-
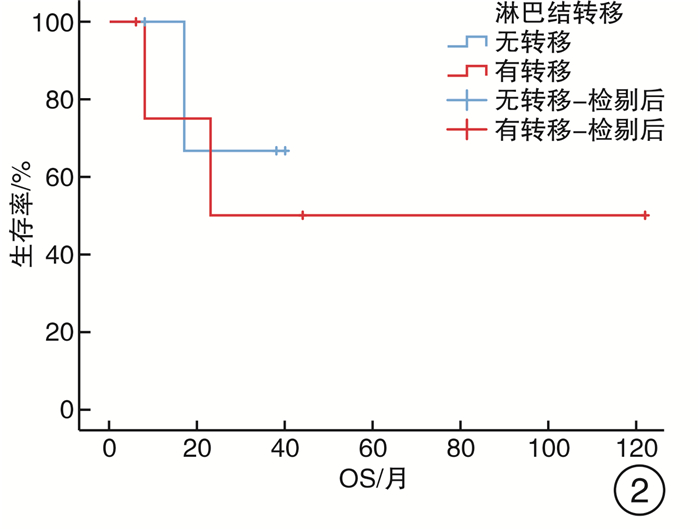
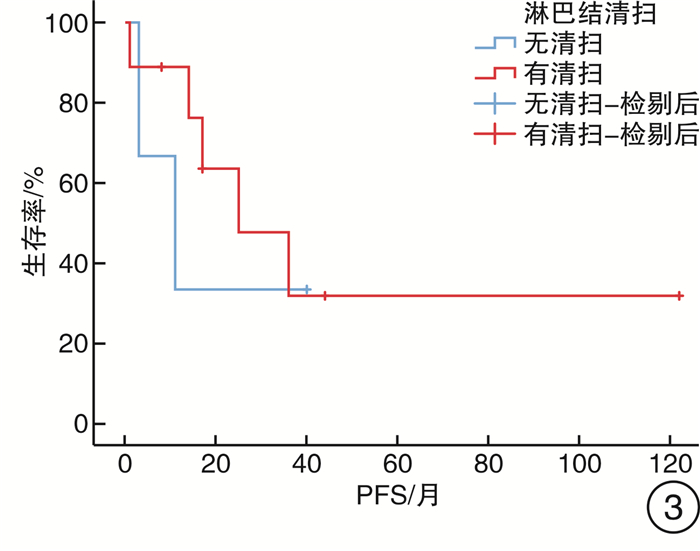
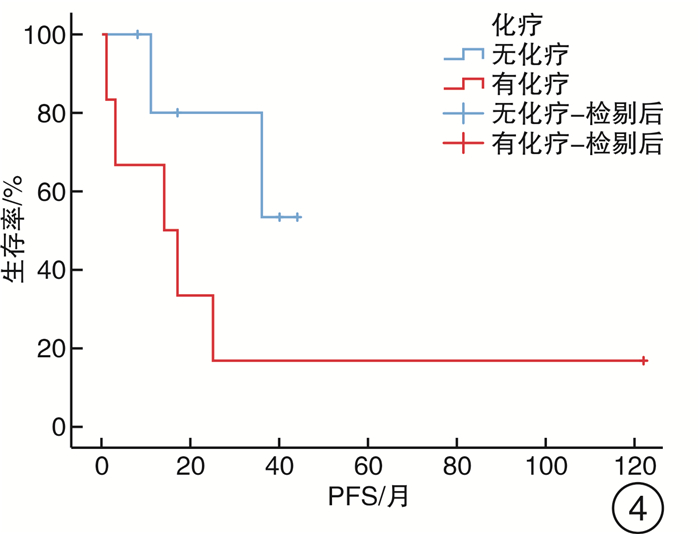
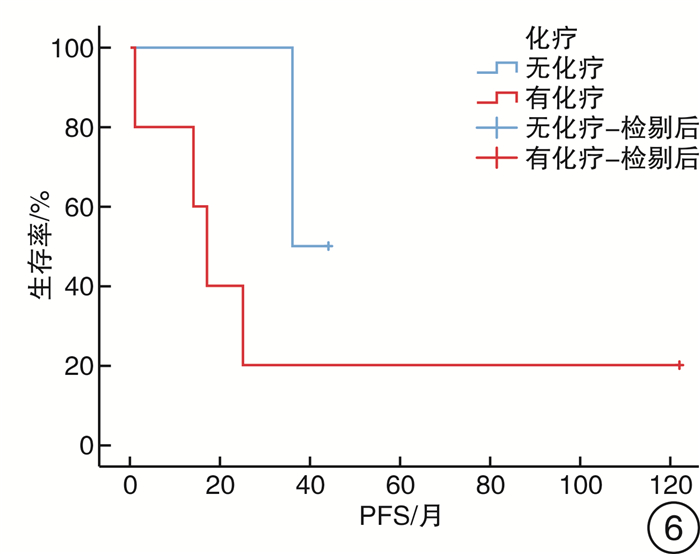
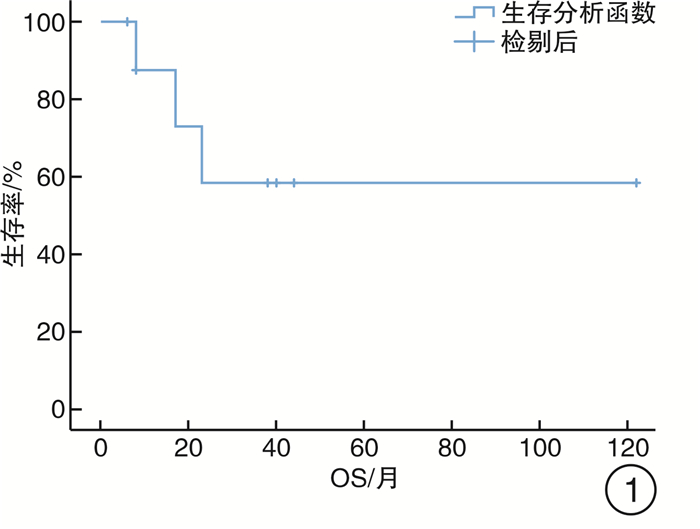
摘要: 本文回顾性分析云南省肿瘤医院2009—2020年诊治的17例尿道癌患者的临床资料,探讨女性原发性尿道癌的临床特点、诊疗及预后。17例女性原发性尿道癌患者平均年龄57岁;常见临床表现为尿道外口肿物、肉眼血尿、排尿困难;病理类型有腺癌、鳞癌、尿路上皮癌以及其他罕见病理组织类型;17例患者中有16例患者行手术,其中7例患者术后行辅助化疗,1例患者接受辅助放疗。随访时间6~122个月,其中3例患者死亡,6例患者目前仍存活,8例患者失访;经Kaplan-Meier生存分析显示,平均生存时间为78个月,由于随访人数较少,仅计算出23个月生存率为58.3%,中位无进展生存期(progression-free survival,PFS)为25个月。女性原发性尿道癌十分罕见,对于尿道远端局部肿瘤建议确保手术切缘阴性的情况下,行保留尿道的手术或行局部放射治疗替代尿道手术;对于局部晚期患者提倡多元模式治疗,以手术治疗为主选择性辅予放化疗治疗的综合治疗方案。Abstract: This paper retrospectively analyzed the clinical data of 17 female patients with urethral cancer treated in Yunnan Cancer Hospital from 2009 to 2020, and discussed the clinical characteristics, diagnosis, treatment and prognosis of female primary urethral cancer. These patients' average age was 57 years old. The common clinical manifestations were external orifice mass, gross hematuria and dysuria. The pathological types include adenocarcinoma, squamous cell carcinoma, urothelial carcinoma and other rare pathological tissue types. Of the 17 patients, 16 underwent surgery, of which 7 received adjuvant chemotherapy and 1 received adjuvant radiotherapy. The follow-up time ranged from 6 to 122 months, of which 3 patients died, 6 patients were still alive, and 8 patients were lost to follow-up. Kaplan-Meier survival analysis showed that the average survival time was 78 months. Due to the small number of follow-up, only the 23 month survival rate was calculated to be 58.3%, and the median progression free survival (PFS) was 25 months. Primary urethral cancer in women is very rare. It is recommended to perform urethra sparing surgery or local radiotherapy instead of urethra surgery if the surgical margin is negative. For locally advanced patients, we advocate a comprehensive treatment scheme of multi-mode treatment, surgery as the main treatment combined with selective adjuvant radiotherapy and chemotherapy.
-
Key words:
- female /
- primary urethral carcinoma /
- clinical characteristics /
- treatment /
- prognosis
-

-
表 1 17例女性原发性尿道癌的临床特点、治疗及预后
病例 年龄/岁 症状 肿瘤位置 病理类型 分期 手术方式 辅助治疗 随访结果 1 68 尿道外口肿物伴间断肉眼血尿 远端尿道 鳞癌+尿路上皮癌 T1N0M0 RU+UD+LD 无 术后8个月无瘤存活至今 2 65 尿道外口肿物、左侧腹股沟肿物 远端尿道 腺癌+鳞癌 TxN2M0 RU+UD+LD 化疗 术后6个月存活至今 3 53 右侧腹股沟肿物、会阴部出血 尿道全段 腺癌 T3N2M0 RU+UD+LD 化疗 术后23个月死亡 4 45 尿道外口肿物 远端尿道 黏液腺癌 T1N0M0 PU 无 术后40个月无瘤存活至今 5 54 外阴肿物、肉眼血尿 远端尿道 腺癌 T3N2M0 RU+UD+LD 无 术后44个月存活至今 6 75 外阴肿物、肉眼血尿、排尿困难 远端尿道 腺癌 T2N0M0 RU+UD 无 失访 7 58 尿道外口肿物 远端尿道 小细胞神经内分泌癌+腺癌 TxN2M1 PU 无 术后11个月复发 8 67 尿道外口肿物 远端尿道 腺癌 T2N0M0 RU+UD+LD 无 术后17个月死亡 9 70 肉眼血尿、排尿困难 远端尿道 尿路上皮癌 T2N2M0 RU+UD+LD 化疗 术后1年2个月复发 10 67 尿道外口肿物 远端尿道 尿路上皮癌 T1N0M0 PU 无 失访 11 73 肉眼血尿、排尿困难 近端尿道 腺癌 T3N0M0 UD 化疗 失访 12 14 尿道外口肿物 远端尿道 腺泡横纹肌肉瘤 TxN0M0 PU 化疗 术后38个月末次随访后失访 13 66 肉眼血尿 远端尿道 鳞癌 T3N2M0 RU+UD+LD 化疗 术后2年1个月复发,术后38个月存活至今 14 47 阴道流血 尿道中段 鳞癌 T3N1M0 RU+UD 放疗、化疗、右肾穿刺引流术 术后8个月死亡 15 49 尿道外口肿物 远端尿道 鳞癌 TxN1M0 RU+UD+LD 无 术后3年复发 16 50 尿道外口肿物 远端尿道 鳞癌 TxN2M0 无 化疗 失访 17 51 左腹股沟肿物 远端尿道 鳞癌 T2N2M0 PU+LD 化疗 术后122个月存活至今 注:RU:根治性尿道切除术;UD:尿流改道术;PU:尿道部分及肿瘤切除术;LD:淋巴结清扫术。 -
[1] Gatta G, van der Zwan JM, Casali PG, et al. Rare cancers are not so rare: the rare cancer burden in Europe[J]. Eur J Cancer, 2011, 47(17): 2493-2511. doi: 10.1016/j.ejca.2011.08.008
[2] Swartz MA, Porter MP, Lin DW, et al. Incidence of primary urethral carcinoma in the United States[J]. Urology, 2006, 68(6): 1164-1168. doi: 10.1016/j.urology.2006.08.1057
[3] Gakis G, Witjes JA, Compérat E, et al. EAU Guidelines on Primary Urethral Carcinoma[J]. Euro Urol, 2013, 64(5): 823-830. doi: 10.1016/j.eururo.2013.03.044
[4] Feldskou E, Thind P. Primary adenocarcinoma of the male urethra[J]. Ugeskr Laeger, 2012, 174(43): 2636-2637.
[5] Gakis G, Bruins HM, Cathomas R, et al. European Association of Urology Guidelines on Primary Urethral Carcinoma-2020 Update[J]. Eur Urol Oncol, 2020, 3(4): 424-432. doi: 10.1016/j.euo.2020.06.003
[6] Krukowski J, Czajkowski M, Kłącz J, et al. Primary urethral carcinoma-unexpected cause of urethral stricture. Case report and review of the literature[J]. Med Ultrason, 2019, 21(4): 494-496. doi: 10.11152/mu-2015
[7] Guo H, Peng X, Jin C, et al. Lichen Sclerosus Accompanied by Urethral Squamous Cell Carcinoma: A Retrospective Study From a Urethral Referral Center[J]. Am J Mens Health, 2018, 12(5): 1692-1699. doi: 10.1177/1557988318782095
[8] Colapinto V, Evans DH. Primary carcinoma of the male urethra developing after urethroplasty for stricture[J]. J Urol, 1977, 118(4): 581-584. doi: 10.1016/S0022-5347(17)58111-2
[9] Mohanty NK, Jolly BB, Saxena S, et al. Squamous cell carcinoma of perineal urethrostomy[J]. Urol Int, 1995, 55(2): 118-119. doi: 10.1159/000282765
[10] Sawczuk I, Acosta R, Grant D, et al. Post urethroplasty squamous cell carcinoma[J]. N Y State J Med, 1986, 86(5): 261-263.
[11] Mohan H, Bal A, Punia RP, et al. Squamous cell carcinoma of the prostate[J]. Int J Urol, 2003, 10(2): 114-116. doi: 10.1046/j.1442-2042.2003.00580.x
[12] Arva NC, Das K. Diagnostic dilemmas of squamous differentiation in prostate carcinoma case report and review of the literature[J]. Diagn Pathol, 2011, 6(1): 46. doi: 10.1186/1746-1596-6-46
[13] Cupp MR, Malek RS, Goellner JR, et al. Detection of human papillomavirus DNA in primary squamous cell carcinoma of the male urethra[J]. Urology, 1996, 48(4): 551-555. doi: 10.1016/S0090-4295(96)00246-4
[14] Thomas AA, Rackley RR, Lee U, et al. Urethral diverticula in 90 female patients: a study with emphasis on neoplastic alterations[J]. J Urol, 2008, 180(6): 2463-2467. doi: 10.1016/j.juro.2008.08.040
[15] Libby B, Chao D, Schneider BF. Non-surgical treatment of primary female urethral cancer[J]. Rare Tumors, 2010, 2(3): e55.
[16] Gheiler EL, Tefilli MV, Tiguert R, et al. Management of primary urethral cancer[J]. Urology, 1998, 52(3): 487-493. doi: 10.1016/S0090-4295(98)00199-X
[17] Touijer A K, Dalbagni G. Role of voided urine cytology in diagnosing primary urethral carcinoma[J]. Urology, 2004, 63(1): 33-35. doi: 10.1016/j.urology.2003.08.007
[18] Schubert T, Keegan KA, Kuczyk MA, et al. MP11-20 The predictive accuracy betweenclinical staging andpathological staging inpatients with primary urethral carcinoma[J]. J Urol, 2019, 201(Suppl 4): e135.
[19] Del Gaizo A, Silva AC, Lam-Himlin DM, et al. Magnetic resonance imaging of solid urethral and peri-urethral lesions[J]. Insights Imaging, 2013, 4(4): 461-469. doi: 10.1007/s13244-013-0259-3
[20] Itani M, Kielar A, Menias CO, et al. MRI of female urethra and periurethral pathologies[J]. Int Urogynecol J, 2016, 27(2): 195-204. doi: 10.1007/s00192-015-2790-x
[21] Stewart SB, Leder RA, Inman BA. Imaging tumors of the penis and urethra[J]. Urol Clin North Am, 2010, 37(3): 353-367. doi: 10.1016/j.ucl.2010.04.014
[22] Gakis G, Bruins HM, Cathomas R, et al. European Association of Urology Guidelines on Primary Urethral Carcinoma-2020 Update[J]. Eur Urol Oncol, 2020, 3(4): 424-432. doi: 10.1016/j.euo.2020.06.003
[23] Dimarco DS, Dimarco CS, Zincke H, et al. Surgical treatment for local control of female urethral carcinoma[J]. Urol Oncol, 2004, 22(5): 404-409. doi: 10.1016/S1078-1439(03)00174-1
[24] DiMarco DS, DiMarco CS, Zincke H, et al. Outcome of surgical treatment for primary malignant melanoma of the female urethra[J]. J Urol, 2004, 171(2 Pt 1): 765-767.
[25] Cahn DB, Handorf E, Ristau BT, et al. Contemporary practice patterns and survival outcomes for locally advanced urethral malignancies: A National Cancer Database Analysis[J]. Urol Oncol, 2017, 35(12): 670.e15-670.e21. doi: 10.1016/j.urolonc.2017.07.026
[26] Gakis G, Morgan TM, Daneshmand S, et al. Impact of perioperative chemotherapy on survival in patients with advanced primary urethral cancer: results of the international collaboration on primary urethral carcinoma[J]. Ann Oncol, 2015, 26(8): 1754-1759. doi: 10.1093/annonc/mdv230
[27] Sui W, RoyChoudhury A, Wenske S, et al. Outcomes and Prognostic Factors of Primary Urethral Cancer[J]. Urology, 2017, 100: 180-186. doi: 10.1016/j.urology.2016.09.042
[28] Abudurexiti M, Wang J, Shao N, et al. Prognosis of rare pathological primary urethral carcinoma[J]. Cancer Manag Res, 2018, 10: 6815-6822. http://www.dovepress.com/getfile.php?fileID=46806
-

| 引用本文: | 毕颖, 胡辰, 王启林. 女性原发性尿道癌17例报告[J]. 临床泌尿外科杂志, 2022, 37(10): 790-795. doi: 10.13201/j.issn.1001-1420.2022.10.014 |
| Citation: | BI Ying, HU Chen, WANG Qilin. Analysis and literature review of 17 cases of female primary urethral carcinoma[J]. J Clin Urol, 2022, 37(10): 790-795. doi: 10.13201/j.issn.1001-1420.2022.10.014 |
- Figure 1.
- Figure 2.
- Figure 3.
- Figure 4.
- Figure 5.
- Figure 6.



 下载:
下载: