Comparative study on transperineal mpMRI-ultrasound imaging fusion-guided prostate biopsy versus transrectal cognitive fusion prostate biopsy
-
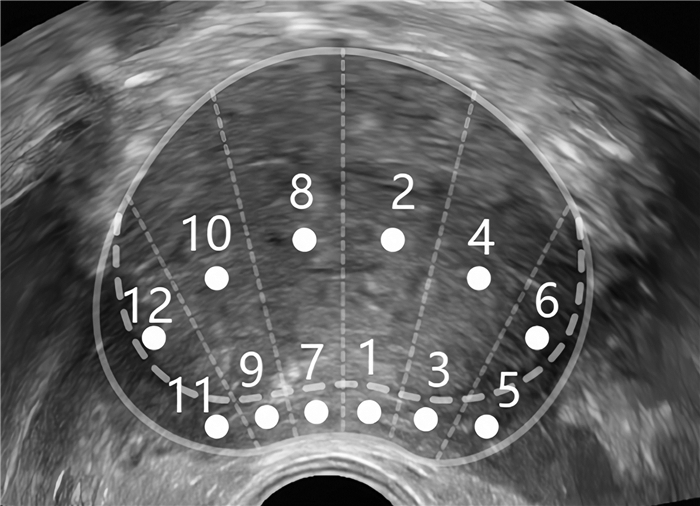
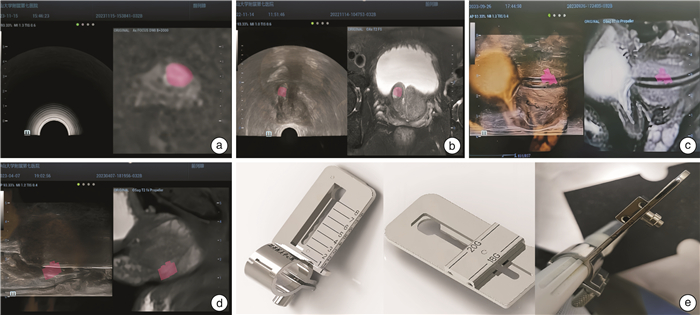
摘要: 目的 对比研究经会阴多参数磁共振(multiparametric magnetic resonance imaging,mpMRI)-超声图像融合前列腺穿刺活检术与经直肠认知融合前列腺穿刺活检术的诊断价值和安全性。方法 回顾性分析2022年1月—2024年1月于中山大学附属第七医院泌尿外科住院行前列腺穿刺活检术的184例患者临床资料,将其中行经会阴mpMRI-超声图像融合前列腺穿刺术的68例作为病例组,行经直肠认知融合前列腺穿刺术的116例作为对照组,2组患者均为靶向穿刺1~3针后行12针系统穿刺。比较2组患者一般临床资料、前列腺癌(prostate cancer,PCa)检出率、临床显著性前列腺癌(clinical significant prostate cancer,csPCa)检出率及并发症发生情况。结果 2组一般临床资料比较差异无统计学意义。病例组靶向穿刺PCa检出率和csPCa检出率(42.65%、36.76%)均显著高于对照组(27.59%、22.41%)。2组总体穿刺(靶向+系统)PCa检出率和csPCa检出率差异均无统计学意义。病例组的并发症发生率(10.29%)显著低于对照组(23.28%)。结论 经会阴mpMRI-超声图像融合前列腺穿刺活检术较经直肠认知融合前列腺穿刺活检术可进一步提高靶向穿刺的准确度,且具有更好的安全性。目前靶向穿刺联合系统穿刺可能是前列腺穿刺活检更好的方案。Abstract: Objective To comparatively investigate the diagnostic value and safety between transperineal multiparametric magnetic resonance imaging(mpMRI) -ultrasound imaging fusion-guided prostate biopsy and transrectal cognitive fusion prostate biopsy.Methods A retrospective analysis was conducted on prostate biopsy 184 patients admitted to the Department of Urology, Seventh Affiliated Hospital of Sun Yat-sen University, from January 2022 to January 2024. Among them, 68 patients who underwent transperineal mpMRI-ultrasound imaging fusion-guided prostate biopsy were designated as the case group, and 116 patients who underwent transrectal cognitive fusion prostate biopsy were designated as the control group. Both groups underwent targeted biopsy with 1-3 needles followed by a systematic 12-needle biopsy. The general clinical data, prostate cancer(PCa) detection rate, clinically significant prostate cancer(csPCa) detection rate, and complication occurrence were compared between the two groups.Results No significant differences were observed in the general clinical data between the two groups. The PCa and csPCa detection rates(42.65%, 36.76%) of targeted biopsy in the case group were both significantly higher than those in the control group(27.59%, 22.41%). However, no statistically significant differences were found in the overall(targeted+systematic biopsy) PCa and csPCa detection rates between the two groups. The complication rate in the case group(10.29%) was significantly lower than that in the control group(23.28%).Conclusion Transperineal mpMRI-ultrasound imaging fusion-guided prostate biopsy can further improve the accuracy of targeted biopsy and demonstrate better safety compared to transrectal cognitive fusion prostate biopsy. Targeted biopsy combined with systematic biopsy may be a better strategy for prostate biopsy.
-

-
表 1 2组患者一般临床资料比较
例(%),X±S 指标 病例组(68例) 对照组(116例) t/χ2 P值 年龄/岁 68.19±10.94 70.65±10.02 -1.518 0.131 前列腺体积/mL 44.32±15.85 45.08±17.64 -0.301 0.764 tPSA/(ng/mL) 12.62±10.38 11.78±13.20 0.469 0.640 PI-RADS≥3分结节/个 1.23±0.95 1.19±1.03 0.267 0.790 PI-RADS评分 0.265 0.607 3分 29(42.6) 45(38.8) 4~5分 39(57.4) 71(61.2) 靶向穿刺针数/针 2.13±1.18 2.06±1.26 0.379 0.705 表 2 2组患者穿刺病理结果比较
例(%) 组别 例数 总体结果(靶向+系统) 靶向结果 PCa csPCa PCa csPCa 病例组 68 31(45.59) 26(38.24) 29(42.65) 25(36.76) 对照组 116 52(44.83) 43(37.07) 32(27.59) 26(22.41) χ2 0.01 0.03 4.39 4.41 P值 0.92 0.88 0.04 0.04 表 3 2组并发症发生情况比较
例(%) 组别 例数 明显肉眼血尿 发热 尿潴留 穿刺部位疼痛 下尿路刺激症状 出现并发症例数 病例组 68 3(4.41) 1(1.47) 1(1.47) 2(2.94) 2(2.94) 7(10.29) 对照组 116 8(6.90) 9(7.76) 4(3.45) 6(5.17) 5(4.31) 27(23.28) χ2 0.47 3.30 0.63 0.51 0.22 4.80 P值 0.72 0.14 0.74 0.73 0.95 0.03 -
[1] Siegel RL, Giaquinto AN, Jemal A. Cancer statistics, 2024[J]. CA Cancer J Clin, 2024, 74(1): 12-49. doi: 10.3322/caac.21820
[2] Bray F, Laversanne M, Sung H, et al. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries[J]. CA Cancer J Clin, 2024, 74(3): 229-263. doi: 10.3322/caac.21834
[3] Wei WQ, Zeng HM, Zheng RS, et al. Cancer registration in China and its role in cancer prevention and control[J]. Lancet Oncol, 2020, 21(7): e342-e349. doi: 10.1016/S1470-2045(20)30073-5
[4] Sekhoacha M, Riet K, Motloung P, et al. Prostate cancer review: genetics, diagnosis, treatment options, and alternative approaches[J]. Molecules, 2022, 27(17): 5730. doi: 10.3390/molecules27175730
[5] Liu JZ, Dong L, Zhu YJ, et al. Prostate cancer treatment-China's perspective[J]. Cancer Lett, 2022, 550: 215927. doi: 10.1016/j.canlet.2022.215927
[6] Kaplan I, Oldenburg NE, Meskell P, et al. Real time MRI-ultrasound image guided stereotactic prostate biopsy[J]. Magn Reson Imaging, 2002, 20(3): 295-299. doi: 10.1016/S0730-725X(02)00490-3
[7] You CY, Li XH, Du YL, et al. The microultrasound-guided prostate biopsy in detection of prostate cancer: a systematic review and meta-analysis[J]. J Endourol, 2022, 36(3): 394-402. doi: 10.1089/end.2021.0361
[8] 胡隽, 赵晓东, 周昱霖, 等. 人工智能引导影像融合辅助经会阴前列腺穿刺活检临床研究[J]. 中华男科学杂志, 2023, 29(8): 729-735.
[9] Cornford P, van den Bergh RCN, Briers E, et al. EAU-EANM-ESTRO-ESUR-ISUP-SIOG guidelines on prostate cancer-2024 update. part I: screening, diagnosis, and local treatment with curative intent[J]. Eur Urol, 2024, 86(2): 148-163. doi: 10.1016/j.eururo.2024.03.027
[10] Schroeder DW, Foster BR, Young DJ, et al. Targeted biopsy of the prostate[J]. Abdom Radiol(NY), 2024.
[11] Falagario UG, Pellegrino F, Fanelli A, et al. Prostate cancer detection and complications of MRI-targeted prostate biopsy using cognitive registration, software-assisted image fusion or in-bore guidance: a systematic review and meta-analysis of comparative studies[J]. Prostate Cancer Prostatic Dis, 2024.
[12] Wei JT, Barocas D, Carlsson S, et al. Early detection of prostate cancer: AUA/SUO guideline part Ⅱ: considerations for a prostate biopsy[J]. J Urol, 2023, 210(1): 54-63. doi: 10.1097/JU.0000000000003492
[13] Blas L, Shiota M, Tsukahara S, et al. Fusion-targeted biopsy significantly improves prostate cancer detection in biopsy-naïve men[J]. Int J Urol, 2023, 30(7): 600-604. doi: 10.1111/iju.15188
[14] 杨景, 封淏, 夏晗, 等. 对比MRI-经直肠超声软件融合导航穿刺与认知融合导航穿刺检出前列腺癌效果[J]. 中国介入影像与治疗学, 2024, 21(7): 403-407.
[15] 梁健, 何京伟, 关文峰, 等. 多参数MRI与超声认知融合引导下前列腺靶向穿刺的前瞻性研究[J/OL]. 中华腔镜泌尿外科杂志(电子版), 2023, 17(6): 558-562.
[16] 聂军, 罗卫平, 李栋, 等. MRI引导下软件融合与认知融合穿刺活检对PSA < 20 ng/mL患者前列腺癌检出率比较研究[J]. 放射学实践, 2023, 38(10): 1297-1302.
[17] 施云峰, 曹锴, 刘晓武, 等. 认知融合MRI和超声引导靶向穿刺在前列腺前部肿瘤诊断中的临床应用[J]. 临床泌尿外科杂志, 2023, 38(4): 251-254. https://lcmw.whuhzzs.com/article/doi/10.13201/j.issn.1001-1420.2023.04.003
[18] Monda SM, Vetter JM, Andriole GL, et al. Cognitive versus software fusion for MRI-targeted biopsy: experience before and after implementation of fusion[J]. Urology, 2018, 119: 115-120. doi: 10.1016/j.urology.2018.06.011
[19] 黄尚, 毕学成, 李腾, 等. 认知融合及影像融合在前列腺穿刺活检中的应用[J]. 临床泌尿外科杂志, 2020, 35(7): 557-561. https://lcmw.whuhzzs.com/article/doi/10.13201/j.issn.1001-1420.2020.07.010
[20] Marra G, Ploussard G, Futterer J, et al. Controversies in MR targeted biopsy: alone or combined, cognitive versus software-based fusion, transrectal versus transperineal approach?[J]. World J Urol, 2019, 37(2): 277-287. doi: 10.1007/s00345-018-02622-5
-




 下载:
下载: