-
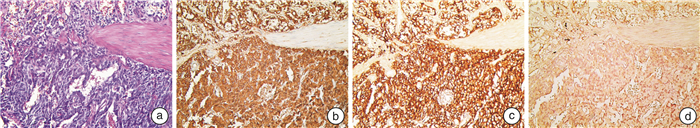
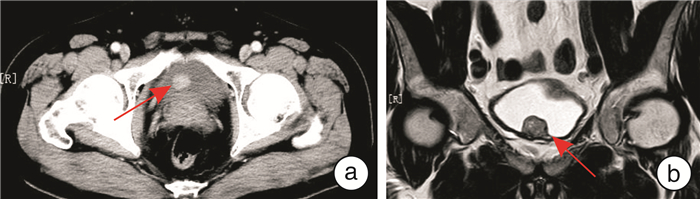
摘要: 目的 分析膀胱副神经节瘤的临床诊疗方法,以提高其诊疗技术水平。方法 回顾性分析2011年6月—2021年8月徐州市中心医院和蚌埠医学院第一附属医院收治的8例膀胱副神经节瘤患者的临床资料和随访结果。结果 所有患者术后病理结果均提示膀胱副神经节瘤,免疫组织化学染色标志物突触素(Syn)、瘤细胞嗜铬素A(CgA)均为阳性。术后随访3~126个月,平均59.3个月,8例患者均存活,术后无明显并发症,7例无复发,1例复发。结论 膀胱副神经节瘤临床易诊断,结合临床表现、影像学、膀胱镜可初步诊断,病理诊断可确诊。手术是治疗膀胱副神经节瘤的有效手段,术后并发症少,不易复发,能有效提高患者生活质量。Abstract: Objective To analyze the clinical diagnosis and treatment methods of paraganglioma of bladder, so as to improve the diagnosis and treatment.Methods The clinical data and follow-up results of 8 patients with paraganglioma of bladder admitted to Xuzhou Central Hospital and First Affiliated Hospital of Bengbu Medical College from June 2011 to August 2021 were retrospectively studied.Results Postoperative pathological results of all patients in this study indicated paraganglioma of bladder, and immunohistochemical staining marker synaptophysin (Syn) and chromogranin A (CgA) were positive. The patients were followed up for 3-126 months with an average of 59.3 months. All 8 patients survived without significant postoperative complications, and only 1 patient had recurrence.Conclusion Bladder paraganglioma is easy to be diagnosed clinically, and bladder paraganglioma can be preliminarily diagnosed through cystoscopy combined with clinical manifestations and imaging results. However, its final diagnosis relies on pathology. Surgery is an effective means to treat bladder paraganglioma for its less postoperative complications, low recurrence rate and satisfactory patients' quality of life.
-
Key words:
- paraganglioma /
- pheochromocytoma /
- bladder /
- diagnosis /
- treatment /
- prognosis
-

-
[1] Neumann HPH, Young WF Jr, Eng C. Pheochromocytoma and Paraganglioma[J]. N Engl J Med, 2019, 381(6): 552-565. doi: 10.1056/NEJMra1806651
[2] Lam AK. Update on Adrenal Tumours in 2017 World Health Organization(WHO)of Endocrine Tumours[J]. Endocr Pathol, 2017, 28(3): 213-227. doi: 10.1007/s12022-017-9484-5
[3] 兰卫华, 蓝保华, 刘秋礼, 等. 嗜铬细胞瘤和副神经节瘤遗传学和基因诊断的研究进展[J]. 临床泌尿外科杂志, 2019, 34(12): 1003-1008. https://www.cnki.com.cn/Article/CJFDTOTAL-LCMW201912020.htm
[4] Tanabe A, Naruse M. Recent advances in the management of pheochromocytoma and paraganglioma[J]. Hypertens Res, 2020, 43(11): 1141-1151. doi: 10.1038/s41440-020-0531-0
[5] Pastor-Guzmán JM, López-García S, Giménez-Bachs JM, et al. Paraganglioma of the bladder: controversy regarding treatment[J]. Urol Int, 2004, 73(3): 270-275. doi: 10.1159/000080841
[6] Buffet A, Burnichon N, Favier J, et al. An overview of 20 years of genetic studies in pheochromocytoma and paraganglioma[J]. Best Pract Res Clin Endocrinol Metab, 2020, 34(2): 101416. doi: 10.1016/j.beem.2020.101416
[7] Chow L, Chan M, Wong S. Functional Ulnar Nerve Paraganglioma: First Documented Occurrence in the Extremity With Hitherto Undescribed Associated Extensive Glomus Cell Hyperplasia and Tumorlet Formation[J]. Int J Surg Pathol, 2018, 26(1): 64-72. doi: 10.1177/1066896917720750
[8] Zimmerman IJ, Biron RE, Macmahon HE. Pheochromocytoma of the urinary bladder[J]. N Engl J Med, 1953, 249(1): 25-26. doi: 10.1056/NEJM195307022490106
[9] Malik AA, Afandi B, Jamil G, et al. Paraganglioma of urinary bladder[J]. BMJ Case Rep, 2013, 2013: bcr2013010063.
[10] Malhotra AK, Yan R, Tabeshi R, et al. Case-Bladder paraganglioma in a pediatric patient[J]. Can Urol Assoc J, 2018, 12(5): E260-E264. doi: 10.5489/cuaj.4937
[11] Zhai H, Ma X, Nie W, et al. Paraganglioma of the Urinary Bladder: A Series of 22 Cases in a Single Center[J]. Clin Genitourin Cancer, 2017, 15(5): e765-e771. doi: 10.1016/j.clgc.2017.03.010
[12] Chaaya G, Morales J, Castiglioni A, et al. Paraganglioma of the Urinary Bladder: A Rare Cause of Hypertension and Urinary Tract Infections[J]. Am J Med Sci, 2018, 355(2): 191-194. doi: 10.1016/j.amjms.2017.03.037
[13] Lenders JW, Sluiter HE, Thien T, et al. Treatment of a phaeochromocytoma of the urinary bladder with nifedipine[J]. Br Med J(Clin Res Ed), 1985, 290(6482): 1624-1625.
[14] 窦相权, 黄聪, 李强, 等. 膀胱异位嗜铬细胞瘤的MR分析及临床意义[J]. 现代医用影像学, 2019, 28(5): 972-974. https://www.cnki.com.cn/Article/CJFDTOTAL-XDYY201905005.htm
[15] Perry CG, Sawka AM, Singh R, et al. The diagnostic efficacy of urinary fractionated metanephrines measured by tandem mass spectrometry in detection of pheochromocytoma[J]. Clin Endocrinol(Oxf), 2007, 66(5): 703-708. doi: 10.1111/j.1365-2265.2007.02805.x
[16] Qin J, Zhou G, Chen X. Imaging manifestations of bladder paraganglioma[J]. Ann Palliat Med, 2020, 9(2): 346-351. doi: 10.21037/apm.2020.03.09
[17] Quist EE, Javadzadeh BM, Johannesen E, et al. Malignant paraganglioma of the bladder: a case report and review of the literature[J]. Pathol Res Pract, 2015, 211(2): 183-188. doi: 10.1016/j.prp.2014.10.009
[18] Frantellizzi V, Pontico M, Letizia C, et al. Bladder wall paraganglioma located using(123) I-mIBG SPECT and CT imaging[J]. Rev Esp Med Nucl Imagen Mol(Engl Ed), 2018, 37(4): 253-254.
[19] Zhang J, Bai X, Yuan J, et al. Bladder paraganglioma: CT and MR imaging characteristics in 16 patients[J]. Radiol Oncol, 2021, 56(1): 46-53. doi: 10.2478/raon-2021-0055
[20] Hou G, Jiang Y, Li F, et al. Site-based performance of 131I-MIBG imaging and 99mTc-HYNIC-TOC scintigraphy in the detection of nonmetastatic extra-adrenal paraganglioma[J]. Nucl Med Commun, 2022, 43(1): 32-41. doi: 10.1097/MNM.0000000000001490
[21] Cho DK, Kim JH, Chung N. Cardiovascular flashlight. Transient mid-ventricular ballooning cardiomyopathy associated with bladder pheochromocytoma[J]. Eur Heart J, 2009, 30(10): 1202. doi: 10.1093/eurheartj/ehp074
[22] Pahwa HS, Kumar A, Srivastava R, et al. Unsuspected pheochromocytoma of the urinary bladder: reminder of an important clinical lesson[J]. BMJ Case Rep, 2012, 2012: bcr2012006377.
[23] Katiyar R, Dwivedi S, Trivedi S, et al. Non-Functional Paraganglioma of the Urinary Bladder Treated by Transurethral Resection: Report of Two Cases[J]. J Clin Diagn Res, 2016, 10(2): XD01-XD03.
[24] Li W, Yang B, Che JP et al. Diagnosis and treatment of extra-adrenal pheochromocytoma of urinary bladder: case report and literature review[J]. Int J Clin Exp Med 2013, 6(9): 832-839.
[25] Thrasher JB, Rajan RR, Perez LM, et al. Pheochromocytoma of urinary bladder: contemporary methods of diagnosis and treatment options[J]. Urology, 1993, 41(5): 435-439. doi: 10.1016/0090-4295(93)90503-3
[26] Peczkowska M, Gessek J, Januszewicz A, et al. Pheochromocytoma of the urinary bladder coexisting with another extra-adrenal tumour-case report of a 19-year-old male patient[J]. Blood Press, 2002, 11(2): 101-105. doi: 10.1080/08037050211257
[27] Liang J, Li H, Gao L, et al. Bladder Paraganglioma: Clinicopathology and Magnetic Resonance Imaging Study of Five Patients[J]. Urol J, 2016, 13(2): 2605-2611.
[28] Mithqal A, Darvishi P, Rehm P. MIBG Localization of a Subclinical Paraganglioma of the Bladder[J]. Clin Nucl Med, 2017, 42(4): e196-e198. doi: 10.1097/RLU.0000000000001562
[29] Li M, Xu X, Bechmann N, et al. Correction to: Differences in clinical presentation and management between pre-and postsurgical diagnoses of urinary bladder paraganglioma: is there clinical relevance? A systematic review[J]. World J Urol, 2022, 40(2): 391. doi: 10.1007/s00345-021-03888-y
[30] Cheung V, Gill AJ, Chou A. Old, New, and Emerging Immunohistochemical Markers in Pheochromocytoma and Paraganglioma[J]. Endocr Pathol, 2018, 29(2): 169-175. doi: 10.1007/s12022-018-9534-7
[31] Fang F, Ding L, He Q, et al. Preoperative Management of Pheochromocytoma and Paraganglioma[J]. Front Endocrinol(Lausanne), 2020, 11: 586795. doi: 10.3389/fendo.2020.586795
[32] Tank AW, Lee Wong D. Peripheral and central effects of circulating catecholamines[J]. Compr Physiol, 2015, 5(1): 1-15.
[33] Pacak K. Preoperative management of the pheochromocytoma patient[J]. J Clin Endocrinol Metab, 2007, 92(11): 4069-4079. doi: 10.1210/jc.2007-1720
[34] Naranjo J, Dodd S, Martin YN. Perioperative Management of Pheochromocytoma[J]. J Cardiothorac Vasc Anesth, 2017, 31(4): 1427-1439. doi: 10.1053/j.jvca.2017.02.023
[35] 谢剑伟, 殷波. 原发性膀胱嗜铬细胞瘤一例并文献复习[J]. 现代肿瘤医学, 2019, 27(19): 3472-3474. doi: 10.3969/j.issn.1672-4992.2019.19.026
[36] Zhou M, Epstein JI, Young RH. Paraganglioma of the urinary bladder: a lesion that may be misdiagnosed as urothelial carcinoma in transurethral resection specimens[J]. Am J Surg Pathol, 2004, 28(1): 94-100. doi: 10.1097/00000478-200401000-00011
[37] Alkhatatbeh H, Alzaghari D, Alharahsheh S, et al. Urinary bladder pheochromocytoma managed with TURBT. Case report and review of literature[J]. Urol Case Rep, 2020, 33: 101291. doi: 10.1016/j.eucr.2020.101291
[38] Tu X, Zhang N, Zhuang X, et al. Incidental diagnosis of nonfunctional bladder paraganglioma: a case report and literature review[J]. BMC Urol, 2021, 21(1): 98. doi: 10.1186/s12894-021-00863-y
[39] Fishbein L, Bonner L, Torigian DA, et al. External beam radiation therapy(EBRT)for patients with malignant pheochromocytoma and non-head and-neck paraganglioma: combination with 131I-MIBG[J]. Horm Metab Res, 2012, 44(5): 405-410. doi: 10.1055/s-0032-1308992
[40] Gedik GK, Hoefnagel CA, Bais E, et al. 131I-MIBG therapy in metastatic phaeochromocytoma and paraganglioma[J]. Eur J Nucl Med Mol Imaging, 2008, 35(4): 725-733. doi: 10.1007/s00259-007-0652-6
[41] 李彬彬, 侯国良, 刘建华, 等. 膀胱副神经节瘤7例报告并文献复习[J]. 微创泌尿外科杂志, 2021, 10(2): 123-128. https://www.cnki.com.cn/Article/CJFDTOTAL-WCMN202102010.htm
[42] Granberg D, Juhlin CC, Falhammar H. Metastatic Pheochromocytomas and Abdominal Paragangliomas[J]. J Clin Endocrinol Metab, 2021, 106(5): e1937-e1952. doi: 10.1210/clinem/dgaa982
[43] 苏鹏, 刘志艳, Thomas J Giordano. 2017版WHO肾上腺肿瘤分类解读[J]. 中华病理学杂志, 2018, 47(10): 804-807. doi: 10.3760/cma.j.issn.0529-5807.2018.10.020
[44] Hamidi O, Young WF Jr, Iñiguez-Ariza NM, et al. Malignant Pheochromocytoma and Paraganglioma: 272 Patients Over 55 Years[J]. J Clin Endocrinol Metab, 2017, 102(9): 3296-3305. doi: 10.1210/jc.2017-00992
[45] Crona J, Taïeb D, Pacak K. New Perspectives on Pheochromocytoma and Paraganglioma: Toward a Molecular Classification[J]. Endocr Rev, 2017, 38(6): 489-515. doi: 10.1210/er.2017-00062
[46] Lenders JW, Duh QY, Eisenhofer G, et al. Pheochromocytoma and paraganglioma: an endocrine society clinical practice guideline[J]. J Clin Endocrinol Metab, 2014, 99(6): 1915-1942. doi: 10.1210/jc.2014-1498
[47] Hamidi O. Metastatic pheochromocytoma and paraganglioma: recent advances in prognosis and management[J]. Curr Opin Endocrinol Diabetes Obes, 2019, 26(3): 146-154. doi: 10.1097/MED.0000000000000476
[48] 罗瑶, 尚攀峰, 侯子珍, 等. 膀胱副神经节瘤: 单中心7例报告[J]. 现代泌尿外科杂志, 2022, 27(1): 50-53. https://www.cnki.com.cn/Article/CJFDTOTAL-MNWK202201010.htm
[49] Severi S, Bongiovanni A, Ferrara M, et al. Peptide receptor radionuclide therapy in patients with metastatic progressive pheochromocytoma and paraganglioma: long-term toxicity, efficacy and prognostic biomarker data of phase Ⅱ clinical trials[J]. ESMO Open, 2021, 6(4): 100171. doi: 10.1016/j.esmoop.2021.100171
-

| 引用本文: | 王光跃, 吕游, 刘形, 等. 膀胱原发性副神经节瘤8例诊治分析[J]. 临床泌尿外科杂志, 2022, 37(9): 702-707. doi: 10.13201/j.issn.1001-1420.2022.09.012 |
| Citation: | WANG Guangyue, LV You, LIU Xing, et al. Diagnosis and treatment of 8 cases of primary paraganglioma of bladder[J]. J Clin Urol, 2022, 37(9): 702-707. doi: 10.13201/j.issn.1001-1420.2022.09.012 |
- Figure 1.
- Figure 2.



 下载:
下载: