Effect of 7F triple-lumen transurethral catheter on uroflow during pressure-flow study
-
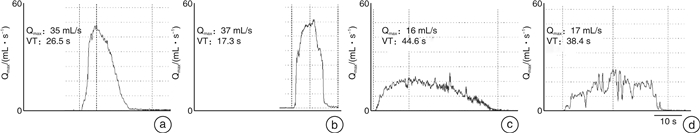
摘要: 目的 探讨尿道内置7F三腔测压管对压力-流率测定(pressure-flow study,PFS)时尿流率的影响。方法 回顾性分析2011年9月—2016年4月在华中科技大学同济医学院附属同济医院行尿动力学检查的患者资料,筛选出女性压力性尿失禁(stress urinary incontinence,SUI)、逼尿肌活动低下(detrusor underactivity,DU)、膀胱出口梗阻(bladder outlet obstruction,BOO)、逼尿肌过度活动(detrusor overactivity,DO)患者,共计875例。剔除置管前后尿流量相差超过20%的患者,最终406例患者被纳入研究。PFS采用7F三腔测压管,对比自由尿流率(free flow,FF)和PFS时的参数:最大尿流率(maximum flow rate,Qmax),尿流时间(flow time,FT),尿流量(voided volume,VV)以及尿流曲线形态变化。结果 各组的Qmax-PFS < Qmax-FF且FT-PFS>FT-FF。在女性患者中,SUI组的Qmax下降比例大于DU组。置管前后尿流曲线发生明显改变者在男性BOO组、DO组、DU组分别占35.0%、30.4%、14.7%;在女性DO组、SUI组、BOO组、DU组分别占52.9%、50.3%、41.5%、30.0%。结论 尿道内置7F三腔测压管会降低Qmax并延长尿流时间,测压管对尿流率的影响程度可能与性别和膀胱尿道的病理生理状态有关。Abstract: Objective To examine the effect of 7F triple-lumen transurethral catheter on uroflow during pressure-flow study (PFS).Methods We retrospectively analysed the data of patients received urodynamic study ranging from September 2011 to April 2016 in our center to collect both free flow (FF) and PFS parameters including maximum flow rate (Qmax), voided volume (VV) and flow time (FT) in patients with stress urinary incontinence (SUI), detrusor underactivity (DU), bladder outlet obstruction (BOO) and detrusor overactivity (DO). All patients underwent free uroflowmetry before PFS using 7F triple-lumen catheter. Of the 875 patients, 406 patients whose VV varying by less than 20% between the two tests were enrolled in our study. We compared their uroflow parameters and uroflow curve patterns between the two tests.Results Qmax-FF was significantly higher than Qmax-PFS and FT-PFS was significantly longer than FT-FF in all groups. ANOVA showed that the reduction rate of Qmaxwas significantly greater in group SUI than group DU of female patients. In group BOO, DO, DU of male patients, the uroflow patterns of PFS were getting worse than those of FF, accounted for 35.0%, 30.4%, 14.7% respectively. And in group DO, SUI, BOO, DU of female patients, it accounted for 52.9%, 50.3%, 41.5%, 30.0% respectively.Conclusion Using 7F triple-lumen urethral catheter significantly decreases Qmax and prolongs flow time. The influencing degree of catheterization on uroflow seems to be associated with gender and the physiopathologic status of the lower urinary tract.
-
Key words:
- urodynamics /
- free uroflow /
- pressure-flow study /
- urethral catheterization
-

-
表 1 患者的基本特征
组别 例数 年龄/岁 P值 SUI组 159 50.6±9.4 DU组 74 < 0.05 男 34 35.7±16.0 女 40 50.5±15.7 BOO组 122 < 0.05 男 40 60.0±10.9 女 82 44.5±12.3 DO组 51 > 0.05 男 17 43.2±18.1 女 34 49.7±17.3 表 2 男性患者FF与PFS参数的比较
X±S 组别 Qmax/(mL·s-1) P值 VV/mL P值 FT/s P值 Qmax下降率/% DU组(n=34) < 0.05 > 0.05 < 0.05 21.8±21.0 FF 10.8±4.4 317.6±111.0 55.0±18.4 PFS 8.5±4.0 320.4±108.4 80.6±30.0 BOO组(n=40) < 0.05 > 0.05 < 0.05 11.0±29.9 FF 8.0±3.8 265.5±100.5 68.3±29.4 PFS 6.8±3.7 263.2±97.7 93.2±29.0 DO组(n=17) < 0.05 > 0.05 < 0.05 20.0±15.2 FF 18.7±6.5 301.5±61.0 33.7±13.1 PFS 14.6±4.1 288.9±79.0 48.4±12.7 注:尿流量(voided volume,VV);尿流时间(flow time,FT)。 表 3 女性患者FF与PFS参数的比较
X±S 组别 Qmax/(mL·s-1) P值 VV/mL P值 FT/s P值 Qmax下降率/% SUI组(n=159) < 0.05 < 0.05 < 0.05 27.0±23.2 FF 29.7±12.1 398.3±133.7 27.5±10.9 PFS 20.8±8.8 409.2±126.7 60.8±34.2 DU组(n=40) < 0.05 > 0.05 < 0.05 11.4±30.4 FF 12.4±3.3 324.5±102.9 50.9±20.2 PFS 10.5±3.0 318.9±90.5 77.7±45.5 BOO组(n=82) < 0.05 < 0.05 < 0.05 20.0±31.6 FF 13.3±5.9 304.1±92.1 50.7±24.7 PFS 9.9±4.4 288.9±84.4 88.1±70.0 DO组(n=34) < 0.05 > 0.05 < 0.05 21.4±28.3 FF 25.5±12.3 276.4±83.5 26.5±16.7 PFS 18.9±10.0 278.3±86.0 53.3±37.3 表 4 各组PFS尿流曲线形态的异变率
例(%) 组别 PFS时的尿流曲线形态发生异变 P值 DO组 < 0.05 男 5(30.4) 女 18(52.9) BOO组 > 0.05 男 14(35.0) 女 34(41.5) DU组 > 0.05 男 5(14.7) 女 12(30.0) SUI组 80(50.3) -
[1] Drake MJ, Doumouchtsis SK, Hashim H, et al. Fundamentals of urodynamic practice, based on International Continence Society good urodynamic practices recommendations[J]. NeurourolUrodyn, 2018, 37(S6): S50-S60.
[2] Blaivas JG, Groutz A. Bladder outlet obstruction nomogram for women with lower urinary tract symptomatology[J]. NeurourolUrodyn, 2000, 19(5): 553-564.
[3] Cohn JA, Brown ET, Kaufman MR, et al. Underactive bladder in women: is there any evidence?[J]. CurrOpinUrol, 2016, 26(4): 309-314.
[4] Gammie A, Kaper M, Dorrepaal C, et al. Signs and Symptoms of Detrusor Underactivity: An Analysis of Clinical Presentation and Urodynamic Tests From a Large Group of Patients Undergoing Pressure Flow Studies[J]. EurUrol, 2016, 69(2): 361-369.
[5] Lose G, Thunedborg P, Jorgensen L, et al. A comparison of spontaneous and intubated urinary flow in female patients[J]. Neurourol Urodyn, 1986, 5: 1-4. doi: 10.1002/nau.1930050102
[6] Reynard JM, Lim C, Swami S, et al. The obstructive effect of a urethral catheter[J]. J Urol, 1996, 155(3): 901-903. doi: 10.1016/S0022-5347(01)66341-9
[7] 吴士良, 杨勇, 段继宏, 等. 膀胱测压检查尿流率与自由尿流率比值的临床意义[J]. 中华泌尿外科杂志, 2002, 23(8): 472-473. doi: 10.3760/j:issn:1000-6702.2002.08.008
[8] 殷凤朝, 李芳, 孙超, 等. 尿动力检测中尿道测压管对尿流率的影响[J]. 中国现代医学杂志, 2018, 28(2): 110-112. doi: 10.3969/j.issn.1005-8982.2018.02.024
[9] 马江伟, 高玉杰. 前列腺增生患者尿道内置F8测压管在压力-流率测定中对尿流率的影响[J]. 中国实用医药, 2019, 14(27): 36-37. https://www.cnki.com.cn/Article/CJFDTOTAL-ZSSA201927018.htm
[10] Zhu BS, Jiang HC, Li Y. Impact of urethral catheterization on uroflow during pressure-flow study[J]. J Int Med Res, 2016, 44(5): 1034-1039. doi: 10.1177/0300060516657700
[11] Groutz A, Blaivas JG, Sassone AM. Detrusor pressure uroflowmetry studies in women: effect of a 7Fr transurethral catheter[J]. J Urol, 2000, 164(1): 109-114. doi: 10.1016/S0022-5347(05)67460-5
[12] Koraitim M. Catheter as source of error in urodynamic study[J]. Urology, 1982, 20(2): 223-225. doi: 10.1016/0090-4295(82)90371-5
[13] Valentini FA, Robain G, Hennebelle DS, et al. Decreased maximum flow rate during intubated flow is not only due to urethral catheter in situ[J]. Int Urogynecol J, 2013, 24(3): 461-467. doi: 10.1007/s00192-012-1856-2
[14] Costantini E, Mearini L, Biscotto S, et al. Impact of different sized catheters on pressure-flow studies in women with lower urinary tract symptoms[J]. NeurourolUrodyn, 2005, 24(2): 106-110.
[15] Scaldazza CV, Morosetti C. Effect of different sized transurethral catheters on pressure-flow studies in women with lower urinary tract symptoms[J]. Urol Int, 2005, 75(1): 21-25. doi: 10.1159/000085922
[16] Duckett J, Cheema K, Patil A, et al. What is the relationship between free flow and pressure flow studies in women?[J]. Int Urogynecol J, 2013, 24(3): 447-452. doi: 10.1007/s00192-012-1883-z
[17] Harding C, Horsburgh B, DorkinTJ, et al. Quantifying the Effect of Urodynamic Catheters on Urine Flow Rate Measurement[J]. NeurourolUrodyn, 2012, 31(1): 139-142.
[18] Madsen FA, Rhodes PR, Bruskewitz RC. Reproducibility of pressure-flow variables in patients with symptomatic benign prostatic hyperplasia[J]. Urology, 1995, 46(6): 816-820. doi: 10.1016/S0090-4295(99)80350-1
[19] Walker RM, Di Pasquale B, Hubregtse M, et al. Pressure-flow studies in the diagnosis of bladder outlet obstruction: a study comparing suprapubic and transurethral techniques[J]. Br J Urol, 1997, 79(5): 693-697. doi: 10.1046/j.1464-410X.1997.00143.x
[20] Zhao SC, Zheng SB, Tan WL, et al. Pressure-flow studies in patients with benign prostatic hyperplasia: a study comparing suprapubic and transurethral methods[J]. Asian J Androl, 2006, 8(6): 731-735. doi: 10.1111/j.1745-7262.2006.00208.x
[21] 刘力搏, 许盛飞, 杜广辉. 压力-流率测定时尿道内置管对尿流率影响的研究现状[J]. 华中科技大学学报(医学版), 2018, 47(4): 502-507. doi: 10.3870/j.issn.1672-0741.2018.04.026
[22] Baseman AG, Baseman JG, Zimmern PE, et al. Effect of 6F urethral catheterization on urinary flow rates during repeated pressure-flow studies in healthy female volunteers[J]. Urology, 2002, 59(6): 843-846. doi: 10.1016/S0090-4295(02)01600-X
-




 下载:
下载:
