Construction and verification of nomogram prediction model for rhabdomyosarcoma of urogenital system
-
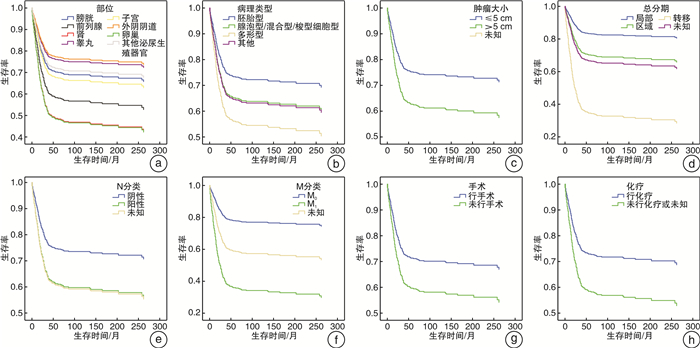
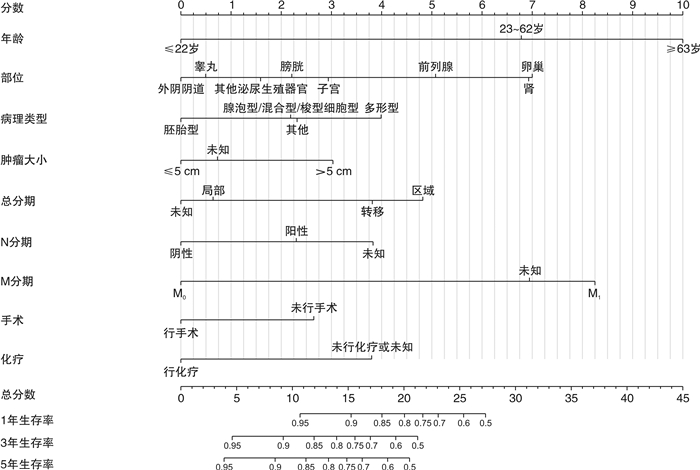
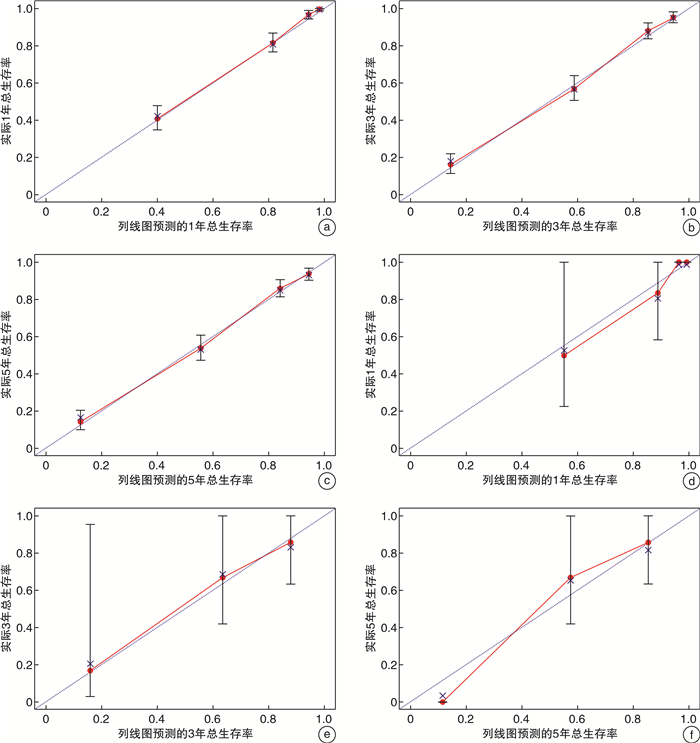
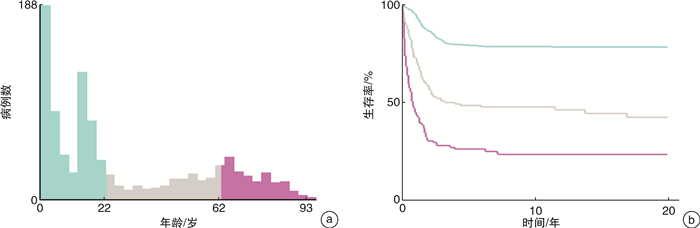
摘要: 目的 本研究目的是明确泌尿生殖系统横纹肌肉瘤(rhabdomyosarcoma,RMS)患者的临床病理特征,同时制作预测泌尿生殖系统RMS患者的1、3、5年生存率的列线图。方法 对1975—2016年SEER数据库确诊的泌尿及生殖系统RMS患者进行筛选,最终有990例患者纳入本研究。采用单因素及多因素Cox回归分析筛选泌尿及生殖系统RMS的独立危险因素,并以此来构建预测泌尿及生殖系统RMS生存率的列线图。选取2012—2018年郑州大学第一附属医院确诊的26例泌尿生殖系统RMS患者作为外部验证队列,然后采用C指数和校准曲线对模型进行内部及外部验证。结果 在泌尿及生殖系统RMS患者中,多因素Cox回归分析结果显示,患者的年龄、肿瘤部位、病理类型、肿瘤大小、总分期、N分类、M分类、手术、化疗均具有独立预测价值(P < 0.05)。根据上述变量构建预测模型,此列线图内部及外部验证的C指数分别为0.841、0.838,具有良好的区分度,同时内部及外部数据的校准曲线均显示出此预测模型具有较好的一致性。结论 本研究所构建的列线图可为泌尿及生殖系统RMS患者提供更为简洁的预后评估,为临床的个体化诊疗提供参考。Abstract: Objective The purpose of this study was to define the Clinical and pathological features of patients with rhabdomyosarcoma(RMS) of the urinary and genital system and to produce nomogram predicting 1-, 3-, and 5-year survival in patients with RMS of the urinary and genital system.Methods Patients with urological and genital rhabdomyosarcoma diagnosed in the SEER database from 1975-2016 were screened, and 990 patients were finally included in this study. Independent risk factors for urological and genital RMS were screened using univariate and multifactorial Cox regression analysis, and this was used to construct nomogram predicting survival in urological and genital RMS. The 26 patients with urogenital rhabdomyosarcoma diagnosed in the First Affiliated Hospital of Zhengzhou University from 2012 to 2018 were selected as the external verification cohort, and then the C-index and calibration curve were used to verify the model internally and externally.Results In patients with urinary and reproductive system RMS, the results of multivariate Cox regression analysis showed that the patient's age, tumor location, pathological type, tumor size, total stage, N classification, M classification, surgery, and chemotherapy all have independent predictive value(P < 0.05). The prediction model is constructed based on the above variables. The internal and externally verified C indexes of this nomogram are 0.841 and 0.838 respectively, which have good discrimination. At the same time, the calibration curves of internal and external data show that the prediction model has good consistency.Conclusion The nomogram constructed in this study can provide a more concise prognostic assessment for patients with urological and genital RMS and provide a reference for individualized clinical treatment
-
Key words:
- rhabdomyosarcoma /
- nomogram /
- prognostic model /
- urogenital system
-

-
表 1 建模队列和外部验证队列一般资料
例(%) 项目 建模队列
(n=990)外部验证队列
(n=26)项目 建模队列
(n=990)外部验证队列
(n=26)年龄 肿瘤大小 0~22岁 579(58.5) 19(73.1) ≤5 cm 245(24.7) 13(50.0) 23~62岁 209(21.1) 6(23.1) > 5 cm 408(41.2) 13(50.0) ≥63岁 202(20.4) 1(3.8) 未知 337(34.0) 0 性别 病理分级 男 536(54.1) 9(34.6) Ⅲ 135(13.6) - 女 454(45.9) 17(65.4) Ⅳ 162(16.4) - 种族 未知 693(70.0) - 白种人 724(73.1) 0 N分类 黑种人 202(20.4) 0 阴性 567(57.3) 25(96.2) 其他 56(5.7) 26(100.0) 阳性 232(23.4) 1(3.8) 未知 8(0.8) 0 未知 191(19.3) 0 部位 M分类 膀胱 123(12.4) 8(30.8) M0 692(69.9) 21(80.8) 前列腺 96(9.7) 1(3.8) M1 238(24.0) 5(19.2) 肾 18(1.8) 7(26.9) 未知 60(6.1) 0 睾丸 244(24.6) 7(26.9) 手术 子宫 288(29.1) 0 行手术 804(81.2) 21(80.8) 外阴阴道 74(7.5) 1(3.8) 未手术 186(18.8) 5(19.2) 卵巢 30(3.0) 0 放射治疗 其他泌尿生殖器官 117(11.8) 2(7.7) 行放射治疗 336(33.9) 4(15.4) 病理类型 未行放疗或未知 654(66.1) 22(84.6) 胚胎型 551(55.7) 18(69.2) 化疗 腺泡型/混合型/梭型细胞型 114(11.5) 6(23.1) 行化疗 717(72.4) 13(50.0) 多形型 57(5.8) 2(7.7) 未行化疗或未知 273(27.6) 13(50.0) 其他 268(27.1) 0 IRSG分级系统 总分期 1级 552(55.8) 9(34.6) 局部 402(40.6) 19(73.1) 2级 35(3.5) 7(26.9) 区域 273(27.6) 2(7.7) 3级 56(5.7) 5(19.2) 转移 240(24.2) 5(19.2) 4级 238(24.0) 5(19.2) 未知 75(7.6) 0 未知 109(11.0) 0 表 2 990例泌尿及生殖系统RMS预后的单因素和多因素分析结果
项目 单因素分析 多因素分析 HR(95%CI) P值 HR(95%CI) P值 年龄 < 0.001 < 0.001 23~62岁vs.0~22岁 3.365(2.568~4.410) < 0.001 2.864(2.061~3.979) < 0.001 ≥63岁vs.0~22岁 7.368(5.696~9.532) < 0.001 4.679(3.169~6.911) < 0.001 性别 男vs.女 2.107(1.699~2.612) < 0.001 种族 0.725 黑种人vs.白种人 1.152(0.889~1.494) 0.285 其他vs.白种人 1.132(0.725~1.767) 0.587 未知vs.白种人 < 0.001 0.913 部位 < 0.001 < 0.001 前列腺vs.膀胱 1.505(0.898~2.522) 0.121 1.589(0.991~2.549) 0.055 肾vs.膀胱 2.817(1.736~4.571) < 0.001 2.041(1.064~3.915 0.032 睾丸vs.膀胱 6.355(3.297~12.249) < 0.001 0.763(0.483~1.208) 0.249 子宫vs.膀胱 0.925(0.569~1.502) 0.751 1.121(0.740~1.698) 0.590 外阴阴道vs.膀胱 3.689(2.406~5.656) < 0.001 0.720(0.385~1.345) 0.303 卵巢vs.膀胱 1.009(0.532~1.914) 0.978 2.063(1.149~3.705) 0.015 其他泌尿生殖器官vs.膀胱 5.993(3.318~10.827) < 0.001 0.900(0.526~1.541) 0.702 病理类型 < 0.001 0.024 腺泡型/混合型/梭型细胞型vs.胚胎型 2.144(1.520~3.023) < 0.001 1.370(0.977~1.997) 0.067 多形型vs.胚胎型 5.419(3.708~7.919) < 0.001 1.851(1.193~2.873) 0.006 其他vs.胚胎型 3.878(3.035~4.955) < 0.001 1.429(1.061~1.924) 0.019 肿瘤大小 < 0.001 0.003 > 5 cm vs.≤5 cm 3.080(2.207~4.297) < 0.001 1.612(1.131~2.298) 0.008 未知vs.≤5 cm 2.578(1.818~3.655) < 0.001 1.130(0.775~1.647) 0.526 总分期 < 0.001 0.004 区域vs.局部 1.945(1.408~2.688) < 0.001 1.908(1.342~2.712) < 0.001 转移vs.局部 6.410(4.822~8.522) < 0.001 1.630(0.212~12.529) 0.639 未知vs.局部 3.122(2.041~4.776) < 0.001 0.905(0.276~2.967) 0.870 病理分级 < 0.001 Ⅳvs.Ⅲ 1.371(0.974~1.929) 0.071 未知vs.Ⅲ 0.618(0.459~0.830) 0.001 N分类 < 0.001 0.001 阳性vs.阴性 2.135(1.667~2.735) < 0.001 1.423(1.076~1.880) 0.013 未知vs.阴性 2.141(1.639~2.798) < 0.001 1.784(1.303~2.443) < 0.001 M分类 < 0.001 0.041 M1vs.M0 4.704(3.763~5.881) < 0.001 3.553(0.474~26.650) 0.217 未知vs.M0 2.741(1.832~4.103) < 0.001 2.943(0.881~9.833) 0.079 手术 行手术vs.未手术 2.057(1.621~2.611) < 0.001 1.450(1.084~1.939) 0.010 放射治疗 行放射治疗vs.未行放疗或未知 1.154(0.921~1.445) 0.213 化疗 行化疗vs.未行化疗或未知 2.703(2.177~3.356) < 0.001 1.763(1.326~2.344) < 0.001 IRSG分级系统 < 0.001 2级vs.1级 1.050(0.513~2.148) 0.894 3级vs.1级 1.266(0.740~2.166) 0.389 4级vs.1级 4.791(3.774~6.081) < 0.001 未知vs.1级 1.834(1.273~2.643) 0.001 -
[1] Lee RJ, Lee KK, Lin T, et al. Rhabdomyosarcoma of the head and neck: impact of demographic and clinicopathologic factors on survival[J]. Oral Surg Oral Med Oral Pathol Oral Radiol, 2017, 124(3): 271-279. doi: 10.1016/j.oooo.2017.05.507
[2] Ognjanovic S, Linabery AM, Charbonneau B, et al. Trends in childhood rhabdomyosarcoma incidence and survival in the United States, 1975-2005[J]. Cancer, 2009, 115(18): 4218-4226. doi: 10.1002/cncr.24465
[3] Jiang C, Zhao W, Qin M, et al. CD56-chimeric antigen receptor T-cell therapy for refractory/recurrent rhabdomyosarcoma: A 3.5-year follow-up case report[J]. Medicine(Baltimore), 2019, 98(43): e17572.
[4] Saltzman AF, Cost NG. Current Treatment of Pediatric Bladder and Prostate Rhabdomyosarcoma[J]. Curr Urol Rep, 2018, 19(1): 11. doi: 10.1007/s11934-018-0761-8
[5] Williams M, Catchpoole D. Sequestration of AS-DACA into acidic compartments of the membrane trafficking system as a mechanism of drug resistance in rhabdomyosarcoma[J]. Int J Mol Sci, 2013, 14(7): 13042-13062. doi: 10.3390/ijms140713042
[6] Zhen H, Liu Z, Guan H, et al. Second Malignant Neoplasms in Patients With Rhabdomyosarcoma[J]. Front Oncol, 2021, 11: 757095. doi: 10.3389/fonc.2021.757095
[7] Nguyen A, Fassas S, Freidberg N, et al. Recurrence and treatment of adult primary nonmetastatic bladder rhabdomyosarcoma: A systematic review[J]. Urol Oncol, 2021, 39(11): 774-780. doi: 10.1016/j.urolonc.2021.07.008
[8] 中华医学会小儿外科学分会泌尿学组. 膀胱/前列腺横纹肌肉瘤专家共识[J]. 临床小儿外科杂志, 2019, 18(11): 902-905, 921. doi: 10.3969/j.issn.1671-6353.2019.11.002
[9] Barnholtz-Sloan JS, Yu C, Sloan AE, et al. A nomogram for individualized estimation of survival among patients with brain metastasis[J]. Neuro Oncol, 2012, 14(7): 910-918. doi: 10.1093/neuonc/nos087
[10] 黄恒海, 林晓操, 黎德林, 等. 睾丸旁胚胎性横纹肌肉瘤1例[J]. 临床泌尿外科杂志, 2022, 37(1): 80-82. https://www.cnki.com.cn/Article/CJFDTOTAL-LCMW202201018.htm
[11] Bergamaschi L, Bertulli R, Casanova M, et al. Rhabdomyosarcoma in adults: analysis of treatment modalities in a prospective single-center series[J]. Med Oncol, 2019, 36(7): 59. doi: 10.1007/s12032-019-1282-0
[12] Hays DM, Shimada H, Raney RB Jr, et al. Sarcomas of the vagina and uterus: the Intergroup Rhabdomyosarcoma Study[J]. J Pediatr Surg, 1985, 20(6): 718-724. doi: 10.1016/S0022-3468(85)80032-4
[13] Raney RB Jr, Gehan EA, Hays DM, et al. Primary chemotherapy with or without radiation therapy and/or surgery for children with localized sarcoma of the bladder, prostate, vagina, uterus, and cervix. A comparison of the results in Intergroup Rhabdomyosarcoma Studies Ⅰ and Ⅱ[J]. Cancer, 1990, 66(10): 2072-2081. doi: 10.1002/1097-0142(19901115)66:10<2072::AID-CNCR2820661006>3.0.CO;2-9
[14] Martelli H, Oberlin O, Rey A, et al. Conservative treatment for girls with nonmetastatic rhabdomyosarcoma of the genital tract: A report from the Study Committee of the International Society of Pediatric Oncology[J]. J Clin Oncol, 1999, 17(7): 2117-2122. doi: 10.1200/JCO.1999.17.7.2117
[15] Skapek SX, Anderson J, Barr FG, et al. PAX-FOXO1 fusion status drives unfavorable outcome for children with rhabdomyosarcoma: a children's oncology group report[J]. Pediatr Blood Cancer, 2013, 60(9): 1411-1417. doi: 10.1002/pbc.24532
[16] Bortnick E, Stock J, Ferrer F. Genito-urinary rhabdomyosarcoma-challenges and controversies for the urologist[J]. Transl Androl Urol, 2020, 9(5): 2422-2429. doi: 10.21037/tau-20-511
[17] Ferrari A, Dileo P, Casanova M, et al. Rhabdomyosarcoma in adults. A retrospective analysis of 171 patients treated at a single institution[J]. Cancer, 2003, 98(3): 571-580. doi: 10.1002/cncr.11550
[18] Dumont SN, Araujo DM, Munsell MF, et al. Management and outcome of 239 adolescent and adult rhabdomyosarcoma patients[J]. Cancer Med, 2013, 2(4): 553-563. doi: 10.1002/cam4.92
[19] Kirsch CH, Goodman M, Esiashvili N. Outcome of female pediatric patients diagnosed with genital tract rhabdomyosarcoma based on analysis of cases registered in SEER database between 1973 and 2006[J]. Am J Clin Oncol, 2014, 37(1): 47-50. doi: 10.1097/COC.0b013e31826b98e4
[20] Nasioudis D, Alevizakos M, Chapman-Davis E, et al. Rhabdomyosarcoma of the lower female genital tract: an analysis of 144 cases[J]. Arch Gynecol Obstet, 2017, 296(2): 327-334. doi: 10.1007/s00404-017-4438-1
[21] 左昊, 陈罗军, 刘华丽, 等. 横纹肌肉瘤患者列线图预后模型的构建[J]. 中国肿瘤临床, 2019, 46(18): 934-939. doi: 10.3969/j.issn.1000-8179.2019.18.881
[22] Zhu L, Sun Y, Wang X, et al. Survival stratification in childhood rhabdomyosarcoma of the extremities: a derivation and validation study[J]. Sci Rep, 2020, 10(1): 5684. doi: 10.1038/s41598-020-62656-x
[23] Yang L, Takimoto T, Fujimoto J. Prognostic model for predicting overall survival in children and adolescents with rhabdomyosarcoma[J]. BMC Cancer, 2014, 14: 654. doi: 10.1186/1471-2407-14-654
[24] Zhang Y, He C, Lian Y, et al. Score for the Survival Probability of Patients With Orbital Rhabdomyosarcoma After Surgery: A Long-Term and Large Cohort Study[J]. Front Oncol, 2020, 10: 1590. doi: 10.3389/fonc.2020.01590
[25] Han D, Li C, Li X, et al. Prognostic Factors in Patients with Rhabdomyosarcoma Using Competing-Risks Analysis: A Study of Cases in the SEER Database[J]. J Oncol, 2020, 2020: 2635486.
[26] Chisholm JC, Marandet J, Rey A, et al. Prognostic factors after relapse in nonmetastatic rhabdomyosarcoma: a nomogram to better define patients who can be salvaged with further therapy[J]. J Clin Oncol, 2011, 29(10): 1319-1325. doi: 10.1200/JCO.2010.32.1984
-




 下载:
下载: