Application experience of modified Politano-Leadbetter procedure under pneumatic bladder for the treatment of distal ureteral stenosis
-
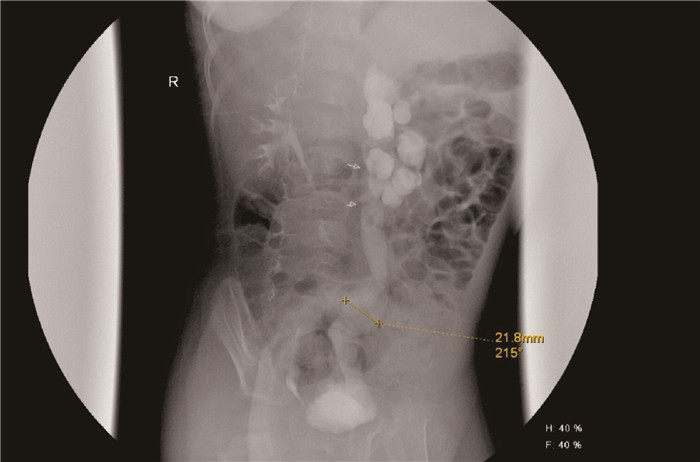
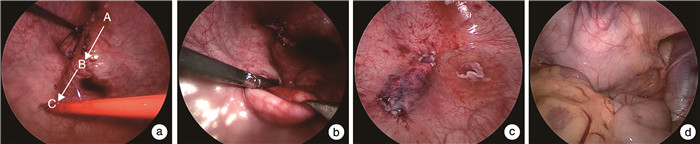
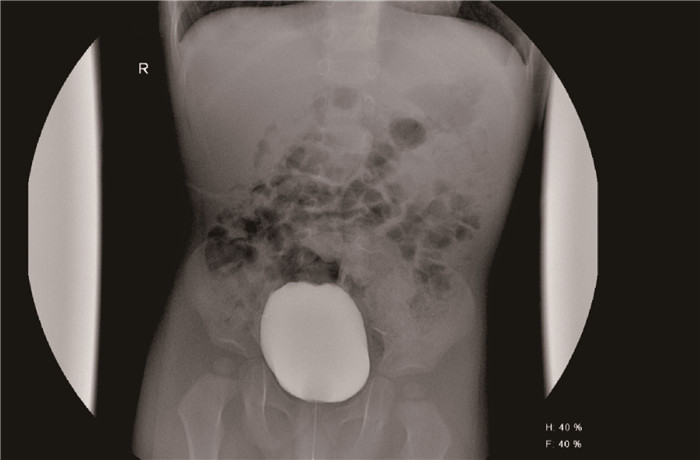
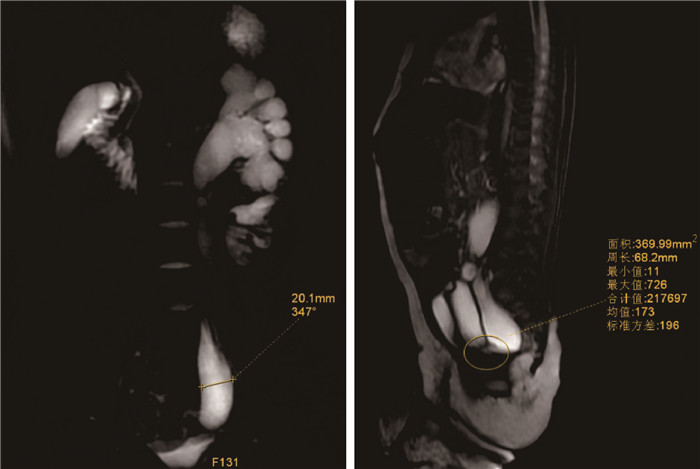
摘要: 目的 总结改良气膀胱下Politano-Leadbetter术治疗输尿管末端狭窄的经验,提高诊治水平。方法 回顾性分析厦门大学附属妇女儿童医院(厦门市妇幼保健院)小儿外科2020年1月—2022年1月收治的15例输尿管膀胱连接部狭窄患儿的临床资料,患儿均采用改良气膀胱下Politano-Leadbetter术治疗。其中男12例,女3例;年龄6个月~8岁,平均4.5岁;右侧5例,左侧9例,双侧1例。手术方法:建立气膀胱,膀胱内游离输尿管下段,末端输尿管口缝合牵引线,应用尿道口-输尿管开口-新输尿管裂孔三点一线原理,准确寻找膀胱外输尿管。将已游离的输尿管自新输尿管裂孔重新迁入膀胱内,建立黏膜下隧道,将输尿管远端包埋于黏膜下隧道内,缝合输尿管口,再置入双J管,完成Leadbetter输尿管再植手术。术后定期复查尿常规了解尿道感染情况,泌尿系彩超及排泄性膀胱尿道造影(voiding cystourethrography,VCUG)评估肾积水、输尿管扩张或狭窄、是否存在输尿管反流等指标。结果 15例患儿均经气膀胱下完成Politano-Leadbetter术,无一例中转开放手术。手术时间单侧81~103 min,平均(91.0±16.5) min;双侧136~165 min,平均(149.0±15.4) min。术中几乎无明显出血。留置尿管7~8 d,拔除尿管后所有患儿均未出现排尿困难、切口感染或裂开,住院时间8~15 d。术后随访12~24个月,近期无尿漏、切口感染、尿路感染,远期无膀胱输尿管反流、膀胱输尿管连接部梗阻等并发症。术后12个月复查彩超测得肾盂前后径为(0.95±0.35) cm,较术前的(2.68±0.75) cm明显减小;输尿管最大直径为(0.75±0.21) cm,也比术前的(2.85±0.65) cm明显减小,差异均有统计学意义(P < 0.01)。结论 改良气膀胱下Politano-Leadbetter术已是一种技术成熟且易于学习的手术方法,手术成功率高,术后恢复快,保留了原始输尿管的开口位置与解剖走向,是治疗小儿输尿管末端狭窄类疾病一种安全有效的手术方式。
-
关键词:
- Politano-Leadbetter术 /
- 腹腔镜 /
- 膀胱输尿管连接部狭窄 /
- 输尿管再植
Abstract: Objective To summarize the experience of the modified Politano-Leadbetter procedure under the pneumatic bladder for the treatment of distal ureteral stenosis, and improve the level of diagnosis and treatment.Methods A retrospective analysis was conducted on the clinical data of 15 children with ureterobladder junction stenosis admitted to the pediatric surgery department of Xiamen Maternal and Child Health Hospital from January 2020 to January 2022. All patients were treated with modified pneumatic bladder laparoscopic Politano-Leadbetter procedure including 12 boys and 3 girls; The average age was 4.5 years from 6 months to 8 years old. Among them, there were 5 cases on the right side, 9 cases on the left side, and 1 case on both sides. Operation method: establish the pneumatic bladder routinely, place laparoscope and operation instruments under cystoscope, free the ureter in the bladder, and apply the three-point one line principle of urethral orifice ureteral opening new ureteral hole to accurately find the ureter outside the bladder. Free the lower segment of the ureter, suture the traction line at the end of the ureter, relocate the already free ureter into the bladder from the new ureteral hiatus, establish a submucosal tunnel, embed the distal ureter into the submucosal tunnel, remove the narrow and partially dilated ureter, suture the urethral opening, and then insert a double J tube to complete the Leadbetter ureteral reimplantation surgery. Urine routine was regularly reviewed after the operation, and urinary color ultrasound and voiding cystourethrography (VCUG) were examined to evaluate indicators such as hydronephrosis, ureteral dilation or stenosis, presence of ureteral reflux, and renal function parameters.Results All 15 cases underwent Politano-Leadbetter surgery under the pneumatic bladder without conversion to open surgery. The unilateral surgery time was 81 to 103 minutes, with an average of (91.0±16.5) minutes. The bilateral surgery time ranged from 135 to 165 minutes, with an average of (149.0±15.4) minutes. There was almost no significant bleeding during the operation. After 8 days of surgery, the urinary catheter was removed, and all patients did not experience difficulty in urinating, incision infection, or incision dehiscence. The hospital stay was 8-15 days. All 15 cases were followed up for 12-24 months, and there were no complications such as urinary leakage, incision infection, urinary tract infection, bladder ureteral reflux, or obstruction of the ureter bladder junction. After 12 months of surgery, the value of the anterior and posterior diameter of the renal pelvis measured by color Doppler ultrasound was (0.95±0.35) cm compared to preoperative (2.68±0.75) cm, and the maximum diameter of the ureter was (0.75±0.21) cm compared to preoperative (2.85±0.65) cm. The difference was statistically significant (P < 0.01).Conclusion The modified Politano-Leadbetter procedure under the pneumatic bladder has become a mature surgical method for treating pediatric distal ureteral stenosis, and is easy to learn. It is safe and effective for its high success rate, fast postoperative recovery, and preservation of the original opening position and anatomical direction of the ureter. -

-
表 1 术前与术后12个月肾盂前后径、输尿管最大径的比较
cm,X±S 时间 肾盂前后径 输尿管最大径 术前 2.68±0.75 2.85±0.65 术后12个月 0.95±0.35 0.75±0.21 t 16.8 18.4 P值 < 0.01 < 0.01 -
[1] 中华医学会小儿外科学分会小儿泌尿外科学组. 儿童原发性梗阻性巨输尿管症诊疗专家共识[J]. 中华小儿外科杂志, 2022, 43(8): 679-684. doi: 10.3760/cma.j.cn421158-20220402-00233
[2] Konheim JA, Khaled DT, Canter DJ. Ileocalicostomy ureteral substitution for complex ureteropelvic junction stricture: technique and initial experience[J]. Urology, 2018, 122: 174-178. doi: 10.1016/j.urology.2018.08.024
[3] Yeung CK, Sihoe JD, Borzi PA. Endoscopic cross-trigonal ureteral reimplantation under carbon dioxide bladder insufflation: a novel technique[J]. J Endourol, 2005, 19(3): 295-299. doi: 10.1089/end.2005.19.295
[4] 徐延波, 陈海琛, 马丽丽, 等. 气膀胱下Politano-Leadbetter输尿管移植术的经验分析[J]. 临床小儿外科杂志, 2020, 19(8): 741-745, 758. doi: 10.3969/j.issn.1671-6353.2020.08.015
[5] Winfield HN, Donovan JF, See WA, et al. Urological laparoscopic surgery[J]. J Urol, 1991, 146(4): 941-948. doi: 10.1016/S0022-5347(17)37970-3
[6] 朱炜玮, 周辉霞, 李品, 等. 机器人辅助腹腔镜Lich-Gregoir输尿管再植术与气膀胱Cohen输尿管再植术治疗原发性膀胱输尿管反流的疗效对比[J]. 临床小儿外科杂志, 2022, 21(5): 437-444.
[7] 张旭辉, 王计文, 李龙, 等. 气膀胱腹腔镜Cohen输尿管移植术治疗先天性膀胱输尿管连接部梗阻[J]. 临床小儿外科杂志, 2010, 9(3): 182-183.
[8] Kurtz MP, Nelson CP. Urology mythbusters: the 5: 1 ratio in ureteral reimplantation[J]. J Pediatr Urol, 2017, 13(2): 187-188.
[9] Emiliani E, Talso M, Audouin M, et al. Modern flexible ureteroscopy in Cohen cross-trigonal ureteral reimplantations[J]. J Pediatr Urol, 2017, 13(3): 329-331. doi: 10.1016/j.jpurol.2017.03.009
[10] Krambeck AE, Gettman MT, BaniHani AH, et al. Management of nephrolithiasis after Cohen cross-trigonal and Glenn-Anderson advancement ureteroneocystostomy[J]. J Urol, 2007, 177(1): 174-178. doi: 10.1016/j.juro.2006.08.112
[11] Liu X, Liu JH, Zhang DY, et al. Retrospective study to determine the short-term outcomes of a modified pneumovesical Glenn-Anderson procedure for treating primary obstructing megaureter[J]. J Pediatr Urol, 2015, 11(5): 266. e1-6. doi: 10.1016/j.jpurol.2015.03.020
[12] Chung MS, Han SW, Jung HJ, et al. Transvesicoscopic ureteral reimplantation in children with bilateral vesicoureteral reflux: surgical technique and results[J]. J Laparoendosc Adv Surg Tech A, 2012, 22(3): 295-300. doi: 10.1089/lap.2011.0318
[13] 曾莉, 黄一东, 康磊, 等. 改良Politano-Leadbetter术治疗儿童原发性输尿管膀胱连接处异常[J]. 中国修复重建外科杂志, 2015, 29(10): 1279-1283. doi: 10.7507/1002-1892.20150277
[14] Soh S, Kobori Y, Shin T, et al. Transvesicoscopic ureteral reimplantation: Politano-Leadbetter versus Cohen technique[J]. Int J Urol, 2015, 22(4): 394-399.
[15] 吴永隆, 陈海琛, 胡杨, 等. 气膀胱下Politano-Leadbetter术治疗小儿膀胱输尿管连接部异常的临床疗效分析[J]. 临床泌尿外科杂志, 2023, 38(3): 179-183. https://lcmw.whuhzzs.com/article/doi/10.13201/j.issn.1001-1420.2023.03.005
-




 下载:
下载: