-
摘要: 目的 探讨前列腺癌根治性剜除术应用于局限期前列腺癌的可行性。方法 收集2023年12月—2024年3月于华中科技大学同济医学院附属同济医院就诊的局限期前列腺癌患者,筛选入组的患者均前列腺特异性抗原(prostate-specific antigen,PSA) < 20 ng/mL,且由单一术者完成前列腺癌根治性剜除术。排除临床诊断分期≥T3期、难以耐受全身麻醉手术或拒绝该术式的患者。10例入组患者的中位年龄71岁,中位体重指数25 kg/m2,中位Gleason评分3+4=7分。前列腺癌根治性剜除术在Hood技术保护耻骨后和前列腺尖部附近结构的基础上,借鉴后入路根治性前列腺切除术在筋膜内层面探查和前列腺颈部神经血管束保护中的优势,前入路离断膀胱颈主体后迅速自前列腺背侧进入筋膜内层面、逆行松解神经血管束。结果 从切开皮肤至完成皮肤缝合的中位时间为109 min,中位出血量为80 mL;切缘阳性率为20%,术后6周90%的患者PSA < 0.2 ng/mL;即刻尿控率达60%;中位随访4个月时勃起功能保留率为86%(6/7)。结论 前列腺癌根治性剜除术在即刻尿控和勃起功能保留方面效果理想,入路和步骤清晰简明,值得临床上参考应用。Abstract: Objective To investigate the feasibility of radical enucleation of prostate cancer in the application of localized prostate cancer.Methods From December 2023 to March 2024, 10 patients with localized prostate cancer with prostate-specific antigen(PSA) < 20 ng/mL were screened and enrolled in Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, with a median age of 71 years, a median body mass index of 25 kg/m2, and a median Gleason score of 3+4=7. On the basis of Hood technology to protect the structures behind the pubic bone and near the apex of the prostate, radical enucleation of prostate cancer draws on the advantages of posterior radical prostatectomy in the exploration of the intrafascial layer and the protection of the neurovascular bundle in the neck of the prostate.Results The median time from skin incision to skin closure was 109 minutes, and the median blood loss was 80 mL. The positive rate of resection margin was 20%, and PSA < 0.2 ng/mL was found in 90% of patients 6 weeks after surgery. Immediate urinary continence rate was 60%, and erectile preservation rates at median follow-up of 4 months were 86% (6/7).Conclusion Radical enucleation of prostate cancer has ideal effect in immediate urinary continence and sexual function preservation, and the approach and steps are clear and concise, which is worthy of clinical reference and application.
-
Key words:
- localized prostate cancer /
- radical prostatectomy /
- intrafascial /
- enucleation /
- functional protection
-

-
表 1 患者基线资料和手术相关指标
例序 年龄/岁 PSA/ (ng/mL) 体积/mL PIRADS评分 穿刺GG cT 手术时间/min 根治术GG pT 切缘 术后6周PSA/ (ng/mL) 尿控恢复时间 术前IIEF-5 ≥17分 术后IIEF-5 ≥17分 1 73 5.6 32 4 2 2a 94 2 2a 阴性 0.05 3 d 是 否 2 68 10.3 38 4 5 2a 110 4 3b 阴性 0.19 3个月 是 是 3 75 13.0 85 3 3 2a 109 2 2a 阴性 0.01 当天 是 是 4 69 14.5 100 5 3 2c 128 5 2c 阴性 0.40 当天 是 是 5 70 15.6 24 2 2 2a 105 3 2a 阴性 0.03 1周 否 否 6 68 10.1 30 5 2 2a 137 2 2a 阴性 0.01 4周 否 否 7 76 12.4 26 5 5 2a 103 4 3b 阳性 0.18 1周 是 是 8 70 18.3 50 5 1 2a 119 1 2a 阴性 0.05 1周 否 否 9 73 9.9 27 5 2 2b 117 2 2b 阳性 0.05 4周 是 是 10 72 11.2 38 4 1 2a 97 2 2a 阴性 0.01 4周 是 是 注:手术时间指从切开皮肤至完成皮肤缝合的时间;GG(Grade Group)指前列腺癌病理的ISUP预后分级分组系统;cT指临床T分期;pT指病理T分期;IIEF-5指国际勃起功能指数问卷表-5。 -
[1] Bray F, Laversanne M, Sung H, et al. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries[J]. CA Cancer J Clin, 2024, 74(3): 229-263. doi: 10.3322/caac.21834
[2] Huang Q, Zi H, Luo LS, et al. Secular trends of morbidity and mortality of prostate, bladder, and kidney cancers in China, 1990 to 2019 and their predictions to 2030[J]. BMC Cancer, 2022, 22(1): 1164. doi: 10.1186/s12885-022-10244-9
[3] Qi JL, Li ML, Wang LJ, et al. National and subnational trends in cancer burden in China, 2005-20: an analysis of national mortality surveillance data[J]. Lancet Public Health, 2023, 8(12): e943-e955. doi: 10.1016/S2468-2667(23)00211-6
[4] Mian AH, Tollefson MK, Shah P, et al. Navigating now and next: recent advances and future horizons in robotic radical prostatectomy[J]. J Clin Med, 2024, 13(2): 359. doi: 10.3390/jcm13020359
[5] Axén E, Godtman RA, Bjartell A, et al. Degree of preservation of neurovascular bundles in radical prostatectomy and recurrence of prostate cancer[J]. Eur Urol Open Sci, 2021, 30: 25-33. doi: 10.1016/j.euros.2021.06.005
[6] Wagaskar VG, Mittal A, Sobotka S, et al. Hood technique for robotic radical prostatectomy-preserving periurethral anatomical structures in the space of retzius and sparing the pouch of Douglas, enabling early return of continence without compromising surgical margin rates[J]. Eur Urol, 2021, 80(2): 213-221. doi: 10.1016/j.eururo.2020.09.044
[7] Egan J, Marhamati S, Carvalho FLF, et al. Retzius-sparing robot-assisted radical prostatectomy leads to durable improvement in urinary function and quality of life versus standard robot-assisted radical prostatectomy without compromise on oncologic efficacy: single-surgeon series and step-by-step guide[J]. Eur Urol, 2021, 79(6): 839-857. doi: 10.1016/j.eururo.2020.05.010
[8] Lenfant L, Garisto J, Sawczyn G, et al. Robot-assisted radical prostatectomy using single-port perineal approach: technique and single-surgeon matched-paired comparative outcomes[J]. Eur Urol, 2021, 79(3): 384-392. doi: 10.1016/j.eururo.2020.12.013
[9] Galfano A, Ascione A, Grimaldi S, et al. A new anatomic approach for robot-assisted laparoscopic prostatectomy: a feasibility study for completely intrafascial surgery[J]. Eur Urol, 2010, 58(3): 457-461. doi: 10.1016/j.eururo.2010.06.008
[10] Gao X, Pang J, Si-tu J, et al. Single-port transvesical laparoscopic radical prostatectomy for organ-confined prostate cancer: technique and outcomes[J]. BJU Int, 2013, 112(7): 944-952. doi: 10.1111/bju.12225
[11] Zhou XC, Fu B, Zhang C, et al. Transvesical robot-assisted radical prostatectomy: initial experience and surgical outcomes[J]. BJU Int, 2020, 126(2): 300-308. doi: 10.1111/bju.15111
[12] Sievert KD, Hennenlotter J, Dillenburg T, et al. Extended periprostatic nerve distributions on the prostate surface confirmed using diffusion tensor imaging[J]. BJU Int, 2019, 123(6): 995-1004. doi: 10.1111/bju.14508
[13] Patel VR, Schatloff O, Chauhan S, et al. The role of the prostatic vasculature as a landmark for nerve sparing during robot-assisted radical prostatectomy[J]. Eur Urol, 2012, 61(3): 571-576. doi: 10.1016/j.eururo.2011.12.047
-

| 引用本文: | 杨春光, 杨俊, 李凡, 等. 前列腺癌根治性剜除术的初步探索[J]. 临床泌尿外科杂志, 2024, 39(8): 664-667. doi: 10.13201/j.issn.1001-1420.2024.08.002 |
| Citation: | YANG Chunguang, YANG Jun, LI Fan, et al. Preliminary exploration of radical enucleation for prostate cancer[J]. J Clin Urol, 2024, 39(8): 664-667. doi: 10.13201/j.issn.1001-1420.2024.08.002 |
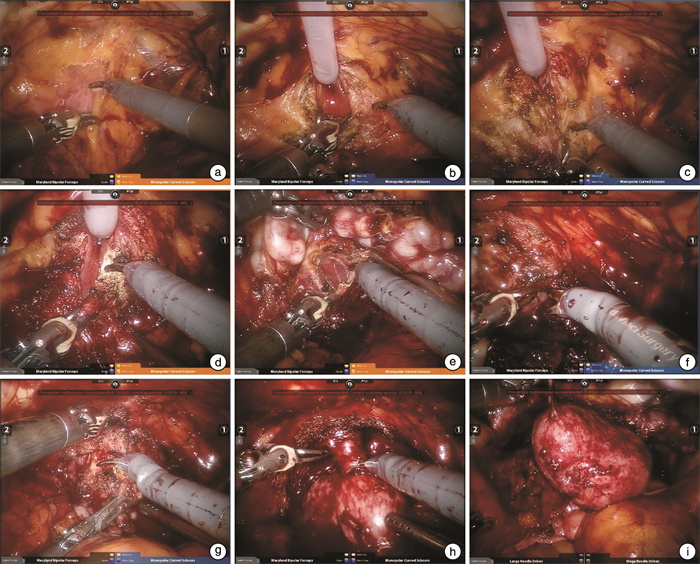
- Figure 1.



 下载:
下载: