Surgical effect and related prognostic factors in patients with renal cell carcinoma and venous tumor thrombus
-
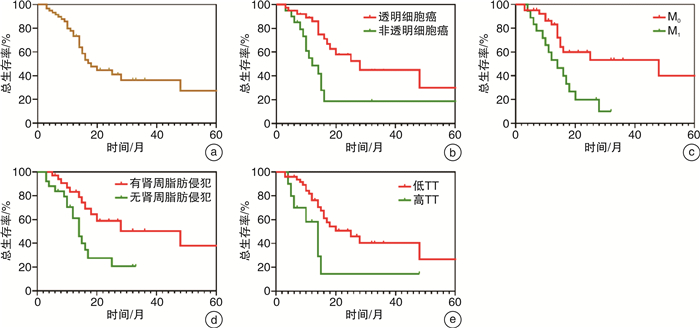
摘要: 目的 探讨伴有静脉癌栓肾癌患者行根治性肾切除联合静脉癌栓取出术的手术疗效及相关预后因素。方法 回顾性分析2013年5月—2022年2月于中国科学技术大学附属第一医院(安徽省立医院)行手术治疗的伴有静脉癌栓肾癌患者的临床资料。用Kaplan-Meier分析得到总生存曲线,用log-rank检验进行统计学比较;采用Cox回归模型进行多因素生存分析,寻找影响预后的独立危险因素。结果 共纳入59例患者,0~Ⅳ级癌栓分别有36例、4例、10例、5例、4例。围手术期无死亡事件发生。患者术后3年、5年总生存率分别为66.1%、50.1%。单因素Cox分析表明,病理类型(非透明细胞癌)(HR=2.613,95%CI:1.237~5.520,P<0.05)、癌栓分级(HR=2.339,95%CI:0.985~5.557,P<0.05)、M分期(HR=3.114,95%CI:1.474~6.578,P<0.05)、肾周脂肪侵犯(HR=2.986,95%CI:1.360~6.559,P<0.05)与患者预后相关;多因素Cox回归分析表明,病理类型(非透明细胞癌)(HR=3.326,95%CI:1.208~9.160,P<0.05)、M分期(HR=3.315,95%CI:1.284~8.558,P<0.05)以及肾周脂肪侵犯(HR=2.813,95%CI:1.133~6.988,P<0.05)是患者预后的独立危险因素。结论 对于伴有静脉癌栓肾癌患者,手术效果较好,可显著改善预后,非透明细胞癌、远处转移和肾周脂肪侵犯是影响其生存的独立危险因素。Abstract: Objective To investigate the curative effect and related prognostic factors of radical nephrectomy combined with removal of venous tumor thrombus in patients with renal cell carcinoma and venous tumor thrombus.Methods The clinical data of patients with renal cell carcinoma and venous tumor thrombus in First Affiliated Hospital of University of Science and Technology of China (Anhui Provincial Hospital) from May 2013 to February 2022 were analyzed retrospectively. An overall survival curve was obtained by Kaplan-Meier analysis, and statistical comparison was made by log-rank test. Cox regression model was used for multivariate survival analysis to find independent risk factors affecting prognosis.Results A total of 59 patients were included, including 36, 4, 10, 5 and 4 cases of 0-Ⅳ grade tumor thrombus, respectively. There was no death during the perioperative period, and the 3-and 5-year overall survival rates were 66.1% and 50.1%, respectively. Univariate Cox analysis revealed that the pathological type of non-clear cell carcinoma (HR=2.613, 95%CI: 1.237-5.520, P < 0.05), tumor thrombus Mayo grade (HR=2.339, 95%CI: 0.985-5.557, P < 0.05), M grade (HR=3.114, 95%CI: 1.474-6.578, P < 0.05), and perirenal fat invasion (HR=2.986, 95%CI: 1.360-6.559, P < 0.05) were related to postoperative overall survival. Multivariate Cox analysis showed that the pathological type of non-clear cell carcinoma (HR=3.326, 95%CI: 1.208-9.160, P < 0.05), M grade (HR=3.315, 95%CI: 1.284-8.558, P < 0.05) and perirenal fat invasion (HR=2.813, 95%CI: 1.133-6.988, P < 0.05) were independent risk factors affecting postoperative survival.Conclusion The surgical effect is good for patients with renal cell carcinoma and venous tumor thrombus, for it can significantly improve the prognosis of the patients. Non-clear cell carcinoma, distant metastasis and perirenal fat invasion are independent risk factors for survival.
-
Key words:
- renal cell carcinoma /
- tumor thrombus /
- prognosis
-

-
表 1 患者临床资料比较
例(%),X±S,M(P25,P75) 变量 总体(59例) Mayo 0~Ⅱ级癌栓组(49例) Mayo Ⅲ~Ⅳ级癌栓组(10例) P 性别 0.725 男 36(61) 29(59) 7(70) 女 23(39) 20(41) 3(30) 年龄/岁 62.24±11.64 63.47±10.82 56.20±14.14 0.259 BMI/(kg·m-2) 22.86±3.44 22.61±3.45 24.05±3.26 0.740 高血压 22(37) 18(37) 4(40) 1.000 糖尿病 7(12) 5(10) 2(20) 0.737 KPS 0.745 <80分 11(19) 10(20) 1(10) ≥80分 48(81) 39(80) 9(90) 血红蛋白/(g·L-1) 116.50±20.37 117.69±19.89 110.40±22.68 0.768 血清Ca2+/(mmol·L-1) 2.240(2.170,2.370) 2.240(2.185,2.360) 2.245(2.135,2.240) 0.895 副肿瘤综合征 10(17) 7(14) 3(30) 0.457 肿瘤侧别 0.953 左侧 30(51) 25(51) 5(50) 右侧 29(49) 24(49) 5(50) 血尿 26(44) 21(43) 5(50) 0.678 病理类型 0.074 透明细胞癌 39(66) 35(71) 4(40) 非透明细胞癌 20(34) 14(29) 6(60) Fuhrman分级 0.609 1+2 14(36) 12(34) 2(50) 3+4 25(64) 23(66) 2(50) 肿瘤直径/cm 8.82±3.12 8.60±3.12 9.90±3.08 0.913 T分期 0.130 T3 55(93) 47(96) 8(80) T4 4(7) 2(4) 2(20) N分期 1.000 N0(NX) 46(78) 38(78) 8(80) N1 13(22) 11(22) 2(20) M分期 0.475 M0 41(70) 35(71) 6(60) M1 18(30) 14(29) 4(40) 肾周脂肪侵犯 26(44) 21(43) 5(50) 0.678 肿瘤坏死 33(56) 27(55) 6(60) 1.000 术后靶向治疗 31(52.5) 25(51.0) 6(60.0) 0.734 开放手术 24(41) 17(35) 7(70) 0.039 微创(腹腔镜+机器人) 35(59) 32(65) 3(30) 住院天数/d 14.0(11.0,19.0) 13.0(11.0,18.0) 19.5(13.8,24.0) 0.039 术中输红细胞量/mL 200(0,800) 0(0,600) 1 300(750,3 250) <0.001 术中输血浆/mL 0(0,300.0) 0(0,0) 950.0(450.0,1 000.0) <0.001 术中出血量/mL 400(100,1 000) 300(50,600) 1 500(875,3 625) <0.001 手术时长/min 180.0(130.0,300.0) 170.0(130.0,260.0) 367.5(260.0,555.0) 0.002 术后转入ICU 14(24) 7(14) 7(70) 0.001 表 2 单因素及多因素Cox回归分析结果
因素 单因素分析 多因素分析 HR(95%CI) P HR(95%CI) P 病理类型 2.613(1.237~5.520) 0.012 3.326(1.208~9.160) 0.020 T分期 2.424(0.670~7.500) 0.190 2.087(0.457~9.529) 0.343 N分期 1.368(0.581~3.219) 0.473 0.570(0.193~1.690) 0.311 M分期 3.114(1.474~6.578) 0.003 3.315(1.284~8.558) 0.013 肾周脂肪侵犯 2.986(1.360~6.559) 0.006 2.813(1.133~6.988) 0.026 癌栓分级 2.339(0.985~5.557) 0.045 2.658(0.457~9.529) 0.063 -
[1] Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries[J]. CA Cancer J Clin, 2021, 71(3): 209-249. doi: 10.3322/caac.21660
[2] Abbasi A, Johnson TV, Ying K, et al. Duplicated vena cava with tumor thrombus from renal cancer: use of venogram for safer operative planning[J]. Urology, 2012, 79(4): e57-58. doi: 10.1016/j.urology.2011.06.044
[3] Reese AC, Whitson JM, Meng MV. Natural history of untreated renal cell carcinoma with venous tumor thrombus[J]. Urol Oncol, 2013, 31(7): 1305-1309. doi: 10.1016/j.urolonc.2011.12.006
[4] Martínez-Salamanca J I, Linares E, González J, et al. Lessons learned from the International Renal Cell Carcinoma-Venous Thrombus Consortium(IRCC-VTC)[J]. Curr Urol Rep, 2014, 15(5): 404. doi: 10.1007/s11934-014-0404-7
[5] Blute ML, Leibovich BC, Lohse CM, et al. The Mayo Clinic experience with surgical management, complications and outcome for patients with renal cell carcinoma and venous tumour thrombus[J]. BJU Int, 2004, 94(1): 33-41. doi: 10.1111/j.1464-410X.2004.04897.x
[6] Skinner DG, Pfister RF, Colvin R. Extension of renal cell carcinoma into the vena cava: the rationale for aggressive surgical management[J]. J Urol, 1972, 107(5): 711-716. doi: 10.1016/S0022-5347(17)61122-4
[7] McDougall E, Clayman RV, Elashry OM. Laparoscopic radical nephrectomy for renal tumor: the Washington University experience[J]. J Urol, 1996, 155(4): 1180-1185. doi: 10.1016/S0022-5347(01)66207-4
[8] Abaza R. Initial series of robotic radical nephrectomy with vena caval tumor thrombectomy[J]. Eur Urol, 2011, 59(4): 652-656. doi: 10.1016/j.eururo.2010.08.038
[9] Klatte T, Pantuck AJ, Riggs SB, et al. Prognostic factors for renal cell carcinoma with tumor thrombus extension[J]. J Urol, 2007, 178(4 Pt 1): 1189-1195.
[10] Haferkamp A, Bastian PJ, Jakobi H, et al. Renal cell carcinoma with tumor thrombus extension into the vena cava: prospective long-term followup[J]. J Urol, 2007, 177(5): 1703-1708. doi: 10.1016/j.juro.2007.01.039
[11] Whitson JM, Reese AC, Meng MV. Population based analysis of survival in patients with renal cell carcinoma and venous tumor thrombus[J]. Urol Oncol, 2013, 31(2): 259-263. doi: 10.1016/j.urolonc.2010.11.017
[12] ZapałaŁ, Sharma S, Kunc M, et al. Analysis of Clinicopathological Factors Influencing Survival in Patients with Renal Cell Carcinoma and Venous Tumor Thrombus[J]. J Clin Med, 2021, 10(17): 3852. doi: 10.3390/jcm10173852
[13] Chen Z, Yang F, Ge L, et al. Outcomes of renal cell carcinoma with associated venous tumor thrombus: experience from a large cohort and short time span in a single center[J]. BMC Cancer, 2021, 21(1): 766. doi: 10.1186/s12885-021-08508-x
[14] Master VA, Ethun CG, Kooby DA, et al. The value of a cross-discipline team-based approach for resection of renal cell carcinoma with IVC tumor thrombus: A report of a large, contemporary, single-institution experience[J]. J Surg Oncol, 2018, 118(8): 1219-1226. doi: 10.1002/jso.25271
[15] Shiff B, Breau RH, Mallick R, et al. Prognostic significance of extent of venous tumor thrombus in patients with non-metastatic renal cell carcinoma: Results from a Canadian multi-institutional collaborative[J]. Urol Oncol, 2021, 39(12): 836.e19-836.e27.
[16] Manso M, Pacheco-Figueiredo L, Santos-Silva A, et al. Renal Cell Carcinoma with Venous Thrombus: Should Surgery Be Offered When Metastasis Is Present at Diagnosis?[J]. Urol Int, 2018, 101(4): 387-390. doi: 10.1159/000493510
[17] Kirkali Z, Van Poppel H. A critical analysis of surgery for kidney cancer with vena cava invasion[J]. Eur Urol, 2007, 52(3): 658-662. doi: 10.1016/j.eururo.2007.05.009
[18] Xiao R, Xu C, Ge L, et al. Prognostic Value of Positive Lymph Nodes in Patients with Renal Cell Carcinoma and Tumor Thrombus Undergoing Nephrectomy and Thrombectomy[J]. Urol Int, 2021, 105(7-8): 657-665. doi: 10.1159/000514057
[19] Cao C, Bi X, Liang J, et al. Long-term survival and prognostic factors for locally advanced renal cell carcinoma with renal vein tumor thrombus[J]. BMC Cancer, 2019, 19(1): 144. doi: 10.1186/s12885-019-5359-0
[20] Shang B, Guo L, Shen R, et al. Prognostic Significance of NLR About NETosis and Lymphocytes Perturbations in Localized Renal Cell Carcinoma With Tumor Thrombus[J]. Front Oncol, 2021, 11: 771545. doi: 10.3389/fonc.2021.771545
[21] Gu L, Li H, Wang Z, et al. A systematic review and meta-analysis of clinicopathologic factors linked to oncologic outcomes for renal cell carcinoma with tumor thrombus treated by radical nephrectomy with thrombectomy[J]. Cancer Treat Rev, 2018, 69: 112-120. doi: 10.1016/j.ctrv.2018.06.014
[22] Tilki D, Nguyen HG, Dall'Era MA, et al. Impact of histologic subtype on cancer-specific survival in patients with renal cell carcinoma and tumor thrombus[J]. Eur Urol, 2014, 66(3): 577-583. doi: 10.1016/j.eururo.2013.06.048
[23] Capitanio U, Suardi N, Matloob R, et al. Extent of lymph node dissection at nephrectomy affects cancer-specific survival and metastatic progression in specific sub-categories of patients with renal cell carcinoma(RCC)[J]. BJU Int, 2014, 114(2): 210-215. doi: 10.1111/bju.12508
[24] Marchioni M, Bandini M, Pompe RS, et al. The impact of lymph node dissection and positive lymph nodes on cancer-specific mortality in contemporary pT(2-3) non-metastatic renal cell carcinoma treated with radical nephrectomy[J]. BJU Int, 2018, 121(3): 383-392. doi: 10.1111/bju.14024
[25] Bhindi B, Wallis CJD, Boorjian SA, et al. The role of lymph node dissection in the management of renal cell carcinoma: a systematic review and meta-analysis[J]. BJU Int, 2018, 121(5): 684-698. doi: 10.1111/bju.14127
[26] Karmali RJ, Suami H, Wood CG, et al. Lymphatic drainage in renal cell carcinoma: back to the basics[J]. BJU Int, 2014, 114(6): 806-817. doi: 10.1111/bju.12814
[27] Jürgens H, Ojamaa K, Pokker H, et al. Changes in therapy and survival of metastatic renal cell carcinoma in Estonia[J]. BMC Cancer, 2020, 20(1): 201. doi: 10.1186/s12885-020-6685-y
[28] 中国抗癌协会泌尿男生殖系肿瘤专业委员会肾癌学组. 高危非转移性肾癌术后辅助治疗中国专家共识(2020)[J]. 临床泌尿外科杂志, 2021, 36(4): 251-258. http://lcmw.cbpt.cnki.net/WKC/WebPublication/paperDigest.aspx?paperID=231cc528-3cef-47a8-aa56-12ce091b5b26
[29] Motzer RJ, Ravaud A, Patard JJ, et al. Adjuvant Sunitinib for High-risk Renal Cell Carcinoma After Nephrectomy: Subgroup Analyses and Updated Overall Survival Results[J]. Eur Urol, 2018, 73(1): 62-68. doi: 10.1016/j.eururo.2017.09.008
[30] Gul A, Rini BI. Adjuvant therapy in renal cell carcinoma[J]. Cancer, 2019, 125(17): 2935-2944. doi: 10.1002/cncr.32144
-




 下载:
下载: