Application of ureter-lower calyx distance in the treatment of flexible ureteroscopy for less than 2 cm lower pole kidney stones
-
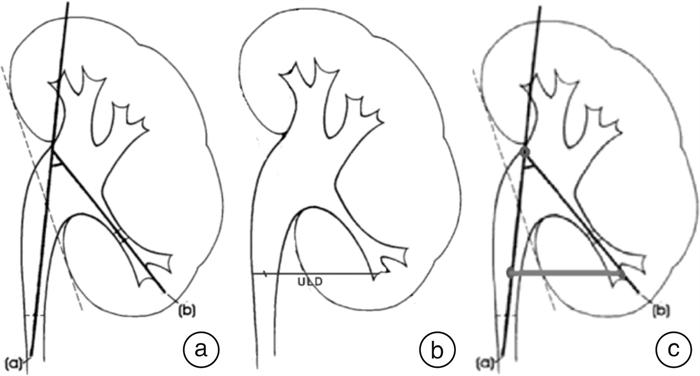
摘要: 目的 探讨一种新的评估方法——输尿管-肾下盏距离(ureter-lower calyx distance,ULD)在肾下盏结石患者中的运用效果。方法 回顾性分析2021年10月—2022年12月华中科技大学同济医学院附属协和医院泌尿外科收治的126例肾下盏结石患者的临床资料。所有患者均行输尿管软镜处理肾下盏结石。分析分别采用肾盂漏斗部夹角(infundibulopelvic angle,IPA)分组与ULD分组比较患者手术时间和术后清石率的差异。结果 以IPA进行分组,分为IPA>30°组和IPA≤30°组,2组手术时间和清石率比较差异有统计学有意义(P < 0.05);以ULD进行分组,分为ULD>3 cm组和ULD≤3 cm组,2组手术时间和清石率比较差异有统计学意义(P < 0.05)。IPA>30°组与ULD>3 cm组手术时间和清石率比较差异无统计学意义。结论 ULD作为一种全新的输尿管软镜术前评估指标,较IPA更方便简单,实用性强,值得在临床进一步推广。Abstract: Objective To investigate the effect of a new evaluation method: ureter-lower calyx distance (ULD) in patients with lower pole kidney stones.Methods The data of 126 patients with lower pole kidney stones treated from October 2021 to December 2022 were retrospectively analyzed. All patients were treated by flexible ureteroscopy. The differences in operative time and postoperative stone free rate between infundibulopelvic angle (IPA) group and ULD group were analyzed.Results IPA was divided into IPA > 30° group and IPA≤30° group, and there were significant differences in operation time and postoperative stone free rate between the two groups. ULD was divided into ULD > 3 cm group and ULD≤3 cm group, and there were significant differences in operation time and postoperative stone free rate between the two groups. However, there was no significant difference between the IPA > 30° group and ULD > 3 cm group in operation time or postoperative stone free rate.Conclusion ULD as a new preoperative evaluation index of flexible ureteroscopy is more convenient, simple and practical than IPA, so it's worthy of further promotion in clinic.
-

-
表 1 患者一般资料
例(%),X±S 项目 数值 年龄/岁 51.2±11.4 性别 男 75(59.52) 女 51(40.48) 主要结石分布 左肾下盏 68(53.97) 右肾下盏 58(46.03) 结石直径/cm 1.56±0.33 一期置管 是 24(19.05) 否 102(80.95) 总清石率 111(88.10) -
[1] Ye Z, Zeng G, Yang H, et al. The status and characteristics of urinary stone composition in China[J]. BJU Int, 2020, 125(6): 801-809. doi: 10.1111/bju.14765
[2] 赵志健, 曾国华. 《2021 EULIS与IAU联合专家共识: 输尿管软镜碎石术》解读[J]. 临床泌尿外科杂志, 2022, 37(2): 83-85. https://lcmw.whuhzzs.com/article/doi/10.13201/j.issn.1001-1420.2022.02.001
[3] Kallidonis P, Ntasiotis P, Somani B, et al. Systematic Review and Meta-Analysis Comparing Percutaneous Nephrolithotomy, Retrograde Intrarenal Surgery and Shock Wave Lithotripsy for Lower Pole Renal Stones Less Than 2 cm in Maximum Diameter[J]. J Urol, 2020, 204(3): 427-433. doi: 10.1097/JU.0000000000001013
[4] Tastemur S, Senel S, Kizilkan Y, et al. Evaluation of the anatomical factors affecting the success of retrograde intrarenal surgery for isolated lower pole kidney stones[J]. Urolithiasis, 2022, 50(1): 65-70. doi: 10.1007/s00240-021-01279-x
[5] Inoue T, Murota T, Okada S, et al. Influence of Pelvicaliceal Anatomy on Stone Clearance After Flexible Ureteroscopy and Holmium Laser Lithotripsy for Large Renal Stones[J]. J Endourol, 2015, 29(9): 998-1005. doi: 10.1089/end.2015.0071
[6] Jessen JP, Honeck P, Knoll T, et al. Flexible ureterorenoscopy for lower pole stones: influence of the collecting system's anatomy[J]. J Endourol, 2014, 28(2): 146-151. doi: 10.1089/end.2013.0401
[7] Elbahnasy AM, Clayman RV, Shalhav AL, et al. Lower-pole caliceal stone clearance after shockwave lithotripsy, percutaneous nephrolithotomy, and flexible ureteroscopy: impact of radiographic spatial anatomy[J]. J Endourol, 1998, 12(2): 113-119. doi: 10.1089/end.1998.12.113
[8] 中华医学会泌尿外科分会, 中国泌尿系结石联盟. 软性输尿管镜术中国专家共识[J]. 中华泌尿外科杂志, 2016, 37(8): 561-565. doi: 10.3760/cma.j.issn.1600-6702.2016.08.001
[9] 徐汉江, 郝宗耀, 曾国华. 肾下盏解剖结构对输尿管软镜碎石术疗效影响的研究进展[J]. 临床泌尿外科杂志, 2018, 33(2): 129-131. https://www.cnki.com.cn/Article/CJFDTOTAL-LCMW201802014.htm
[10] 曾佩, 刘莹, 不同肾盂漏斗部夹角肾下盏结石患者采用不同术式的疗效及疗效相关因素分析[J]. 临床泌尿外科杂志, 2022, 30(1): 78-81. https://www.cnki.com.cn/Article/CJFDTOTAL-LCWK202201026.htm
-




 下载:
下载: