the testis.
-
Key words:
- testicular torsion /
- testicular atrophy /
- risk factors /
- children
-

-
表 1 睾丸扭转复位固定术后睾丸萎缩单因素分析
例(%),X±S 因素 睾丸萎缩组
(39例)非睾丸萎缩组
(33例)P值 年龄/岁 6.75±0.13 8.27±0.68 >0.05 有无阴囊红肿 >0.05 有 25(64.10) 18(54.55) 无 14(35.90) 15(45.45) 血WBC>10×109/L >0.05 有 19(48.72) 16(48.48) 无 20(51.28) 17(51.52) 术前疼痛时间/ h <0.05 ≤12 13(33.33) 21(63.64) >12 26(66.67) 12(36.36) 术前超声不均质表现 <0.05 有 24(61.54) 11(33.33) 无 15(38.46) 22(66.67) 睾丸复位10 min后颜色评分/分 <0.05 1~2 37(94.87) 4(12.12) 3~6 2(5.13) 29(87.88) 表 2 睾丸扭转复位固定术后睾丸萎缩多因素分析
因素 Wald χ2 P值 OR 95%CI 术前疼痛时间>12 h 6.311 < 0.05 5.223 1.438~18.967 术前超声有不均质表现 6.347 < 0.05 2.195 1.191~4.045 睾丸复位10 min后颜色评分1~2分 9.566 < 0.05 4.047 1.669~9.815 -
[1] 钟海军, 沈剑, 张斌, 等. 儿童间歇性睾丸扭转的临床诊治分析[J]. 中华泌尿外科杂志, 2020, 41(7): 536-539. doi: 10.3760/cma.j.cn112330-20200316-00198
[2] 中华医学会男科学分会, 睾丸扭转诊断与治疗指南编写组. 睾丸扭转诊断与治疗指南[J]. 中华男科学杂志, 2022, 28(3): 252-261. https://www.cnki.com.cn/Article/CJFDTOTAL-NKXB202203010.htm
[3] 张明艳, 姜力. 睾丸扭转20例临床分析[J]. 国际泌尿系统杂志, 2020, 40(5): 900-901. doi: 10.3760/cma.j.cn431460-20190516-00037
[4] 邢民者, 齐灿. 儿童睾丸扭转早期临床诊治的多因素分析[J]. 河北医药, 2022, 44(13): 1989-1992. doi: 10.3969/j.issn.1002-7386.2022.13.016
[5] Jacobsen FM, Rudlang TM, Fode M, et al. The Impact of Testicular Torsion on Testicular Function[J]. World J Mens Health, 2020, 38(3): 298-307. doi: 10.5534/wjmh.190037
[6] 李骥, 张谦, 郭立华, 等. 儿童长时间睾丸扭转得以保留原因分析及对侧睾丸处理方式选择[J]. 中华实用儿科临床杂志, 2020, 35(21): 1659-1662.
[7] 李慕婕, 何梦, 谢向辉, 等. 睾丸扭转患儿平均血小板体积与睾丸活性的相关性[J]. 中华实用儿科临床杂志, 2022, 37(3): 191-195.
[8] 蒲九州, 刘帅, 李绪, 等. 睾丸扭转的研究进展[J]. 中华泌尿外科杂志, 2020, 41(4): 318-320. doi: 10.3760/cma.j.cn112330-20191215-00556
[9] 张兵, 王秀艳. 彩色多普勒超声对精索扭转早期诊断及扭转睾丸术后存活力预测的临床价值[J]. 外科研究与新技术, 2019, 8(2): 97-101, 105. https://www.cnki.com.cn/Article/CJFDTOTAL-TJYE201902009.htm
[10] 韦佳, 陈光杰, 高磊, 等. 以腹痛为首发症状的学龄儿童睾丸扭转的临床特点分析[J]. 中华急诊医学杂志, 2021, 30(6): 682-684.
[11] 陈炽炜, 刘昊, 王峻. 睾丸扭转误诊延诊9例[J]. 临床泌尿外科杂志, 2019, 34(4): 327-329. https://lcmw.whuhzzs.com/article/doi/10.13201/j.issn.1001-1420.2019.04.019
[12] 许云峰, 蒋海燕, 胡慧勇, 等. 高频彩超对小儿阴囊急症的诊断及鉴别诊断价值[J]. 中华男科学杂志, 2016, 22(11): 996-1000. https://www.cnki.com.cn/Article/CJFDTOTAL-NKXB201611009.htm
[13] 廖有刚, 龙建华, 申凯, 等. 睾丸扭转诊治的研究现状[J]. 临床泌尿外科杂志, 2019, 34(7): 578-581. https://lcmw.whuhzzs.com/article/doi/10.13201/j.issn.1001-1420.2019.07.020
[14] Jacobsen FM, Rudlang TM, Fode M, et al. The Impact of Testicular Torsion on Testicular Function[J]. World J Mens Health, 2020, 38(3): 298-307. doi: 10.5534/wjmh.190037
[15] 袁帅, 武进峰, 张雁钢. 血浆D-二聚体在预测扭转睾丸存活力中的价值[J]. 临床泌尿外科杂志, 2021, 36(1): 38-40, 45. https://lcmw.whuhzzs.com/article/doi/10.13201/j.issn.1001-1420.2021.01.008
[16] Sessions AE, Rabinowitz R, Hulbert WC, et al. Testicular torsion: direction, degree, duration and disinformation[J]. J Urol, 2003, 169(2): 663-665. doi: 10.1016/S0022-5347(05)63987-0
[17] Cimador M, DiPace MR, Castagnetti M, et al. Predictors of testicular viability in testicular torsion[J]. J Pediatr Urol, 2007, 3(5): 387-390. doi: 10.1016/j.jpurol.2007.01.194
[18] Shimizu S, Saito M, Kinoshita Y, et al. Ischemic preconditioning and post-conditioning to decrease testicular torsion-detorsion injury[J]. J Urol, 2009, 182(4): 1637-1643. doi: 10.1016/j.juro.2009.06.010
[19] Tian XM, Tan XH, Shi QL, et al. Risk Factors for Testicular Atrophy in Children With Testicular Torsion Following Emergent Orchiopexy[J]. Front Pediatr, 2020, 8: 584796. doi: 10.3389/fped.2020.584796
[20] Zvizdic Z, Aganovic A, Milisic E, et al. Duration of symptoms is the only predictor of testicular salvage following testicular torsion in children: A case-control study[J]. Am J Emerg Med, 2021, 41: 197-200. doi: 10.1016/j.ajem.2020.11.023
[21] 郭祥, 李爽, 陈海涛, 等. 儿童睾丸不全扭转的临床特点[J]. 中华男科学杂志, 2019, 25(11): 1005-1010. https://www.cnki.com.cn/Article/CJFDTOTAL-NKXB201911012.htm
[22] Lian BS, Ong CC, Chiang LW, et al. Factors Predicting Testicular Atrophy after Testicular Salvage following Torsion[J]. Eur J Pediatr Surg, 2016, 26(1): 17-21.
[23] Grimsby GM, Schlomer BJ, Menon VS, et al. Prospective Evaluation of Predictors of Testis Atrophy After Surgery for Testis Torsion in Children[J]. Urology, 2018, 116: 150-155.
-

| 引用本文: | 许鹏, 周云, 贾蓉, 等. 儿童睾丸扭转复位术后睾丸萎缩的危险因素分析[J]. 临床泌尿外科杂志, 2024, 39(3): 222-226. doi: 10.13201/j.issn.1001-1420.2024.03.009 |
| Citation: | XU Peng, ZHOU Yun, JIA Rong, et al. Risk factors analysis of testicular atrophy after torsion reduction in children[J]. J Clin Urol, 2024, 39(3): 222-226. doi: 10.13201/j.issn.1001-1420.2024.03.009 |
- Figure 1.
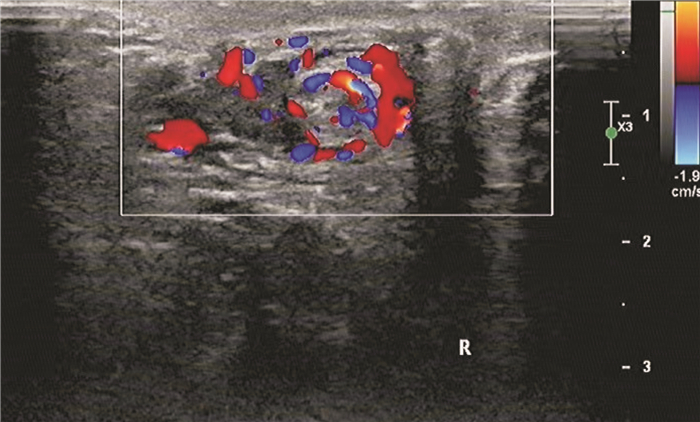
- Figure 2.
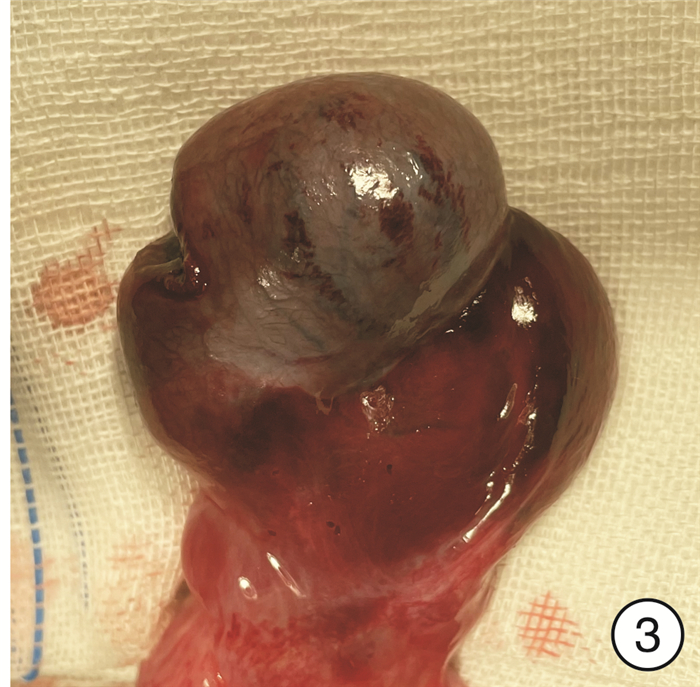
- Figure 3.
- Figure 4.



 下载:
下载: