Predictors and oncological benefits of pentafecta achievements in patients treated with laparoscopic radical cystectomy for bladder cancer
-
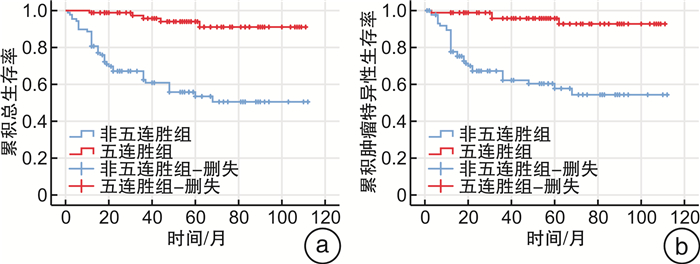
摘要: 目的 探讨中国膀胱癌(bladder cancer,BCa)患者行腹腔镜根治性膀胱切除术(laparoscopic radical cystectomy,LRC)达到五连胜对判断远期预后的价值,分析达到五连胜的预测因素。方法 对2015年5月—2022年4月在首都医科大学附属北京友谊医院、附属北京世纪坛医院及北京朝阳医院接受LRC的174例BCa患者进行回顾性分析。采用Zapał a等提出的五连胜标准:①切缘阴性;②清扫≥10个淋巴结;③术后90 d内不存在高级别(Clavien-Dindo Ⅲ~Ⅴ级)并发症;④术后1年内肿瘤无复发;⑤术后1年内无尿流改道相关并发症。同时满足以上5项标准视为实现“五连胜”,否则纳入非五连胜组。为均衡混杂因素,2组患者进行倾向性评分匹配(propensity score matching,PSM),按1∶1匹配,比较2组患者一般资料。PSM后,采用Kaplan-Meier法绘制生存曲线;采用Cox回归分析达成五连胜与患者术后总生存期(overall survival,OS)和肿瘤特异性生存期(cancer-specific survival,CSS)的关系;采用logistic回归分析五连胜达成的预测因素。结果 纳入的174例患者中,86例(49.4%)患者实现五连胜。其中,切缘阴性、清扫≥10个淋巴结、术后90 d内不存在高级别(Clavien-Dindo Ⅲ~Ⅴ级)并发症、术后1年内肿瘤无复发、术后1年内无尿流改道相关并发症的达成率分别为94.8%、75.3%、90.8%、83.3%、86.2%。在中位48个月的随访中,分别有42例患者死亡和40例患者出现肿瘤复发或转移。PSM前五连胜组与非五连胜组患者的年龄、性别、体重指数(BMI)、吸烟史、加速康复外科(enhanced recovery after surgery,ERAS)临床管理策略的应用情况、尿流改道类型(回肠通道术/回肠新膀胱术)、手术时间、术中出血量均差异无统计学意义;五连胜组患者术后病理T分期(P < 0.001)、淋巴结阳性率(P < 0.001)低于非五连胜组。PSM后,2组患者一般资料比较差异无统计学意义(P>0.05)。Kaplan-Meier生存曲线显示五连胜组患者的OS(P < 0.001)和CSS(P < 0.001)均显著高于非五连胜组。多因素Cox回归模型显示,达到五连胜是影响BCa患者LRC术后OS(HR=0.224,95%CI:0.073~0.682,P=0.008)和CSS(HR=0.133,95%CI:0.035~0.499,P=0.003)的独立危险因素。多因素logistic回归分析中,pT≥T3(OR=0.379,95%CI:0.184~0.780,P=0.008)、淋巴结阳性(OR=0.153,95%CI:0.049~0.479,P=0.001)均为影响五连胜达成的独立预测因素。结论 本组行LRC的中国患者实现五连胜比例与国际先进水平相似。实现五连胜显著改善BCa患者OS和CSS,其中T分期、淋巴结阳性是影响达到五连胜的独立预测因素。Abstract: Objective To investigate the value of achieving pentafecta outcome in laparoscopic radical cystectomy(LRC) for Chinese patients with bladder cancer(BCa) in predicting long-term prognosis and to analyze the predictive factors in achieving the pentafecta outcome.Methods A retrospective analysis was conducted on 174 BCa patients who underwent LRC from May 2015 to April 2022 at Beijing Friendship Hospital, Beijing Shijitan Hospital, and Beijing Chaoyang Hospital affiliated to Capital Medical University. The pentafecta criteria proposed by Zapał a were adopted, which were: ①negative surgical margins; ②dissection of ≥10 lymph nodes; ③no high-grade complications(Clavien-Dindo Ⅲ-Ⅴ) within 90 days after surgery; ④no tumor recurrence within 1 year after surgery; ⑤no urinary diversion-related complications within 1 year after surgery. Patients who met all five criteria were considered to have achieved "pentafecta", while those who did not were included in the non-pentafecta group. To balance confounding factors, propensity scores were used for the two patient groups, and 1∶1 matching was performed to compare the general data of the two groups. The Kaplan-Meier method was used to draw survival curves. Cox regression analysis was used to investigate the relationship between achieving pentafecta and the patients' overall survival(OS), cancer-specific survival(CSS) after surgery. Logistic regression analysis was performed to identify predictive factors in achieving the pentafecta outcome.Results Of the 174 patients included, 86(49.4%) achieved the pentafecta outcome. The achievement rates for negative surgical margin, dissection of ≥10 lymph nodes, no high-grade complications within 90 days postoperatively, no tumor recurrence within 1 year postoperatively, and no urinary diversion-related complications within 1 year postoperatively were 94.8%, 75.3%, 90.8%, 83.3%, and 86.2%, respectively. During a median follow-up period of 48 months, 42 patients died, and 40 patients experienced tumor recurrence or metastasis. There were no significant differences between the two groups in terms of age, gender, BMI, smoking history, ERAS, type of urinary diversion, operative time, intraoperative blood loss, or intraoperative blood loss. The T stage(P < 0.001), and positive lymph node rate(P < 0.001) were lower in the pentafecta group compared to the non-pentafecta group. The Kaplan-Meier survival curves revealed that the OS(P < 0.001) and CSS(P < 0.001) were significantly higher in the pentafecta group compared to the non-pentafecta group. Multivariate Cox regression analysis showed that achieving the pentafecta outcome was an independent predictor of OS(HR=0.224, 95%CI: 0.073-0.682, P=0.008) and CSS(HR=0.133, 95%CI: 0.035-0.499, P=0.003) after LRC for BCa patients. In multivariate logistic regression analysis, pT≥T3(OR=0.379, 95%CI: 0.184-0.780, P=0.008), positive lymph nodes(OR=0.153, 95%CI: 0.049-0.479, P=0.001) were identified as independent predictors of achieving the pentafecta outcome.Conclusion The proportion of Chinese patients achieving the pentafecta outcome in LRC is similar to the international advanced level. Achieving the pentafecta outcome significantly improves OS and CSS, and T stage and positive lymph nodes are independent predictors of achieving the pentafecta outcome.
-
Key words:
- bladder cancer /
- radical cystectomy /
- laparoscope /
- pentafecta /
- oncological outcome
-

-
表 1 倾向性匹配前患者基线资料
例(%),X±S 基线资料 整体队列 PSM队列 总数
(174例)非五连胜组
(88例)五连胜组
(86例)P值 总数
(110例)非五连胜组
(55例)五连胜组
(55例)P值 年龄/岁 62.8±9.3 63.9±8.8 61.6±9.7 0.498 62.3±9.5 63.4±9.0 61.2±10.0 0.233 男性 145(83.3) 76(86.4) 69(80.2) 0.437 96(87.3) 51(92.7) 45(81.8) 0.086 BMI/(kg/m2) 24.9±3.7 24.4±3.5 25.8±3.9 0.113 24.8±3.6 24.4±3.4 25.2±3.7 0.197 ASA≥3 19(10.9) 15(17.0) 4(4.7) 0.296 15(13.6) 8(14.5) 7(12.7) 0.781 aCCI 3.7±2.2 4.0±2.1 3.0±2.1 0.057 3.2±1.9 3.5±2.0 3.0±1.8 0.225 吸烟史 78(44.8) 48(54.5) 30(34.9) 0.238 46(41.8) 23(41.8) 23(41.8) 1.000 ERAS 62(35.6) 29(32.9) 33(38.3) 0.456 33(30.0) 21(38.2) 22(40.0) 0.845 尿流改道类型 0.331 0.057 回肠通道术 120(69.0) 67(76.1) 53(61.6) 70(63.6) 40(72.7) 30(54.5) 原位回肠新膀胱术 54(31.0) 21(23.9) 33(38.4) 40(36.4) 15(27.3) 25(45.5) 手术时间/h 390.5±126.4 390.5±121.7 390.4±139.9 0.900 424.0±141.8 426.5±128.7 621.6±153.9 0.856 术中出血量/mL 232.9±177.9 227.5±143.9 246.0±244.1 0.293 292.7±226.3 320.9±242.9 264.5±206.7 0.193 T分期 < 0.001 1.000 Ta~T2 110(63.2) 42(47.7) 68(79.1) 74(67.3) 37(67.3) 37(67.3) T3~T4 64(36.8) 46(52.3) 18(20.9) 36(32.7) 18(32.7) 18(32.7) N分期 < 0.001 1.000 N0 141(81.0) 59(67.0) 82(95.3) 102(92.7) 51(92.7) 51(92.7) N1~3 33(19.0) 29(33.0) 4(4.7) 8(7.3) 4(7.3) 4(7.3) 切缘阳性 9(5.2) 9(10.2) 0(0) < 0.001 6(5.4) 6(10.9) 0(0) 0.012 表 2 OS影响因素分析
因素 单因素 多因素 HR 95%CI P值 HR 95%CI P值 年龄 0.932 0.864~1.006 0.071 0.965 0.909~1.024 0.240 性别(男) 0.864 0.290~2.570 0.972 BMI 0.910 0.777~1.064 0.237 吸烟史 0.864 0.124~3.382 0.806 ASA≥3 0.648 0.124~3.382 0.607 aCCI 1.196 0.900~1.590 0.217 肌酐 1.008 0.989~1.027 0.400 T分期(≥T3) 2.964 0.891~9.867 0.077 3.632 1.444~9.131 0.006 淋巴结阳性 5.163 1.064~25.049 0.042 3.133 0.984~9.977 0.053 ERAS 0.901 0.229~3.548 0.881 尿流改道类型(回肠通道术vs原位回肠新膀胱术) 0.283 0.077~1.035 0.056 0.345 0.102~1.172 0.088 达到五连胜 0.211 0.060~0.745 0.016 0.224 0.073~0.682 0.008 表 3 CSS影响因素分析
因素 单因素 多因素 HR 95%CI P值 HR 95%CI P值 年龄 0.889 0.806~0.980 0.018 0.935 0.877~0.998 0.043 性别(男) 0.976 0.248~2.646 0.727 BMI 0.898 0.740~1.090 0.278 吸烟史 0.248 0.055~1.115 0.069 0.439 0.154~1.248 0.122 ASA≥3 0.137 0.012~1.536 0.107 aCCI 1.256 0.911~1.733 0.164 肌酐 1.019 0.998~1.040 0.081 1.011 0.995~1.027 0.187 T分期(≥T3) 5.212 1.150~23.614 0.032 5.152 1.688~15.727 0.004 淋巴结阳性 7.124 0.948~53.553 0.056 4.023 1.022~15.833 0.046 ERAS 0.545 0.110~2.687 0.456 尿流改道类型(回肠通道术vs原位回肠新膀胱术) 0.067 0.011~0.391 0.003 0.105 0.021~0.526 0.006 达到五连胜 0.088 0.017~0.454 0.004 0.133 0.035~0.499 0.003 表 4 RC五连胜预测因素分析
因素 单因素 多因素 OR 95%CI P值 OR 95%CI P值 年龄 1.014 0.965~1.065 0.586 性别(男) 0.573 0.172~1.911 0.365 BMI 1.055 0.949~1.173 0.323 ASA≥3 0.909 0.290~2.848 0.870 吸烟史 0.938 0.435~2.024 0.871 肌酐 0.990 0.974~1.006 0.238 T分期(≥T3) 0.419 0.185~0.947 0.037 0.379 0.184~0.780 0.008 淋巴结阳性 0.152 0.045~0.511 0.002 0.153 0.049~0.479 0.001 ERAS 0.899 0.395~2.045 0.799 尿流改道类型(原位回肠新膀胱术vs回肠通道术) 1.782 0.744~4.269 0.195 手术时长 1.000 0.997~1.003 0.945 术中出血 0.999 0.997~1.001 0.289 术中输血 1.331 0.451~3.926 0.605 -
[1] Gill E, Sandhu G, Ward DG, et al. The sirenic links between diabetes, obesity, and bladder cancer[J]. Int J Mol Sci, 2021, 22(20): 11150. doi: 10.3390/ijms222011150
[2] Jubber I, Ong S, Bukavina L, et al. Epidemiology of bladder cancer in 2023: a systematic review of risk factors[J]. Eur Urol, 2023, 84(2): 176-190. doi: 10.1016/j.eururo.2023.03.029
[3] Witjes JA, Bruins HM, Cathomas R, et al. European association of urology guidelines on muscle-invasive and metastatic bladder cancer: summary of the 2020 guidelines[J]. Eur Urol, 2021, 79(1): 82-104. doi: 10.1016/j.eururo.2020.03.055
[4] Kowalewski KF, Wieland VLS, Kriegmair MC, et al. Robotic-assisted versus laparoscopic versus open radical Cystectomy-a systematic review and network Meta-analysis of randomized controlled trials[J]. Eur Urol Focus, 2023, 9(3): 480-490. doi: 10.1016/j.euf.2022.12.001
[5] Aminoltejari K, Hird AE, Klaassen Z, et al. Robotic versus open cystectomy for bladder cancer: synthesizing the data from current systematic reviews and meta-analyses[J]. Ann Surg Oncol, 2023, 30(5): 2976-2987. doi: 10.1245/s10434-022-12692-w
[6] Clement KD, Pearce E, Gabr AH, et al. Perioperative outcomes and safety of robotic vs open cystectomy: a systematic review and meta-analysis of 12, 640 cases[J]. World J Urol, 2021, 39(6): 1733-1746. doi: 10.1007/s00345-020-03385-8
[7] Xu C, Zou W, Wang YH, et al. Bladder-sparing treatment for muscle-invasive bladder carcinoma using immune checkpoint inhibitors[J]. Crit Rev Oncol Hematol, 2023, 191: 104137. doi: 10.1016/j.critrevonc.2023.104137
[8] Brunocilla E, Pernetti R, Schiavina R, et al. The number of nodes removed as well as the template of the dissection is independently correlated to cancer-specific survival after radical cystectomy for muscle-invasive bladder cancer[J]. Int Urol Nephrol, 2013, 45(3): 711-719. doi: 10.1007/s11255-013-0461-8
[9] Małkiewicz B, Gurwin A, Karwacki J, et al. Management of bladder cancer patients with clinical evidence of lymph node invasion(cN+)[J]. Cancers(Basel), 2022, 14(21): 5286.
[10] Aziz A, Gierth M, Rink M, et al. Optimizing outcome reporting after radical cystectomy for organ-confined urothelial carcinoma of the bladder using oncological trifecta and pentafecta[J]. World J Urol, 2015, 33(12): 1945-1950. doi: 10.1007/s00345-015-1572-x
[11] Cacciamani GE, Winter M, Medina LG, et al. Radical cystectomy pentafecta: a proposal for standardisation of outcomes reporting following robot-assisted radical cystectomy[J]. BJU Int, 2020, 125(1): 64-72. doi: 10.1111/bju.14861
[12] Zapała Ł,
[13] Piazza P, Bravi CA, Puliatti S, et al. Assessing pentafecta achievement after robot-assisted radical cystectomy and its association with surgical experience: Results from a high-volume institution[J]. Urol Oncol, 2022, 40(6): 272. e11-272. e20.
[14] Oh JJ, Lee S, Ku JH, et al. Oncological outcome according to attainment of pentafecta after robot-assisted radical cystectomy in patients with bladder cancer included in the multicentre KORARC database[J]. BJU Int, 2021, 127(2): 182-189. doi: 10.1111/bju.15178
[15] von Deimling M, Rink M, Klemm J, et al. Oncological validation and discriminative ability of pentafecta criteria after open radical cystectomy[J]. BJU Int, 2023, 131(1): 90-100. doi: 10.1111/bju.15890
[16] Li K, Yang X, Zhuang JT, et al. External validation of Pentafecta in patients undergoing laparoscopic radical cystectomy: results from a high-volume center[J]. BMC Urol, 2022, 22(1): 41. doi: 10.1186/s12894-022-00987-9
[17] Gschwend JE, Heck MM, Lehmann J, et al. Extended versus limited lymph node dissection in bladder cancer patients undergoing radical cystectomy: survival results from a prospective, randomized trial[J]. Eur Urol, 2019, 75(4): 604-611. doi: 10.1016/j.eururo.2018.09.047
[18] Froehner M, Novotny V, Heberling U, et al. Relationship of the number of removed lymph nodes to bladder cancer and competing mortality after radical cystectomy[J]. Eur Urol, 2014, 66(6): 987-990. doi: 10.1016/j.eururo.2014.07.046
[19] von Deimling M, Furrer M, Mertens LS, et al. Impact of the extent of lymph node dissection on survival outcomes in clinically lymph node-positive bladder cancer[J]. BJU Int, 2024, 133(3): 341-350. doi: 10.1111/bju.16210
[20] Ploussard G, Briganti A, de la Taille A, et al. Pelvic lymph node dissection during robot-assisted radical prostatectomy: efficacy, limitations, and complications-a systematic review of the literature[J]. Eur Urol, 2014, 65(1): 7-16. doi: 10.1016/j.eururo.2013.03.057
[21] Laymon M, Mosbah A, Hashem A, et al. Predictors and survival benefit of achieving pentafecta in a contemporary series of open radical cystectomy[J]. Minerva Urol Nephrol, 2022, 74(4): 428-436.
[22] Baron P, Khene Z, Lannes F, et al. Multicenter external validation of the radical cystectomy pentafecta in a European cohort of patients undergoing robot-assisted radical cystectomy with intracorporeal urinary diversion for bladder cancer[J]. World J Urol, 2021, 39(12): 4335-4344. doi: 10.1007/s00345-021-03753-y
-




 下载:
下载: